We present the characteristics and outcomes of heart transplantation in Spain since it was first performed in 1984.
MethodsA descriptive analysis of the characteristics of recipients, donors, the surgical procedure, and the outcomes of heart transplantations performed in Spain until 31 December 2014.
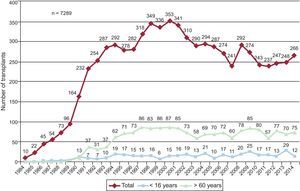
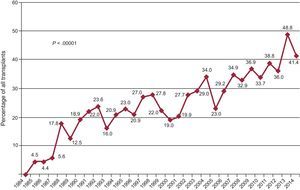
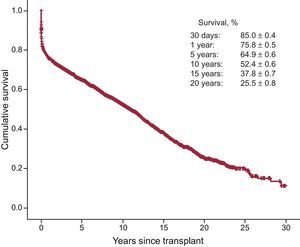
ResultsIn 2014, 266 procedures were performed, making a time series of 7289 transplantations. The temporal analysis confirmed a significant worsening of the clinical profile of recipients (higher percentage of older patients, patients with severe renal failure, insulin-dependent diabetes, previous cardiac surgery, and previous mechanical ventilation), of donors (higher percentage of older donors and greater weight mismatch), and of the procedure (higher percentage of emergency transplantations, reaching 41.4% in 2014, and ischemia time>240min). Mechanical assist devices were used less than in 2013; in 2014 they were used in 18.8% of all transplant recipients. Survival at 1, 5, 10, and 15 years was 76%, 65%, 52%, and 38%, respectively, and has remained stable since 1995.
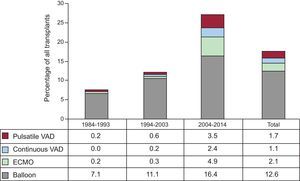
ConclusionsCardiac transplantation activity in Spain has remained stable in recent years, at around 250 procedures per year. Despite a clear deterioration in donor and recipient characteristics and surgical times, the mortality outcomes have remained comparable to those of previous periods in our environment. The growing use of circulatory assist devices before transplantation is also confirmed.
Keywords
Since 1991, the Spanish Heart Transplantation Registry has published reports of the clinical and surgical characteristics and the overall results of cardiac transplant procedures performed in Spain.1-25 This article describes the data on the transplant population to 31 December 2014. As is already well-known, the greatest strength of the Spanish Heart Transplantation Registry is the inclusion and exhaustive updating of all heart transplant procedures performed in all hospitals in Spain since May 1984, regardless of their characteristics and outcomes. Also, data are collected prospectively in a common database and are agreed upon and updated by all the transplantation groups.
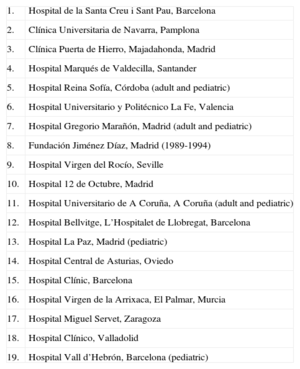
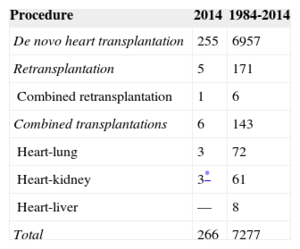
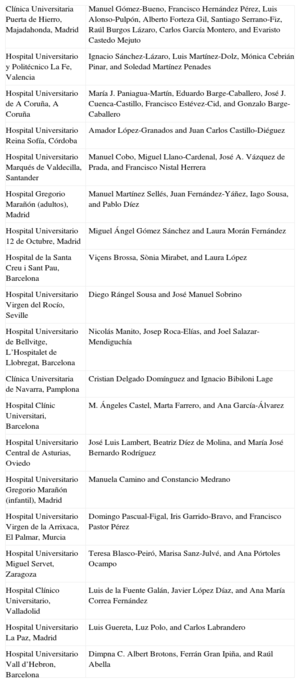
METHODSPatients and CentersNineteen centers contributed data to the Spanish Heart Transplantation Registry, 18 of which are currently still active (Table 1). Two centers are dedicated solely to pediatric transplantation and 3 others perform both adult and pediatric transplantation. The number of procedures performed annually is summarized in Figure 1. The whole series consists of 7289 procedures. Data were lost in 12 cases, including information on follow-up. Those cases were not included in the analysis, and the final sample size was 7277 cases. Of the 266 procedures carried out in 2014, 12 (4.5%) were performed in pediatric patients (age<16 years). The types of procedures carried out in 2014 and in the whole series are summarized in Table 2.
Centers (by Order of First Transplantation Performed) Participating in the Spanish Heart Transplantation Registry (1984-2014)
| 1. | Hospital de la Santa Creu i Sant Pau, Barcelona |
| 2. | Clínica Universitaria de Navarra, Pamplona |
| 3. | Clínica Puerta de Hierro, Majadahonda, Madrid |
| 4. | Hospital Marqués de Valdecilla, Santander |
| 5. | Hospital Reina Sofía, Córdoba (adult and pediatric) |
| 6. | Hospital Universitario y Politécnico La Fe, Valencia |
| 7. | Hospital Gregorio Marañón, Madrid (adult and pediatric) |
| 8. | Fundación Jiménez Díaz, Madrid (1989-1994) |
| 9. | Hospital Virgen del Rocío, Seville |
| 10. | Hospital 12 de Octubre, Madrid |
| 11. | Hospital Universitario de A Coruña, A Coruña (adult and pediatric) |
| 12. | Hospital Bellvitge, L’Hospitalet de Llobregat, Barcelona |
| 13. | Hospital La Paz, Madrid (pediatric) |
| 14. | Hospital Central de Asturias, Oviedo |
| 15. | Hospital Clínic, Barcelona |
| 16. | Hospital Virgen de la Arrixaca, El Palmar, Murcia |
| 17. | Hospital Miguel Servet, Zaragoza |
| 18. | Hospital Clínico, Valladolid |
| 19. | Hospital Vall d’Hebrón, Barcelona (pediatric) |
Spanish Heart Transplantation Registry (1984-2014). Type of Procedure
| Procedure | 2014 | 1984-2014 |
|---|---|---|
| De novo heart transplantation | 255 | 6957 |
| Retransplantation | 5 | 171 |
| Combined retransplantation | 1 | 6 |
| Combined transplantations | 6 | 143 |
| Heart-lung | 3 | 72 |
| Heart-kidney | 3* | 61 |
| Heart-liver | — | 8 |
| Total | 266 | 7277 |
The database comprises 175 clinical variables, pre-established by consensus from all groups, collecting data on the recipient, donor, surgical technique, immunosuppression, and follow-up. As of 2013, data are introduced and updated electronically and in real time using an application available on the internet and specifically designed for this purpose. The database support is a Microsoft Excel file. This method replaces the previous one, in which each center sent data to the registry director in Microsoft Access format via e-mail. An external CRO (contract research organization)—currently ODDS, S.L.—is responsible for database maintenance, quality control, and statistical analysis.
Ethics committee approval, auditing, and registration with the Ministry of Health were carried out in line with the Spanish Organic Law on Data Protection 15/1999.
StatisticsContinuous quantitative variables are reported as mean±standard deviation, and categorical quantitative variables are reported as percentages. Results are organized according to year of transplantation, dividing the total sample into 3 groups (1984-1993, 1994-2003, and 2004-2014). In some variables (such as donor age, emergency transplant, and ischemia time), the data were also analyzed annually for the whole series. Differences between groups were analyzed using a nonparametric test for temporal trends (Kendall's tau) for categorical variables, and analysis of variance with polynomial fit for quantitative variables. Survival curves were calculated using the Kaplan-Meier method, and survival curves were compared with the log rank test. A P value <.05 was considered statistically significant.
RESULTSRecipient CharacteristicsIn 2014, mean recipient age was 50±16 years (0.02-73 years); 75% were men. The most common underlying diagnoses were ischemic cardiomyopathy (25.9%, dilated nonischemic cardiomyopathy (27.8%), cardiomyopathy of valvular origin (4.5%), and other causes (41.7%). Recipient patient characteristics by transplantation period are summarized in Table 3. There were significant trends toward older recipients, female sex, and unusual causes of underlying heart disease. There was an increase in pre-transplant existing conditions known to affect prognosis, such as insulin-dependent diabetes, infection, and cardiac surgery or mechanical ventilation prior to transplantation. Retransplantation frequency remained stable at around 2.4% in the period 1984-2014. In contrast, pulmonary vascular resistance values prior to transplantation were significantly reduced throughout the time series.
Recipient Characteristics in the Spanish Heart Transplantation Registry (1984-2014)
| 1984-1993(n=1230) | 1994-2003(n=3148) | 2004-2014(n=2899) | P (trend) | 2014(n=266) | |
|---|---|---|---|---|---|
| Age, years | 46.7±13.4 | 50.4±14.6 | 49.6±16.5 | <.001 | 49.9±15.8 |
| <16 years | 3.9 | 4.8 | 6.6 | <.001 | 4.5 |
| >60 years | 10.0 | 24.3 | 27.4 | <.001 | 28.2 |
| Sex, male | 85.8 | 81.1 | 76.0 | <.001 | 75.2 |
| BMI | 24.2±4 | 25.0±4.5 | 24.9±4.7 | <.001 | 24.8±4.3 |
| Underlying etiology | <.001 | ||||
| Nonischemic dilated | 39.8 | 34.3 | 27.1 | 27.8 | |
| Ischemic | 30.8 | 30.0 | 26.0 | 25.9 | |
| Valvular | 10.5 | 7.6 | 7.4 | 4.5 | |
| Other | 24.9 | 28.1 | 39.6 | 41.7 | |
| PVR (WU) | 2.6±1.8 | 2.3±1.8 | 2.4±2.1 | <.001 | 2.2±1.3 |
| Creatinine>2 mg/dL | 7.0 | 6.1 | 7.9 | .131 | 5.8 |
| Bilirubin>2 mg/dL | 19.7 | 17.8 | 17.8 | .35 | 16.8 |
| Insulin-dependent diabetes | 8.5 | 12.9 | 17.3 | <.001 | 21.4 |
| Moderate-severe COPD | 9.3 | 11.2 | 9.8 | .109 | 13.7 |
| Previous infection | 4.0 | 9.4 | 13.8 | <.001 | 14.0 |
| Previous cardiac surgery | 25.3 | 26.5 | 29.1 | .024 | 30.1 |
| Heart retransplantation | 2.8 | 2.1 | 2.6 | .84 | 2.3 |
| Mechanical ventilation prior to transplantation | 8.3 | 10.3 | 15.7 | <.001 | 11.7 |
| Emergency transplantation | 18.1 | 23.6 | 35.1 | <.001 | 41.4 |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; PVR, pulmonary vascular resistance.
Values expressed are mean±standard deviation or percentages.
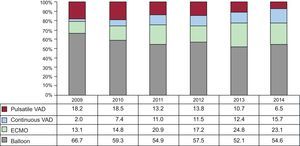
Although fewer emergency transplantations were carried out in 2014 than in 2013, a strongly increasing trend was observed in emergency transplantation over the whole time series (P<.00001) (Figure 2). At the same time, the use of mechanical circulatory assist devices increased (P<.00001) compared with traditional balloon counterpulsation, with mechanical circulatory assist devices coming into use significantly in the last decade (Figure 3). Use of extracorporeal membrane oxygenation (ECMO) and ventricular assist devices–both pulsatile and continuous flow–is particularly evident from 2009 onward (Figure 4). Between 2009 and 2014, the use of ECMO doubled, and that of continuous flow support increased exponentially (from 2.0% in 2009 to 15.7% in 2014).
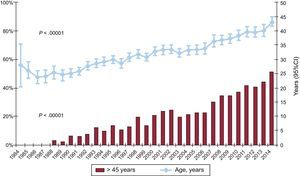
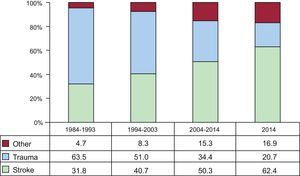
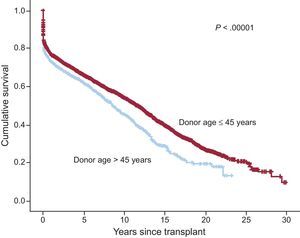
Donor characteristics by time interval and for 2014 are summarized in Table 4. Donor age increased significantly over the whole series, with>50% of donors considered suboptimal (age>45 years) in 2014 (Figure 5). The number of female donors progressively increased, as did the percentage of transplants to a male recipient from a female donor (22.9% in 2014). Increases were also found in cardiac arrest prior to donation (17.4% in 2014), and in ventricular dysfunction on echocardiography prior to extraction (3.3% in 2014). Also, the number of donors who died due to stroke increased, with a decrease in those dying from trauma (Figure 6).
Donor Characteristics and Ischemia Times in the Spanish Heart Transplantation Registry (1984-2014)
| 1984-1993(n=1230) | 1994-2003(n=3148) | 2004-2014(n=2899) | p (trend) | 2014(n=266) | |
|---|---|---|---|---|---|
| Age, years | 26.5±10.3 | 31.3±12.9 | 37.4±14.6 | .067 | 43.6±14.9 |
| Age>45 years | 7.6 | 19.3 | 37.3 | <.001 | 53.8 |
| Sex, male | 78.4 | 70.9 | 65.7 | <.001 | 62.0 |
| Female donor-male recipient | 17.8 | 20.9 | 21.2 | .045 | 22.9 |
| Weight, kg | 69.4±13.4 | 70.1±16.1 | 72.6±18.0 | .007 | 75.0±18.3 |
| Recipient/donor weight | 1.0±0.2 | 1.0±0.3 | 1.0±1.0 | <.001 | 1.0±0.9 |
| Recipient/donor weight>1.20 | 13.3 | 15.8 | 11.1 | <.001 | 9.4 |
| Recipient/donor weight<0.8 | 13.8 | 14.7 | 19.7 | <.001 | 21.1 |
| Pretransplantation cardiac arresta | 3.0 | 7.2 | 11.1 | <.001 | 17.4 |
| Predonation echocardiographyb | <.001 | ||||
| Not done | 52.5 | 21.0 | 6.0 | 1.4 | |
| Normal | 47.1 | 77.7 | 91.4 | 95.3 | |
| Mild generalized dysfunction | 0.3 | 1.2 | 2.7 | 3.3 | |
| Ischemia time, min | 160.8±61.4 | 184.8±61.7 | 205.4±64.3 | .06 | 199.6±72.6 |
| ≤120 min | 27.0 | 18.0 | 11.5 | <.001 | 15.0 |
| 121-180 min | 36.2 | 28.3 | 22.2 | 22.6 | |
| 181-240 min | 28.1 | 36.7 | 38.7 | 35.0 | |
| >240min, % | 8.7 | 17.1 | 27.6 | 27.4 |
Values expressed are mean±standard deviation or percentages.
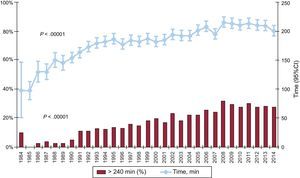
Ischemia time increased over the whole series. In 2014, as in the previous decade, more than one quarter of patients received a transplant with an ischemia time of>240min (Table 4, Figure 7).
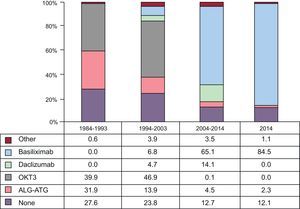
ImmunosuppressionIn 2014, 87.9% of recipients received some type of induction immunosuppressive therapy, mostly basiliximab (84.5%). Figure 8 shows the progressive increase of basiliximab in induction immunosuppression to its current predominant use. In the period 2009-2014, 80% of patients were induced with interleukin-2 inhibitors (basiliximab or daclizumab, primarily basiliximab), replacing the widespread use of OKT3 in earlier periods.
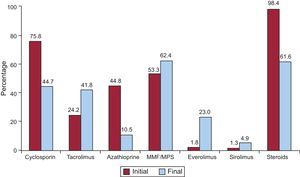
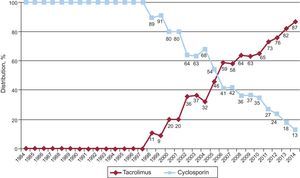
Initial immunosuppression in 2014 was predominantly with tacrolimus (86.7%) as a calcineurin inhibitor, mycophenolate mofetil or mycophenolic acid (96.1%) as an antiproliferative, and steroids (96.9%). Figure 9 shows the immunosuppressors used initially and at the end of follow-up for the whole series. Over an average follow-up of 7 years, 61.6% of patients remained on corticoids. As can be seen, toward the end of follow-up, tacrolimus was used almost as much as cyclosporin, despite the predominant use of cyclosporin in initial immunosuppression regimens. Azathioprine use remains almost anecdotal, and notably, 27.9% of patients were on treatment with mTOR inhibitors (everolimus or sirolimus) at the most recent follow-up.
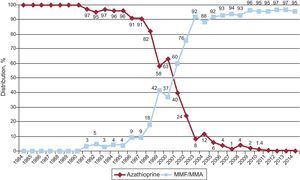
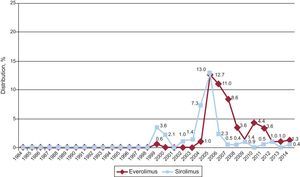
Annual changes in the use of the different calcineurin inhibitors and antimitotics are shown in Figures 10 and 11, respectively. Tacrolimus use equaled cyclosporin use in 2005, and tacrolimus use has continued to increase since then, becoming the most-used calcineurin inhibitor in initial immunosuppression. A similar trend was seen between mycophenolate mofetil and azathioprine, which were used equally between 1999 and 2001, then from 2009 mycophenolate became the predominant antimitotic in initial immunosuppression, with azathioprine being used minimally. The annual changes in the use of mTOR inhibitors (sirolimus, everolimus) in initial immunosuppression are shown in Figure 12. These drugs were used initially at an appreciable percentage between 2005 and 2007; then their use fell to minimal.
Annual changes in use of mTOR inhibitors (sirolimus and everolimus) in initial immunosuppression in the total sample (1984-2014). The differences in values compared with reports from previous years are due to rounding or to differences owing to the continued updating of the database by participating groups.
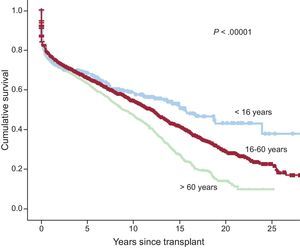
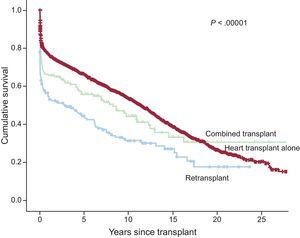
The actuarial survival for the whole series at 1, 5, 10, 15, and 20 years at 31 December 2014 is summarized in Figure 13. This represents an average mortality of approximately 2% to 3% per year after the first post-transplant year, with a median survival of 10.9 years. There were significant differences depending on recipient age at the time of transplantation and the type of procedure. Survival was significantly better in patients younger than 16 years than in those aged 16 to 60 years. Likewise, survival was significantly better in patients aged 16 to 60 years than in those older than 60 years (Figure 14). There were also highly significant differences between heart transplantation alone; combined cardiac and renal, hepatic, or pulmonary transplantation; and retransplantation (Figure 15). Survival was also significantly affected by donor age older than 45 years (Figure 16).
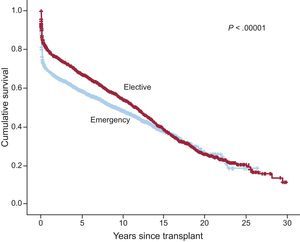
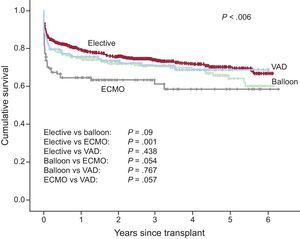
In the whole series, highly significant differences (P<.00001) were found in survival between elective transplantation and emergency transplantation (Figure 17). Analysis of the period 2009-2014, in which use of mechanical assist devices increased appreciably, showed that the worst survival was in emergency transplantations done with ECMO assistance; there were no significant differences between emergency and elective transplantations that used counterpulsation balloon or ventricular assist devices (Figure 18). The differences between the types of transplant according to the condition of the patient at the time of intervention are established over the first 6 months post-transplant, with a subsequent parallel curve pattern.
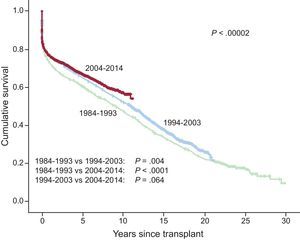
After the first decade (1984-1993), there was a significant improvement in mid-term and long-term survival, influenced mainly by a lower mortality in the early post-transplant stages (Figure 19). Over the last decade (2004-2013), there was a non-significant trend (P=.064) toward improved survival from the third or fourth post-transplant year compared with the decade immediately prior (1994-2003) (Figure 19).
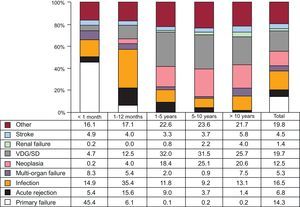
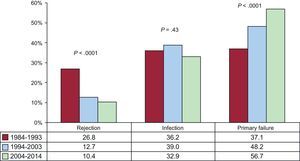
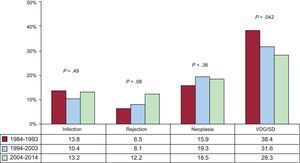
Causes of DeathIn the total population, the most common cause of death was vascular disease of the graft/sudden death (19.7%), followed by infection (16.5%), primary graft failure (14.3%), and neoplasia (12.5%) (Figure 20). Cause of death changed depending on time post-transplant (Figure 20). In the first post-transplant month, almost 50% of deaths were due to primary graft failure. From 1 month to 1 year post-transplant, the most common causes of death were acute rejection (15.6%) and, above all, infection (35.4%). After the first year, the most common causes were the different manifestations of vascular disease of the graft (29.5%), and tumors (21.3%). Over time, the main causes of death in the first year have changed significantly, with more deaths due to primary graft failure and fewer deaths due to acute rejection (Figure 21). However, between the first and fifth years post-transplant, only deaths due to vascular disease of the graft/sudden death have decreased significantly, while deaths due to acute rejection have increased (Figure 22).
Heart transplantation activity in Spain in 2014 has remained stable compared with recent years, after the appreciable reduction at the beginning of the century. The present report confirms the trend in procedure characteristics observed over the past 5 years, we toward recipients with complex clinical profiles, a high proportion of emergency transplantations, a high percentage of suboptimal donors, and relatively long ischemia times. Despite these generally unfavorable circumstances, the mortality outcomes from Spanish teams have remained stable, and we have even started to see a trend toward improved mortality at mid-term follow-up.
Approximately 1 in every 5 transplants in Spain is to a recipient with some sort of circulatory assist device, equally divided between ECMO and circulatory assist devices (pulsatile, or usually continuous). The growing use of circulatory assistance prior to transplantation is a worldwide trend, as shown by data from the registry of the International Society for Heart and Lung Transplantation,26 and has been common practice in Spain since 2009. Our analysis reveals that stabilization of the most severely unwell patients with ventricular assist devices achieves excellent early and mid-term results, close to those obtained in elective transplantation. However, in our series, the prognosis of recipients supported with ECMO was significantly less favorable, a finding similar to other population analyses.27,28 All these findings seem to indicate that use of ECMO is probably more appropriate as a bridge to decision than as a bridge to transplantation, in which case the device should be upgraded to a longer-term device.
Significant changes were also evident in the donor characteristics. In particular, the number of older donors and the proportion of donors considered suboptimal (age>45 years) have increased since the first years of transplantation. In 2014, donor age peaked at a mean age of 44 years, and 54% of donors were suboptimal. This reflects the effort of Spanish teams to offer a clinically effective therapeutic option at a time when donors are relatively scarce and also in worse condition. However, the prognostic effect of such variables must be taken into account when analyzing the outcomes of our programs, especially in the mid- and long-term.
Survival curve analysis shows that despite the increasingly complex clinical circumstances of current transplantations, early mortality remains at a level similar to that of previous periods and is comparable to that reported in the international registry for similar periods.26 It is also noteworthy that in patients who received a transplant in the past decade, from the third or fourth year post-transplant, they have an almost significantly better survival than patients who received a transplant in the decade immediately prior. A cause of death analysis might offer some keys to these findings. In the first post-transplant year, the proportion of deaths due to primary graft failure has increased significantly, which is not surprising given the worse conditions of recipients at the time of transplantation (ongoing widespread use of ECMO as circulatory support instead of ventricular assist devices,29,30 worse hemodynamic status,31 longer ischemia times, and use of suboptimal donors). This increase is compensated, however, by better control of acute severe rejection, which has gone from being the cause of death in 27% in the first decade of the series, to 10% in the most recent decade, without an increase in fatal infections (due to improved diagnosis, prophylaxis, and treatment of infections). In deaths occurring between the first and fifth year, there was a significant reduction in those due to vascular disease of the graft and sudden death (a common manifestation of vascular disease in this post-transplant period). Undoubtedly, Spanish teams practice an aggressive diagnostic strategy toward this serious and limiting post-transplant complication, and above all, implement known effective treatments against this disease, such as the universal use of statins from the time of transplantation in immunosuppressed individuals. In this regard, we must highlight the predominant use of tacrolimus as a calcineurin inhibitor. Tacrolimus has a differential action from that of cyclosporin on microvascular disease and remodeling of epicardial coronary arteries of the graft32 and on the cardiovascular risk profile.33 The same can be said for the use of mycophenolate compared with azathioprine.34 In this regard, the widespread use of mTOR inhibitors (mainly everolimus)35 is particularly relevant, at 28% of patients during follow-up.
CONCLUSIONSCardiac transplantation activity in Spain has remained stable in recent years, with around 250 procedures per year. Despite the worsening and complexity of the current clinical setting (use of suboptimal donors, mechanical circulatory support), Spanish teams have managed to maintain mortality outcomes, with a progressive improvement in mid-term prognosis.
FUNDINGThe Spanish Heart Transplantation Registry is partially funded by an unconditional grant from Novartis.
CONFLICTS OF INTERESTF. González-Vílchez receives remuneration from Roche and Astellas for participating in the follow-up and statistical analysis committee, and for educational papers and presentations; and from Roche, Astellas, and Novartis for travel expenses. A. Villa receives a grant from St. Jude Medical and has received remuneration from St. Jude Medical for educational papers and presentations. J. Segovia has received remuneration from Novartis and Roche for educational papers and presentations.
We acknowledge the statistical support given by ODDS, S.L.
| Clínica Universitaria Puerta de Hierro, Majadahonda, Madrid | Manuel Gómez-Bueno, Francisco Hernández Pérez, Luis Alonso-Pulpón, Alberto Forteza Gil, Santiago Serrano-Fiz, Raúl Burgos Lázaro, Carlos García Montero, and Evaristo Castedo Mejuto |
| Hospital Universitario y Politécnico La Fe, Valencia | Ignacio Sánchez-Lázaro, Luis Martínez-Dolz, Mónica Cebrián Pinar, and Soledad Martínez Penades |
| Hospital Universitario de A Coruña, A Coruña | María J. Paniagua-Martín, Eduardo Barge-Caballero, José J. Cuenca-Castillo, Francisco Estévez-Cid, and Gonzalo Barge-Caballero |
| Hospital Universitario Reina Sofía, Córdoba | Amador López-Granados and Juan Carlos Castillo-Diéguez |
| Hospital Universitario Marqués de Valdecilla, Santander | Manuel Cobo, Miguel Llano-Cardenal, José A. Vázquez de Prada, and Francisco Nistal Herrera |
| Hospital Gregorio Marañón (adultos), Madrid | Manuel Martínez Sellés, Juan Fernández-Yáñez, Iago Sousa, and Pablo Díez |
| Hospital Universitario 12 de Octubre, Madrid | Miguel Ángel Gómez Sánchez and Laura Morán Fernández |
| Hospital de la Santa Creu i Sant Pau, Barcelona | Viçens Brossa, Sònia Mirabet, and Laura López |
| Hospital Universitario Virgen del Rocío, Seville | Diego Rángel Sousa and José Manuel Sobrino |
| Hospital Universitario de Bellvitge, L’Hospitalet de Llobregat, Barcelona | Nicolás Manito, Josep Roca-Elías, and Joel Salazar-Mendiguchía |
| Clínica Universitaria de Navarra, Pamplona | Cristian Delgado Domínguez and Ignacio Bibiloni Lage |
| Hospital Clínic Universitari, Barcelona | M. Ángeles Castel, Marta Farrero, and Ana García-Álvarez |
| Hospital Universitario Central de Asturias, Oviedo | José Luis Lambert, Beatriz Díez de Molina, and María José Bernardo Rodríguez |
| Hospital Universitario Gregorio Marañón (infantil), Madrid | Manuela Camino and Constancio Medrano |
| Hospital Universitario Virgen de la Arrixaca, El Palmar, Murcia | Domingo Pascual-Figal, Iris Garrido-Bravo, and Francisco Pastor Pérez |
| Hospital Universitario Miguel Servet, Zaragoza | Teresa Blasco-Peiró, Marisa Sanz-Julvé, and Ana Pórtoles Ocampo |
| Hospital Clínico Universitario, Valladolid | Luis de la Fuente Galán, Javier López Díaz, and Ana María Correa Fernández |
| Hospital Universitario La Paz, Madrid | Luis Guereta, Luz Polo, and Carlos Labrandero |
| Hospital Universitario Vall d’Hebron, Barcelona | Dimpna C. Albert Brotons, Ferrán Gran Ipiña, and Raúl Abella |