Keywords
INTRODUCTION
This report details findings for 2007 from the Spanish Catheter Ablation Registry. The Registry is coordinated by the Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias.1-6
Catheter ablation of cardiac arrhythmias is extensively covered in the scientific literature, though most of the information available derives from clinical research or controlled registries. Information on the procedures used and outcomes achieved in the general population, where selection bias is not an issue, is scarce. The Catheter Ablation Registry, which is run by the Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias, is one of the few published, large-scale registries which collect and share such information.
Data for the Registry is collected annually from centers around Spain and, although participation is voluntary, the great majority of arrhythmia units in Spain collaborate. The registry therefore provides a highly representative picture of the activity carried out by cardiac interventional electrophysiology units for 2007 in Spain.
METHODS
Data collection was either prospective or retrospective. In the first case, patients were included individually in a database provided by the Registry. Retrospective data collection used a standard questionnaire sent to all interventional electrophysiology laboratories in January 2008. The questionnaire is also available on the Working Group on Electrophysiology and Arrhythmias website (www.arritmias.org). Both methods of data collection were similar to those used in previous registries,1-6 with only minor changes being made to the questionnaires. The secretariat of the Spanish Society of Cardiology ensured that it was impossible for registry managers to identify the participating centers.
Data collected included variables related to the human and technical resources available in arrhythmia units, the different types of ablation procedures performed, and patient socio-demographic variables. The same 10 arrhythmia substrates monitored in previous registries were analyzed. Substrates were: intranodal tachycardia (INT), accessory pathways (AP), atrioventricular node (AVN), focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia related to postmyocardial infarction scarring (VT-AMI), and ventricular tachycardia not related to postmyocardial infarction scarring (VT-NAMI). Variables analyzed in all substrates included number of patients and procedures performed, success rates, type of catheter ablation used, and number and type of complications arising in connection with the procedure, including perioperative death. More specific variables were considered in some of the substrates, such as location of the accessory pathways, location and mechanism of atrial tachycardia, and type of ventricular tachycardia.
As in previous registries, data on human resources only apply to public institutions. Epidemiological variables are only presented for patients included at sites which used prospective data collection.
Again, as in previous registries, the success rate refers to the outcome on termination of the procedure (the acute rate). It therefore only takes into account operating procedures but not clinical follow-up, which means that data on the number of recurrences is lacking. This is particularly relevant for the VT-AMI and AF substrates, in which clinical approach and objectives may differ. For that reason, the acute success / failure rate may vary between laboratories in these substrates and longer term clinical outcomes cannot be extrapolated from results observed during the ablation procedure.
With regard to complications, only those occurring between procedure and discharge were recorded.
Statistical Analysis
Variables are expressed as means (standard deviations). Differences between variables were evaluated using paired or unpaired Student t tests, as appropriate. The χ2 and Fisher's exact test were used to test for differences between categorical variables. Statistical analysis was carried out using SPSS 13.0. A P value less than .05 was considered significant.
RESULTS
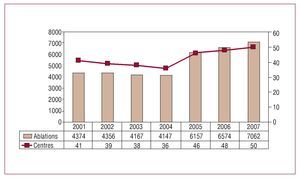
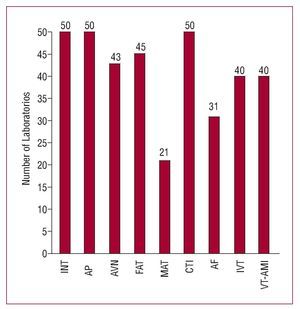
A total of 50 hospitals provided data for the present registry, representing the highest level of participation in the registry's history (Figure 1). The majority of the participating centers were public hospitals (90%). Only 5 (10%) were private. Only 1 of the centers dealt exclusively with pediatric age patients. The great majority of participating centers were tertiary (96%) and teaching (78%) hospitals. A total of 48 (96%) centers were attached to a cardiology department and 41 (82%) had a cardiovascular surgery unit.
Figure 1. Changes in the number of participating institutions and procedures in the Catheter Ablation Registry.
As in previous years, the majority of centers preferred the retrospective system of data collection, with only 8 (16%) centers providing data prospectively.
Epidemiological Characteristics
As in previous years, epidemiological characteristics are only provided for patients included prospectively. This year, that meant 8 centers, which included a total of 1085 patients.
Patients' mean age was 50 (17) years; the youngest were those who received AP ablation (35 [16] years) and the oldest were those treated with AVN ablation (74 [14] years). Intranodal tachycardia ablation had the highest proportion of women (72%), while the highest proportions of men were observed for the AF ablation (81%) and ventricular tachycardia (73%) substrates, with or without structural heart disease. These data are virtually identical to those presented in the previous Registry.
Likewise, 25% of patients had a history of structural heart disease. Left ventricular dysfunction was limited to patients undergoing AVN ablation and ablation for ventricular tachycardia associated with heart disease. The same distribution was seen in patients with an automatic implantable defibrillator.
Infrastructure and Resources
The technical and human resources available in the laboratories participating in the registry are shown in Tables 1 and 2, together with activity for those centers.
Of the total number of centers, 84% had dedicated electrophysiology units, although only 52% of the arrhythmia units were available seven days a week. Two centers had 2 dedicated electrophysiology units.
Pacemakers and defibrillators were implanted in 76% of the units. External electrical cardioversion was performed in 64% of the units and internal cardioversion was carried out in 28%.
As in the previous year, 55% of hospitals still had digital radiology while 45% of the laboratories included had portable fluoroscopy devices. The number of units with at least 1 non-fluoroscopic wapping system (NFMS) continued to increase (80%); 15 centers now had 2 such systems, and 4 centers had 3 systems. In addition, 10 of the electrophysiology laboratories included had intracardiac echocardiography available and, for the first time, 1 center had a remote magnetic navigation system. Cryoablation was performed in 17 (34%) centers, though ultrasound ablation was not available in any of the centers included.
Health care staff dedicated to the electrophysiology laboratories had increased very slightly. In all, 82% of the centers reported having more than one full-time medical doctor and there were more than 2 full-time doctors available in 24% of the centers. In 84% of the centers, there were at least 2 full-time registered nurses.
Overall Results
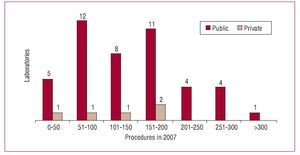
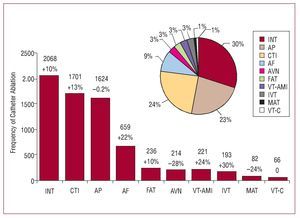
The present registry includes the highest number of reported ablation procedures, with a total of 7062 procedures declared by the 50 participating centers (Figures 1 and 2). This represents an average of 141 (82) ablations per center (median, 129.5; range, 30-470).
Figure 2. Number of electrophysiology laboratories in the National Registry by number of ablation procedures performed during 2007.
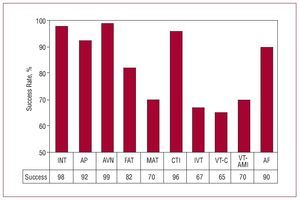
Excluding the AF and VT-AMI substrates, the overall success rate was 92%. A total of 118 complications were reported across all ablation procedures, giving a rate of 1.7%. There were a total of 3 deaths (0.04%), 1 due to a cardiac tamponade during an INT ablation and 2 due to aortic dissection and myocardial infarction during an AP ablation. Two pulmonary thromboembolisms were reported, one during an INT ablation and the other during the epicardial ablation of a VT-AMI. There were 2 cases of catheter entrapment in the mitral valve that required surgical repair. Both occurred during a left AP ablation. The substrate with the highest percentage of complications was AF ablation (5.4%), although there were no fatal complications.
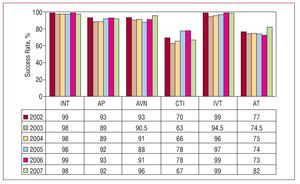
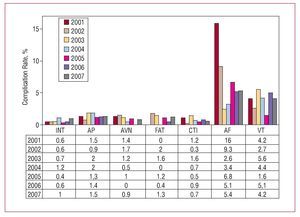
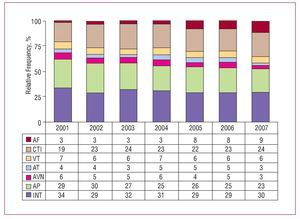
The overall success rates and complication rates are shown in Figure 3. Those rates are compared to data from previous years in Figures 4 and 5.
Figure 3. Changes in catheter ablation success rates by substrate treated, since 2002. AF indicates atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; INT, intranodal tachycardia; VT-C, ventricular tachycardia associated with non-ischemic heart disease; VT-AMI, ventricular tachycardia related to postmyocardial infarction scarring.
Figure 4. Changes in catheter ablation success rates by substrate treated since 2002. AP indicates accessory pathways; AT, atrial tachycardia; AVN, atrioventricular node; CTI, cavotricuspid isthmus; INT, intranodal tachycardia; IVT, idiopathic ventricular tachycardia.
Figure 5. Percentage of major complications associated with catheter ablation by substrate treated, since 2002. AF indicates atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; INT, intranodal tachycardia; VT, ventricular tachycardia.
The most frequently occurring substrate was still INT ablation. This year, and culminating the trend observed in previous years,1-6 CTI became the second most common procedure, ahead of AP ablation (Figure 6). The percentage of AF ablation procedures also increased and accounted for 9.3% of the total number of procedures carried out in 2007. The change in frequency of the different substrates since 2001 is shown in Figure 7.
Figure 6. Relative incidence of different substrates treated by catheter ablation in Spain during 2007. For each substrate, percent change from the previous registry is shown. AF indicates atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; INT, intranodal tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia / atypical atrial flutter; VT-C, heart-disease related ventricular tachycardia; VT-AMI, ventricular tachycardia related to postmyocardial infarction scarring.
Figure 7. Change in relative frequency of different substrates since 2001. AF indicates atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; CTI, cavotricuspid isthmus; INT, intranodal tachycardia; AT, atrial tachycardia; VT, ventricular tachycardia.
As in the previous registry, INT, AP, and CTI ablations were performed in all centers (Figure 8). The number of centers performing AF ablations remained unchanged, at 62% of centers (n=31). The least widely performed ablations were MAT ablations, which were performed in 41% of hospitals.
Figure 8. Number of electrophysiology laboratories participating in the National Registry which treat each of the different substrates. AF indicates atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; INT, intranodal tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia related to postmyocardial infarction scarring.
The following sections show data for specific substrates.
Intranodal Tachycardia
This substrate was treated in all centers. In total, 2068 INT ablations were performed, giving a mean of 41 (24) (range, 3-135) procedures per center. The success rate was identical to the previous year (98.4%). The success rate was 100% in 33 (66%) centers. There were 21 (1%) major complications. Ten (0.5%) of these involved atrioventricular (AV) block requiring implantation of a permanent pacemaker, and t here were 4 cases of pericardial effusion, 3 of complications in vascular access, 1 stroke, 1 pulmonary thromboembolism, 1 pneumothorax, and 1 death (0.05%) resulting from a cardiac tamponade.
A conventional ablation catheter (radiofrequency 4 mm catheter tip) was not suitable in 33 (1.6%) cases: cryoablation was used in 22 cases, an 8 mm tip in 1 case, and an irrigated tip in 10 cases. All ablations in which an irrigated tip was used were carried out at the same center and there were no reports of AV block.
Cavotricuspid Isthmus
Typical atrial flutter was the second most common arrhythmia treated during 2007. Specifically, 1701 CTI ablation procedures were performed (mean, 34 [21] per center), culminating a trend observed in recent years (Figure 7). Success was achieved in 1631 (96%) cases. A total of 22 centers reported a 100% success rate. There were 11 (0.65%) major complications: 5 vascular complications, 3 cases of AV block which required permanent pacemaker implantation, 2 strokes, and 1 case of pulmonary edema.
Non-standard catheters were used in 1603 (94%) procedures. These included 8 mm tip catheters in 991 procedures, irrigated tip catheters in 590 procedures, and 25 cryoablations.
Accessory Pathways
A total of 1624 (mean, 32.5 [19]; interval, 5-92) accessory pathway ablations were performed. The procedure was successful in 1493 (92%) cases. Only 4 centers of the 43 which performed more than 10 accessory pathway ablations in 2007 reported a 100% success rate. There were 25 (1.5%) major complications: 10 vascular complications, 4 (0.25%) AV blocks that required permanent pacemakers, 3 pericardial effusions, 1 myocardial infarction, 1 case of acute pulmonary edema, 1 stroke, and 2 (0.1%) deaths. Deaths were caused by iatrogenic aortic dissection and a massive heart attack (due to an unnoticed application in the coronary artery). During ablation of the left AP, there were 2 cases of entrapment of the catheter in the mitral valve chordae tendineae that required surgical repair: in one case to extract the ablation catheter and in the other case to repair the mitral insufficiency that resulted from a tearing of the chordae tendineae when the catheter was extracted percutaneously.
A conventional ablation catheter was not used in 108 (6.7%) cases: 56 procedures were performed using an irrigated catheter tip, 41 with cryoablation, and 11 with an 8 mm catheter.
The site of the AP ablation was recorded in 1478 cases. As in previous registries, the most frequent sites were the left ventricular free wall (52%) and the inferoparaseptal region (24%). However, this year there was a greater number of right ventricular free wall ablations (15%) than parahisian / supero-paraseptal (9%) ablations. The success of the procedure depended on the location of the AP: the success rate was 96% in the left ventricular free wall, 93% in the right free wall, 90% in the inferoparaseptal region, and 80% in the parahisian / superoparaseptal ablations.
Ablation of the Atrioventricular Node
The total number of procedures was 214, performed in 43 centers. The mean number of procedures per center was lower than in previous years (4 [4]). Success was achieved in 99% of cases and there were only 2 complications, all minor and related to vascular access. A non-conventional ablation catheter was used in 40 cases: irrigated tip catheters were used in 22 procedures and 8 mm catheters in 18.
Focal Atrial Tachycardia
A total of 236 FAT ablations were performed. Forty-two centers performed the procedure when required in the right atrium, but only 20 centers performed it in the left atrium.
The success rate was 82%. The origin of the FAT was reported in 207 cases. Success rates were somewhat higher when FAT originated in the right atrium (81% compared to 71% in the left atrium). There were a total of 3 (1.3%) complications: 2 related to vascular access and 1 stroke.
A non-conventional catheter was used in 37 cases: 8 mm catheters in 4 cases, cryoablation in 8 cases, and an irrigated tip in 25 cases.
Macroreentrant Atrial Tachycardia
A total of 21 (42%) centers performed MAT ablations for a total of 82 procedures (mean, 4 procedures per center; range, 1-19). The procedure was successful in 57 (70.3%) cases. The most noteworthy complication was a stroke.
The origin of the MAT was recorded for 73 procedures, with 37 originating in the right atrium and 36 in the left. Success rates were 83% and 52%, respectively. In 72% of cases, a non-conventional catheter was used: an 8 mm tip was used in 18 procedures and an irrigated tip in 35.
Atrial Fibrillation
A total of 659 (1-98) AF ablations were performed in 31 (62%) of the participating centers. These figures represent a mean of 21.2 procedures per center, although 6 laboratories performed fewer than 5 procedures.
The technique used was recorded for 510 (77%) of the procedures. Ostial pulmonary vein isolation was used in 276 (54.1%) procedures and circumferential ablation in 234 (45.9%). In 15 procedures, the superior vena cava was also electrically disconnected. The 2 approaches achieved an acute success rate of 90.7% and 91.5%, respectively.
Information was available on the ablation catheters used in 462 procedures; an irrigated tip catheter was used in 82% procedures and an 8 mm catheter in the remainder.
There were a total of 36 (5.4%) complications including 21 cases of major pericardial effusion/cardiac tamponade, 4 cases of acute coronary syndrome, 5 complications related to vascular access, 1 acute heart failure, and 5 strokes (although 4 of these were transient).
Idiopathic Ventricular Tachycardia
A total of 193 completed IVT ablation procedures were reported by 40 centers (mean, 4.8 per center; range, 1-15). The procedure was successful in 129 (66.8%) and complications arose in only 4 (2%) cases: 2 cases of tamponade, 1 acute coronary syndrome, and 1 femoral pseudoaneurysm.
The location of the IVT was reported for 166 procedures: 103 occurred in the right ventricular outflow tract, 30 in the left ventricular outflow tract, 25 were fascicular, and 8 referred to "another location." Success rates in the different locations were 76%, 50%, 92%, and 63%, respectively. A 4 mm catheter was used in over 85% of procedures.
Ventricular Tachycardia Associated With Myocardial Infarct Scar
A total of 40 (80%) sites performed 221 VT-AMI ablation procedures (5.5 per center; range, 1-18). There were 11 complications (4.9%): 4 related to vascular access, 2 cardiac tamponades, 2 strokes, and 3 cases of acute heart failure.
The type of ablation was reported in 208 cases: 127 used a conventional technique and 81 used a substrate-based approach. A non-standard catheter was used in 158 (76%) cases: in 73 cases an 8 mm tip was used, and in 85 cases an irrigated tip was used.
The success rate using the conventional approach (clinical tachycardia not inducible after the ablation) was 69.9%. An epicardial approach was used in 3 cases, and was successful in 2.
Ventricular Tachycardia Not Associated With Myocardial Infarction Scarring
Ablation of this substrate was performed 64 times in 24 centers (48%). There were 3 (4.6%) complications: 1 cardiac tamponade, 1 pulmonary edema, and 1 complete AV block.
Success was achieved in 65.6% of procedures. The type of ablations performed were reported as follows: 11 arrhythmogenic right ventricular dysplasias, 10 bundle branch ablations, 18 in non-ischemic dilated cardiomyopathy, and 10 reported as "other." Success rates for the different types of ablation were 82%, 100%, 61%, and 70%, respectively.
In 39% of the procedures, a non-standard catheter was used; in 11 cases, an 8 mm catheter tip was used, and in 14 cases, an irrigated tip.
In 2 patients, an epicardial approach to the arrhythmia was used without achieving success in either case.
DISCUSSION
As in previous years, 2007 saw a progressive increase in the activity of the arrhythmia units included in the registry. Records were set in 2007 both in terms of the number of participating centers (50) and the number of procedures performed, with the figure of 7000 procedures being exceeded for the first time. This makes the data obtained highly representative. On the other hand, the substantial increase in activity contrasts with a correspondingly small increase in human and technical resources. In 2001 (the year of the first Spanish Catheter Ablation Registry), electrophysiology laboratories had a mean of 2.2 (0.6) medical staff and performed 106 (84) procedures per center. In 2007, with 33% more procedures being performed, centers had virtually the same number of medical staff (2.4 [0.6]) (Figure 9 and Table 2). The contrast is even more marked if we consider the increased technical complexity of the procedures performed (especially ablation using non-fluoroscopic navigation and AF) and the use of a wider range of ablation techniques in many laboratories (notably defibrillator implantation and cardiac resynchronization therapy).
Figure 9. Changes in the number of ablation procedures per center.
The distribution of substrates is markedly different from previous registries with 2007 seeing a considerable increase in both the absolute number as well as in the proportion of ablation procedures for typical atrial flutter (TAF). TAF has become the second most frequently treated substrate in electrophysiology laboratories in Spain, thereby confirming an upward trend seen in recent years. For the first time, it has ousted AP ablation as the second most frequently treated substrate. Two factors are likely to have contributed to this change. On the one hand, catheter ablation is increasingly accepted as a first line treatment for TAF on the basis of results from several randomized clinical trials and after its inclusion in clinical practice guidelines.7-9 The change in trend probably also reflects a decrease in the prevalence of AP in the general population due to widespread implementation of a cure for the condition over the last 3 decades.
This edition of the registry has seen a significant increase in the number of laboratories performing AF ablations. While in 2006, only 26 (54%) of the 48 arrhythmia units included in the registry performed this technique, in 2007 the proportion increased to 62%, or 31 of the 50 centers included. Although the number of AF ablations is growing more slowly than might be desirable, the number is rising, making it currently the fourth most common substrate treated in Spanish electrophysiology laboratories and the most widely treated of the "complex" substrates, ahead of MAT or VT-AMI. This year, we have included data on the rate of successful AF ablations, as the omission of this data caused some controversy.10 Nevertheless, these success rates should be interpreted with caution, due to differences in the way acute objectives are de for this procedure (so reported outcomes might vary depending on the way objectives are defined), heterogeneity in the techniques used, and the fact that the relationship between acute success rates and clinical efficacy in the medium or long term is not always linear.11 No less important than the success rates, and probably more illustrative, is the fact that the rate of complications in AF ablations has stabilized at around 5% in recent years. That figure is similar to those published in other AF ablation registries12 and contrasts with earlier editions of the registry (16% in 2001). For many centers, this no doubt reflects rapid progression along the learning curve, which is typical for any new technique.
CONCLUSIONS
The 2007 Spanish Catheter Ablation Registry provides results from one of the largest samples published to date in the international literature on ablation procedures. We now have, for the first time, data on over 7000 procedures obtained from 50 electrophysiology laboratories. The information provided can therefore be considered representative of the activity and outcomes associated with ablation procedures in Spain. The efficacy of the procedure in Spain remains high (92%) with low rates of major complications (1.7%) and deaths (0.04%). The CTI ablation for typical atrial flutter has become the second most frequently treated arrhythmia substrate, behind INT, and there has also been a sustained increase in the number of AF ablation procedures.
ACKNOWLEDGEMENTS
The registry coordinators would like to express their gratitude to all who contributed to the 2007 Ablation Registry by sending data on a voluntary basis and selflessly providing details of their procedures. We would also like to thank Cris-tina Plaza for her excellent administrative work.
ELECTROPHYSIOLOGY LABORATORIES WHO PARTICIPATED IN THE 2007 NATIONAL CATHETER ABLATION REGISTRY BY AUTONOMOUS REGION AND PROVINCE (IN BRACKETS, THE LOCAL CLINICIAN RESPONSIBLE FOR THE REGISTRY)
Andalusia
Cádiz: Hospital Puerta del Mar (Dr L. Cano); Granada: Hospital Virgen de las Nieves (Dr M. Álvarez); Huelva: Hospital Juan Ramón Jiménez (Dr R. Barba); Málaga: Hospital Clínico de Málaga (Dr A. Barrera, Dr J. Alzueta); Sevilla: Hospital Virgen de Macarena (Dr E. Díaz-Infante), Hospital Virgen del Rocío (Dr A. Pedrote), Hospital Virgen de Valme (Dr García Medina).
Aragón
Zaragoza: Hospital Lozano Blesa (Dr G. Rodrigo), Hospital Miguel Servet (Dr A. Asso).
Asturias
Oviedo: Hospital Central de Asturias (Dr N. Pachón).
Balearic Islands
Mallorca: Hospital Son Dureta (Dr M.C. Expósito), Poli-clínica Miramar (Dr N. Alvarenga), Hospital Son Llàtzer (Dr X. Fosch).
Canary Islands
Tenerife: Hospital Nuestra Señora de la Candelaria (Dr R. Romero), Hospital Universitario de Canarias Dr Negrín (Dr E. Arbelo).
Cantabria
Hospital Marqués de Valdecilla (Dr F.J. Rodríguez).
Castilla-La Mancha
Toledo: Hospital Virgen de la Salud (Dr E. Castellanos).
Castilla y León
Burgos: Hospital General Yagüe (Dr J. García); León: Hospital de León (Dr M.L. Fidalgo); Salamanca: Hospital Clínico Universitario (Dr J.L. Moríñigo); Valladolid: Hospital Clínico Universitario (Dr E. García Morán), Hospital del Río Hortega (Dr B. Herreros).
Catalonia
Barcelona: Hospital de Bellvitge (Dr I. Anguera, Dr X. Sabaté), Hospital del Mar (Dr J. Martí), Hospital Clínic (Dr L. Mont), Hospital Vall d'Hebron (Dr A. Moya), Hospital de la Santa Creu i Sant Pau (Dr E. Rodríguez Font), Hospital San Juan de Dios (Dr J. Brugada), Centro Cardiovascular Sant Jordi (Dr J. Brugada), Clínica Sagrada Familia (Dr A. Moya, Dr X. Sabaté).
Valencian Community
Alicante: Hospital Universitario de Alicante (Dr J.G. Martínez); Valencia: Hospital Clínico (Dr A. Martínez), Hospital General (Dr V. Palanca).
Extremadura
Badajoz: Hospital Infanta Cristina (Dr M. Doblado).
Galicia
A Coruña: Hospital Clínico de Santiago de Compostela (Dr J.L. Martínez Sande), Hospital Juan Canalejo (Dr L. Pérez).
Madrid
Hospital Ramón y Cajal (Dr R. Matía); Clínica Puerta de Hierro (Dr I. Fernández Lozano), Hospital 12 de Octubre (Dr R. Salguero), Hospital Clínico San Carlos (Dr N. Pérez Castellano), Hospital Gregorio Marañón (Dr J. Almendral), Hospital de Getafe (Dr A. Pastor), Hospital Severo Ochoa (Dr A. Grande), Hospital La Paz (Dr J.L. Merino), Clínica USP San Camilo (Dr J.L. Merino).
Murcia
Hospital Virgen de la Arrixaca (Dr A. García Alberola).
Navarre
Clínica Universitaria de Navarra (Dr A. Macías), Hospital de Navarra (Dr N. Basterra).
Basque Country
Bilbao: Hospital de Cruces (Dr A. Bodegas), Hospital de Basurto (Dr M.F. Arcocha).
At the end of the article the list of the centers participants and doctors of the Spanish Catheter Ablation Registry of 2007 is exposed.
ABBREVIATIONS
AP: accessory pathways
AF: atrial fibrillation
AV: atrioventricular
AVNRT: atrioventricular node reentry tachycardia
CTI: cavotricuspid isthmus
FAT: focal atrial tachycardia
INT: intranodal tachycardia
IVT: idiopathic ventricular tachycardia
MAT: macroreentrant atrial tachycardia
NFMS: non-fluoroscopic mapping system
VT-AMI: ventricular tachycardia related to postmyocardial infarction scarring
VT-NAMI: ventricular tachycardia not related to postmyocardial infarction scarring
Correspondence: Dr. I. García-Bolao.
Irunlarrea, 13, 8.o-D. 31008 Pamplona. Navarra. España.
E-mail: igarciab@unav.es