To the Editor:
Patent foramen ovale (PFO) is frequent in adults (prevalence of 25% in the general public) and there are numerous cases described that display the relation between this entity and different medical profiles.1
We present the case of a patient who suffered abrupt intraoperative desaturation followed by refractory hypoxaemia with echocardiographic evidence of a right-to-left shunt through the foramen ovale, previously unknown.
Seventy-seven year old female, obese and with hypertension, admitted for surgery on a 6 cm abdominal aortic aneurysm. Cardiopulmonary auscultation, electrocardiogram and spirometry were normal. The chest x-ray displayed a slight elevation of both hemidiaphragms.
The intervention consisted of a resection of the aneurysm and insertion of Dacron prosthesis. During the procedure, there was severe haemorrhaging which required a transfusion of four units of packed red blood cells and a drop in oxygen saturation to 72%, with a decrease in exhaled CO2. No electrocardiographic changes were detected. Arterial gasometry was extracted: pH, 7.52; pCO2, 28; pO2, 49; Sat, 88%; haematocrit, 28%; D-dimer, 2920. With FiO2 at 0.7 a pO2 of 54 mm Hg was obtained on leaving the operating theatre. Pulmonary auscultation and x-ray were normal.
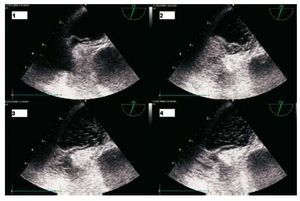
An urgent transoesophageal echocardiogram was requested which displayed a large PFO with bubbles passing immediately through it (Figure). The right cavities were not dilated, right ventricular function normal and no significant tricuspid insufficiency was observed, excluding pulmonary embolism as a cause of the hypoxaemia.2
Figure.Transoesophageal echocardiogram after administering saline serum. 1: during inspiration of the mechanical ventilation, the septum primum moves up to 6 mm. 2: the bubbles reach the left atrium through the foramen. 3: during expiration, the septum primum draws near. 4: the bubbles immediately reach the left atrium in a large number (more than 50).
Ventilation was maintained in volume-control mode (FiO2, 0.7; PEEP, 5) with an oxygen saturation of 90% and PEEP was suspended after the echocardiogram. Her FiO2 was subsequently reduced to 0.5 with 99% saturation.
She was discharged from the hospital after a favourable evolution in the ward. Percutaneous closing of the PFO was ruled out and antiplatelet drug treatment was decided on as a preventative measure in the face of the size of the foramen and the presence of a predisposition to venous thrombosis.
PFO is normally an alteration with no clinical repercussion; although, cases of hypoxaemia and embolic phenomenon in circumstances in which the right atrium pressure exceeds the left have been described.3 This difference in pressure is frequent during the perioperative stage. Some situations which favour it are anatomical, such as horizontalisation of the heart directing the flow of the inferior vena cava towards the PFO (in diaphragmatic paralysis), and others by an increase in pressure of the right cavities, such as pulmonary thromboembolism, tamponade, right ventricle infarction or severe tricuspid insufficiency.3 Mechanical ventilation in these patients is complex. The hypoxaemia does not respond to increases in positive end-expiratory pressure (PEEP) which has even been related to the shunt increase.4 Also, patient maladjustment during weaning which involves a manoeuvre similar to that of Valsalva increases the shunt and consequently the hypoxaemia, which hinders extubation.3
In our patient, the decompression of the left cavities due to massive intraoperative arterial blood loss, mechanical ventilation and PEEP, and diaphragmatic elevation were probable mechanisms of hypoxaemia in the intraoperative and immediate postoperative periods.
It is essential to keep this manifestation of the PFO in mind in cases of intraoperative or perioperative hypoxaemia. With these clinical symptoms, the transoesophageal echocardiogram can exclude, without having to move the patient, a significative pulmonary embolism or a PFO.
The position faced with a PFO shunt in the perioperative stage should be the correction of the precipitant situation if possible. Nitric oxide decreases the shunt3 by reducing pressure in the pulmonary tree and PEEP should be avoided.4 Percutaneous closing is a disputable subject.3 Besides the indications of paradoxical embolism, cases of closing in patients with chronic5 or acute refractory6 hypoxaemia have been described. The evolution of our patient was favourable without percutaneous closing and there is currently no indication of its use to avoid similar occurrences.