Keywords
INTRODUCTION
Since 1990, the main aim of the Working Group on Cardiac Catheterization and Interventional Cardiology has been to collect and analyze data from the Spanish hospitals which perform relevant procedures, with steady improvements taking place in data acquisition.1-17 Data collection and their analysis indicate the interest the interventional cardiology community places on continuous improvement. Data for 2008 were presented to the members of the Section at its annual meeting which took place June 19-21, 2009, in Palma de Mallorca, Spain, and were also presented on its official website (http://www.hemodinámica. com).
The level of information obtained represents, on the one hand, the actual situation in Spain and allows comparisons with other countries and, on the other, facilitates the assessment and comparison of interventional cardiology in the different autonomous communities of Spain. The free availability of these data facilitates knowing how the resources are distributed and assessing the different trends in the use of diagnostic and therapeutic procedures.
This work presents the 18th report on interventional cardiology in Spain, and represents the activities of all the public hospitals and most of the private ones.
METHODS
Data were collected on diagnostic procedures and interventional cardiology in most of the Spanish hospitals. Data were provided on a voluntary basis and were not audited. Only anomalous data or those with values outside the trend for a given hospital in recent years were requested from each researcher for reanalisys. Collection was performed using a standard questionnaire (Appendix 1), delivered to all the Spanish cardiac catheterization laboratories in 2 formats: electronically through the website of the Working Group on Cardiac Catheterization and Interventional Cardiology of the Spanish Society of Cardiology (http.www.hemodinamica.com), to be filled in online; and more traditionally, the same questionnaire was distributed on paper. The Izasa company was in charge of distribution and collection. The information obtained was analyzed by the steering committee of the Working Group and is presented in this article.
The population was estimated at both the national level and at the level of each autonomous community with population estimations provided by the Instituto Nacional de Estadística (National Institute of Statistics) for January 1, 2008 (available from: http://www.ine.es). The Spanish population was estimated at 46 157 822 inhabitants.
Similar to previous registries, hospitals were defined as public when, regardless of their source of funding, they served a specific area within the public health system, and were considered private otherwise.
RESULTS
Infrastructure and Resources
A total of 131 hospitals performing relevant procedures in adults, including 9 that also performed pediatric procedures, participated in the present registry (Appendix 2). All 74 public hospitals and 57 private hospitals submitted their data, which represents almost all the hospitals performing relevant procedures in Spain. A total of 174 cardiac catheterization laboratories were available, of which 112 (64%) were in public hospitals. After adjusting for the population, there were 2.8 hospitals and 3.8 catheterization laboratories per million population, with no change in these figures in the last 2 years. Of the public hospitals, 71% have a 24-hour emergency response team and 69% have a cardiac surgery unit.
Regarding staff, 458 physicians performed interventions in 120 hospitals during 2008, an increase of 12% compared to 2007, with 3.5 specialists per hospital and 10 specialists per million population. Public hospitals had 4.3 specialists per hospital and 2.9 per laboratory, and private hospitals had 2.4 specialists per hospital and 2 per laboratory. Regarding nursing staff, 126 hospitals reported 550 registered nurses (DUE, from the Spanish diplomados universitarios en enfermería) and 100 radiology technicians (ATR from the Spanish técnicos de radiodiagnóstico), with a mean of 5 DUE or ATR per hospital and 3.8 per laboratory.
Diagnostic Procedures
In 2008, 136 458 diagnostic procedures were performed in Spain, with little increase compared to the previous year, probably because the number of hospitals had not increased and neither had the number of laboratories in public hospitals, which is where most of the procedures are conducted. Of these procedures, 123 031 involved coronary angiogram procedures (a 0.6% increase compared to 2007). In total, 24% were performed in women and 22% in patients more than 75 years of age (similar to 2007). Taken together, the data indicate a national average of 2658 coronary angiogram procedures per million population, fewer than in 2007, since the increase of total population was far greater than that of the number of procedures; this is different from the most recent European data published for 2005, which reported 4030 coronary angiogram procedures per million population in the countries participating in this registry.18
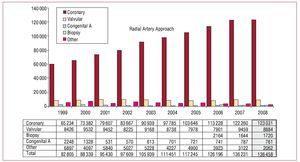
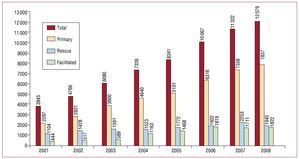
Figure 1 shows the distribution of all the diagnostic procedures and the changes mentioned, as well as fluctuations among the different patient groups, which are probably related to the data collection methodology.
Figure 1. Change in the number and type of diagnostic procedures conducted between 1998 and 2008.
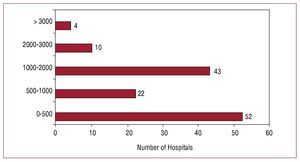
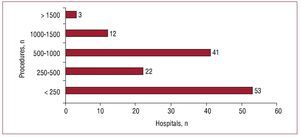
During 2008, the public hospitals performed 85% of diagnostic procedures; 57 hospitals performed more than 1000 coronary angiogram procedures and 14 hospitals performed more than 2000, representing 43% and 11%, respectively, of all hospitals (Figure 2). A mean of 1041 diagnostic procedures were performed per hospital and 784 per laboratory (without important variations compared to the last 2 registries14-17). There were 1578 (884) diagnostic procedures per public hospital, which was a slightly lower figure than that of the previous year.
Figure 2. Distribution of hospitals according to the number of coronary angiogram procedures performed.
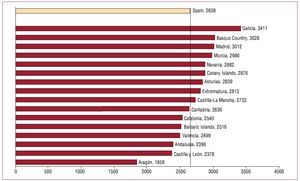
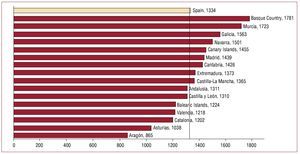
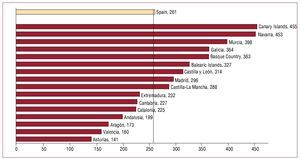
The national average of coronary angiogram procedures was 2658 (438) per million population. Figure 3 shows the distribution of these procedures per autonomous community. Two communities present values at the highest and lowest extremes of the range, whereas the others are similar, ranging around 650 procedures.
Figure 3.Distribution of coronary angiogram procedures per million population by autonomous community.
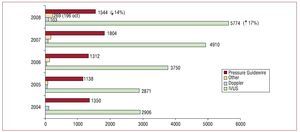
Regarding intracoronary diagnostic techniques, intravascular ultrasound (IVUS) was the most widely used, followed by pressure guidewire. The use of IVUS continued its increasing trend, although to a lesser extent (31% in 2007 and 17% in 2008); the use of pressure guidewire decreased by 14% (in 2007 it had increased by 37%). Optical coherence tomography continued to slowly increase, reaching 196 procedures; Doppler flow wire followed the same trend, increasing from 83 procedures in 2007 to 103 in 2008. Other diagnostic procedures, although few, included endothelial function studies, thermography, and intracardiac ultrasound procedures. Figure 4 shows how the use of the different diagnostic intracoronary techniques has changed in recent years.
Figure 4. Change in the different intracoronary diagnostic methods.
Regarding the access route, the use of the radial artery continues to increase, as observed in previous years, and is almost equal to use of the femoral artery; in 2008 the radial artery was used in 48% (41.4% in 2007 and 38.1% in 2006).
Percutaneous Coronary Intervention Procedures
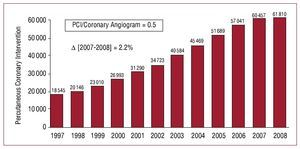
During 2008, 61 810 percutaneous coronary intervention procedures (PCI) were performed, an increase of 2.2% compared to the previous year, and was the smallest increase during the last 4 years. The recent change in PCI procedures in Spain is presented in Figure 5. The number of PCI per million population was 1334 (231) throughout the country, somewhat less than the most recently published European data, which reported a figure of 1601 PCI per million inhabitants in 2005.18 The mean number of interventional procedures was 471 per hospital and 355 per laboratory, and the average number of interventions per year per operator was 135, a decrease compared to the previous year, since the number of physicians had increased by 12% compared to 2007. Public hospitals performed 90% of PCI procedures, with a mean of 751 PCI procedures per hospital and 476 per laboratory. Regarding procedures per operator, these continued to decrease compared to the previous year for the reasons described above, with 167 procedures.
Figure 5. Change in the number of percutaneous coronary intervention (PCI) procedures between 1996 and 2008.
The ratio of PCI/coronary angiogram procedures in 2008 was 0.50 (slightly higher than in 2007) and indicates the strong increase in the number of PCI compared to coronary angiogram procedures. The number of procedures for multivessel disease did not change compared to the previous year, and constituted 27% of the total number of PCI procedures; neither was there a change in the number of procedures performed ad hoc during diagnosis (47 355; 77%).
The percentages by sex and age group fell compared to 2007 (in women, 18.9% vs 24.7% during the previous year, and in those older than 75 years, 20% vs 26.3% during 2007). In 5.2% of patients, PCI was performed on 1 or more restenotic lesions (5.5% in 2007 and 5.3% in 2006). Table 1 shows that the percentage of PCI for restenotic lesions was slightly lower than during the previous year, which could be explained by the fact that the use of drug-eluting stents (DES) remained stable. Intervention on the left main coronary artery (LMCA) remained constant in Spanish hospitals; there were 2356 procedures in 2008, of which 70% (1656) were unprotected LMCA interventions, representing 3.8% of all PCI. A total of 1780 procedures for chronic occlusion were recorded, representing 2.9% of all PCI. Grafting procedures made up 2% of the total; the saphena vein was used in 1007 procedures (81%); the mammary artery was used in 233 procedures.
Glycoprotein IIb/IIIa inhibitors (anti-GPIIb/IIIa) and antithrombotic agents were used as adjunctive drug therapy in 13 766 procedures (22.3%), with a very similar distribution to that of the previous year: 62.3% using abciximab; 19.3% using tirofiban; 9.1% using eptifibatide; and 8.9% using bivalirudin, which presented the greatest increase (3.1% more than the previous year). These figures refer to the total number of procedures in which anti-GPIIb/ IIIa agents were used, although the time of drug administration cannot be specified since this variable was not included in the questionnaire. Intraaortic balloon counterpulsation was used on 1149 occasions (in 1.85% of PCI procedures vs 2.1% of those performed in 2007), whereas other cardiac assistance methods remained at their previous level, with just 27 cases (24 in 2007).
Figure 6 shows the distribution by autonomous community of the 1334 PCI procedures per million population. The range indicates an increasing trend in recent years: 743 in 2008, 543 in 2007, and 600 in 2006, if we exclude the community of Aragón, which could not fulfill its maximum capacity of interventions due to logistics problems; 9 regions were above the national mean, as in 2007. Regarding distribution per hospital (Figure 7), the number of those performing fewer than 500 PCI procedures per year remained the same, whereas there was an increase in number of hospitals performing large numbers of procedures, with 15 hospitals performing more than 1000 PCI.
Figure 6. Distribution of percutaneous coronary intervention procedures per million population by autonomous community.
Figure 7.Distribution of hospitals according to the number of percutaneous coronary intervention procedures performed in 2008.
In relation to the overall outcome of PCI, the figures remained similar to previous years with 95% success, 4.6% failure without complications and 1.5% complications, as follows: 0.4% mortality during the procedure, 0.7% acute myocardial infarction (AMI), and 0.1% urgent surgery. Hospital mortality was 0.9%.
Intracoronary diagnostic techniques (IVUS and pressure guidewire) are basically used to make decisions on lesions of unknown severity and improve the result of intervention and, less frequently, in research protocols. As mentioned, the use of IVUS increased by 9.3% and pressure guidewire fell to 2.5% of all PCI.
The use of the radial artery as an access route continued to increase and reached 43.2% of PCI procedures versus 40.1% in 2007. The femoral route was used for 36 641 percutaneous closure devices, of which 65% were collagen based; 17.4%, suture-mediated; and 17.6% using other types of devices.
Stents
A stent was implanted during 93.3% of all PCI procedures (a total of 57 683 PCI), with 101 753 units being implanted during 2008. The number of stents per procedure continued to increase, the current ratio being 1.76 (1.7 in 2007). The use of DES reached 58.2% (59 220 units), with a 0.5% increase compared to the previous year. The number of stents implanted increased by 6.7%; the relative increase was due to DES in 58% and to conventional stent in 42%. The type of stent used depended on the characteristics of both the patients and the lesions such that either one type or both types of stent were used in a large number of procedures; thus, in 2008, of a total of 40 297 procedures on which information was provided, 8% used both types of stent compared to 52% of procedures in which DES only was used.
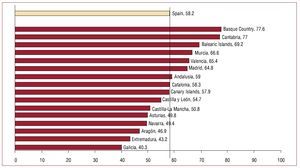
The use of DES strongly differed between the autonomous communities (ranging between 77.6% and 40.3%; Figure 8), overall with similar figures to those of 2007.
Figure 8. Distribution of the percentage of drug-eluting stents relative to the total number of stents implanted, by autonomous community.
Regarding the safety of stents, 449 cases of stent thrombosis (data submitted by 71 hospitals) were reported for the year. Their distribution was similar to that of the previous year, with 56% occurring in DES. In relation to the time of thrombosis, although there were no differences in early thrombosis, there were differences in late and very late thrombosis. Data for the last 3 years are shown in Table 2; 2008 data did not differ from 2007.
Other Percutaneous Coronary Intervention Devices and Procedures
Rotational atherectomy (rotablator) was the intracoronary technique that underwent the greatest increase in the 2008 registry, both in the number of hospitals and total number of procedures: 66 hospitals (16% increase) and 1006 procedures (30.6% increase). No directional atherectomy or intracoronary brachytherapy procedure was documented. Other devices present figures similar to those of 2007, such as the cutting balloon (1373 cases) and distal protection devices (247 procedures); however, the use of thrombus aspiration devices increased by 32% and protrusion balloons by 50%. Regarding other techniques, 35 septal ablation procedures were performed (37 in 2007), which involved 16 fistula embolization procedures and 39 stem cell implantation procedures.
Percutaneous Coronary Intervention in Acute Myocardial Infarction
A total of 112 hospitals provided data on PCI for AMI. In total, 12 079 procedures were performed in this context, which represents 20.6% of all PCI procedures, with a 6.7% increase relative to 2007. The current figures are slightly higher than those of the European Registry of 2005 (17% of all PCI procedures for infarction18). Of all procedures, 2101 (17%) were performed in women. In patients older than 75 years, 2435 procedures were performed, forming 20% of the procedures (with no change in any of the patient subgroups compared to the previous year). Anti-GPIIb/IIIa agents were used in 51.8% of angioplasty procedures for ST-segment elevation AMI (STEMI) and thrombus aspiration devices in 30% of the procedures.
The distribution of PCI performed during acute phase of AMI was similar to that of previous years: 7837 (64%) primary PCI; 1945 (16%) rescue PCI; and 1822 (15.1%) facilitated PCI (Figure 9). The growing number of AMI procedures is due to the increase of primary PCI and facilitated PCI (6.5% in both cases), whereas rescue PCI decreased by 13.7%. No data are available on the incidence of STEMI in Spain, but if we assume that the annual estimation is 45 000 AMI patients admitted to Spanish hospitals,19,20 then primary PCI would be used in just 17.4%. A total of 51 hospitals reported a median door-to-balloon time of 74 min and a mean door-to-balloon time of 80 (46) min.
Figure 9.Change in the types of percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI).
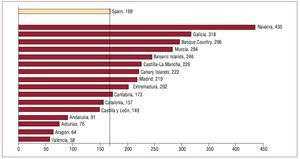
The national distribution of PCI for AMI was more dispersed than that of 2007, with a mean of 261 PCI for AMI per million population, with a range of 312 procedures (377 procedures in the case of PCI); the communities that have an established program of continuous care for AMI patients present the highest values (Figure 10 and Figure 11).
Figure 10.Distribution of percutaneous coronary interventions for acute myocardial infarction per million population and autonomous community.
Figure 11.Distribution of the primary angioplasty per million population and autonomous community.
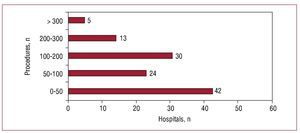
There was a mean of 106 PCI procedures per hospital (more than 2007, with 95 procedures) and the distribution between hospitals remained the same, since 58% performed fewer than 100 PCI procedures for AMI/y (Figure 12).
Figure 12.Distribution of hospitals according to the number of percutaneous coronary intervention procedures for acute myocardial infarction.
As in the other procedures, the radial artery was also used as the PCI access route for AMI, with a total of 4145 procedures, representing 34.3% of the total, with little change compared to the previous year.
A total of 1009 PCI procedures were counted in patients who presented cardiogenic shock in the acute phase of AMI. The procedure was successful in 57% of the patients and hospital mortality was 25%.
Non-Coronary Percutaneous Intervention in Adults
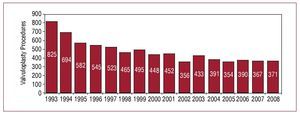
The number of valvuloplasty procedures increased by almost 10% in 2008, due to doubling the number of aortic valvuloplasty procedures, whereas the number of mitral valvuloplasty procedures has remained very similar for 8 years. There were 71 mitral valvuloplasty procedures (83%), 5 aortic valvuloplasty procedures (37 in 2007), and 16 pulmonary valvuloplasty procedures (Figure 13). The results of mitral valvuloplasty were better than during previous year and were successful in 96% of all cases; major complications occurred in 2.1% of the procedures. The most frequent complication was severe mitral regurgitation after valvuloplasty (1.6%), followed by tamponade (0.2%), and stroke (0.6%). Of 161 total percutaneous valve implantations, 10 involved the pulmonary valve and were successful in 90%, with only 1 death. The number of aortic valve implantations has already increased, with a total of 151 prosthetic valves, of which 56% were premounted on balloons and 44% were self-expanding. Self-expanding ones were successfully implanted in 91% of cases, with 8% inhospital mortality of 8%, whereas balloon-mounted ones were successful in 88% with 12% in-hospital mortality.
Figure 13. Change in the number of mitral valvuloplasty procedures in Spain.
The treatment of congenital heart disease remained the most frequent non-coronary percutaneous intervention in the registry. A total of 635 procedures were performed: the most frequent was closure of atria septal defect (ASD), with 305 total cases, of which 96% were successful. There were complications in 1.9% involving device embolization or tamponade. Procedural mortality was zero, as in 2006 and 2007. In total, 211 patent foramen ovale were closed, successfully in 99% of cases, and 23 coarctations of the aorta were treated. The 96 remaining procedures included ductus closure, interventricular communication closure and fistula closure.
A total of 45 paravalvular leaks were treated, of which 32 were mitral and 13 aortic. There were 71 aortic endoprosthesis implantation procedures, 30 of which were in the abdominal aorta and 41 in the thoracic aorta.
Percutaneous Coronary Intervention in Pediatric Patients
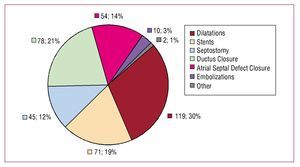
A total of 9 hospitals provided data on the pediatric age group (16 years or less), reporting 379 procedures in 2008. The most frequent procedures were dilatations, both vascular and valvular, with a total of 119 procedures. Atrial septal defect and persistent ductus arteriosus were treated in 132 patients (35% of the total). A total of 45 procedures were performed on the aorta, of which 27 were coarctations, 16 in the valve, and 2 for subaortic stenosis. Furthermore, 16 pulmonary valvuloplasty procedures were performed. The remaining procedures are shown in Figure 14.
Figure 14. Distribution of pediatric interventional procedures performed in hospitals for adults without specific pediatric activity. ASD indicates atrial septal defect.
CONCLUSIONS
The upward trend in the number of procedures performed in previous years slowed down in 2008. The only increase was in unscheduled procedures, such as angioplasty in STEMI, although this increase was less than in 2007. There was no increase in the number of public hospitals or in the number of laboratories available in them. On the other hand, the increase in the general population, which has been very large in certain communities, has led to great differences in the data on procedures per autonomous community.
Overall, diagnostic procedures were very similar to those of the previous year and only the use of intravascular ultrasound has increased, whereas the use of pressure guidewire decreased.
In general, the differences between the various Spanish autonomous communities in the use of PCI remained the same.
The clinical practice guidelines on the management of AMI have led to an increase in the number of interventional procedures due to the increase in primary PCI; even so, there are very marked differences between the autonomous communities, benefiting those which have developed a specific STEMI care plan.
The use of DES increased by 0.5% compared to 2007 (national mean, 58.2%), and was widespread among the autonomous communities with a distribution similar to that of previous years. The use of rotational atherectomy increased considerably, both in hospitals and in the number of procedures, probably due to the greater complexity of the lesions currently treated.
Use of the radial artery access route was close to 50% both for diagnosis and intervention, and was increasingly used during the acute phase of infarction.
Outside the context of PCI, there were 161 percutaneous valve implantation procedures, of which 151 were aortic valves. These figures were attained little more than 1 year after the technique was approved in Spain and this shows the willingness of Spanish interventional cardiologists to implement the latest techniques throughout the country.
Making comparisons remains problematic due to the lack of current data on the procedures performed in the countries surrounding Spain. The lack of data within Spain on the incidence of heart disease makes it difficult to assess whether the use of the different techniques matches the standards of the scientific societies.
ACKNOWLEDGMENTS
The steering committee of the Working Group on Cardiac Catheterization and Interventional
Cardiology would like to thank all the heads of the cardiac catheterization laboratories throughout Spain, those working in them, and all those in charge of data collection for their contribution towards this registry.
ABBREVIATIONS
AMI: acute myocardial infarction
DES: drug-eluting stent
PCI: percutaneous coronary intervention
Correspondence: Dr. J.A. Baz Alonso.
Cardiología Intervencionista. Complejo Hospitalario Universitario de Vigo. Meixoeiro, s/n. 36200 Vigo. Pontevedra. España.
E-mail: jose.baz.alonso@sergas.es; joseantoniobaz@gmail.com