Keywords
INTRODUCTION
Cardiovascular disease is the main cause of death worldwide, 30% of all causes of death.1 Ischaemic cardiopathy is its most frequent expression and is the main cause of individual death of the population as a whole. Different studies have shown that there is an inverse gradient between socioeconomic position (SEP) and total and cardiovascular morbidity and mortality.2-11 Recently the World Health Organization published a report entitled "Closing the gap in a generation: health equity through action on the social determinants of health" with the aim of promoting development and the application of policies and social action directed to achieving health equity.12 In this report we propose 3 types of action: to improve life conditions, attack inequalities due to the distribution of power and economic resources, and measure and understand the issue of inequalities affecting health and assess the impact of the action taken.
With reference to measuring and understanding the problem of inequalities in health, there is discussion as to which is the best indicator to determine an individual's SEP. The classical most frequently used indicators have been level of education and social class based on occupation, but it is not yet known how these indicators are related so as to define the risk associated with the SEP3,11,13. On the other hand, the mechanisms that explain this association are not defined either, although in some studies this excess risk has been explained as due to differences in the prevalence of cardiovascular risk factors.5,7,11 Many studies have been carried out on Anglo-Saxon populations in which the incidence of cardiovascular disease is much greater than that seen in countries of Southern Europe. Furthermore, there are studies that indicate a greater association between SEP and cardiovascular mortality in Northern European countries.4 In Spain there are no data on the relationship between SEP and risk of acute myocardial infarction (AMI).
The objectives of this study were to determine if there is an association between SEP and risk of AMI in our population, learn how different indicators interact and modulate the risk of AMI in association with SEP and determine if the relationship between SEP and risk of AMI is related to a greater prevalence of cardiovascular risk factors.
METHODS
Design
Population-based case-control study paired by sex, age, and year of recruitment, performed in 6 areas of the Province of Girona.
Study Population
The cases were patients with a first AMI, of 25 to 74 years of age, who were consecutively seen at the Hospital Universitario Josep Trueta (Josep Trueta University Hospital) of Girona, the area reference hospital, during the period from 1994 to 2006. AMI was diagnosed using the MONICA Study criteria of the World Health Organization.14 Those patients records that had no information on SEP were excluded.
The controls matched (1:1) the cases in sex, age (±3 years) and year of recruitment (±2 years). The controls were chosen randomly from the participants in three cross-sectional studies from the same population of origin of the cases. The cross-sectional studies were carried out during the years 1994-1996, 1999-2001, and 2003-2005. Those patients who had a previous AMI were excluded and also those with no information about the SEP. The rate of participation in the three cross-sectional studies was greater than 72%. The method used has been explained in detail in previous papers.15,16
The study protocol was approved by the local ethics committee and all the participants signed an informed consent to participate in the study.
Socioeconomic Position
The SEP was determined by social class based on occupation and maximum educational level achieved. The social and demographic variables were collected (age, sex, occupation, and educational level) using standardized questionnaires. The social class was categorized based on the occupation of the participants following the recommendations of the Sociedad Española de Epidemiología (Spanish Society of Epidemiology) based on the Spanish Classification of Occupations of 1994.17 Housewives and those beloging to religious orders, or armed forces were excluded. In the case of pensioners the categorization was based on their last occupation. Three categories of social class were created: I-II (managerial staff, higher degrees, and technicians), III (administrative staff, independent workers, supervisors of skilled workers), IV-V (skilled, semi-skilled, and unskilled manual workers). In some cases (interaction between different SEP indicators) these 3 categories were regrouped as 2: non-manual workers (social class I-II-III) and manual workers (social class IV-V).
Three categories were defined according to the highest educational level achieved: tertiary or university studies, secondary studies, and primary or lower studies.
Other Variables Collected
Standardized questionnaires were used to collect information related to the prevalence of cardiovascular risk factors. The subjects were classified as smokers if they said they smoked at least one cigarette a day during the previous year or had given up smoking during the last 12 months, as former smokers if they had given up more than 12 months ago and as non-smokers if they had never smoked. The prevalence of hypertension, diabetes, and dyslipidaemia was assessed by means of self-statements or the use of drugs to treat them.
The participants were weighed and measured barefoot and in light clothing, and the body mass index (BMI) was calculated based on weight (kilograms) divided by height (meters) squared. Three categories were defined according to BMI: normal weight (BMI<25 kg/m2), overweight (BMI≥25 and <30 kg/m2), and obesity (BMI≥30 kg/m2).
Statistical Analysis
Continuous variables were described using the mean and standard deviation. For comparison of continuous variables between groups, the Student t test or variance analysis was used. Categorical variables were expressed in percentages and the c2 test was used to determine differences between categories. Logistic regression was used for multivariate analysis. Several models were defined to analyze the association between SEP and risk of AMI in which the independent variable was level of education (3 categories) or social class (3 categories) adjusted by age and sex and subsequently including cardiovascular risk factors in the model. Furthermore, the interaction between the 2 SEP indicators used was analyzed, and 6 groups were defined according to level of education and 2 groups were defined according to social class based on whether their occupation was manual or non-manual work. A P<.05 was considered statistically significant.
RESULTS
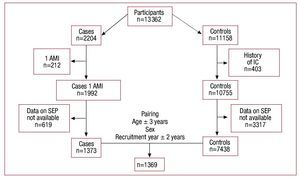
In Figure 1 it is possible to see a diagram of the registration, screening and inclusion of participants in the study. Of the 2204 cases of AMI registered during the study period, 212 were excluded because of previous AMI and 619 were excluded because we had no data on their SEP. Of the 11 158 participants in the cross-sectional studies, 403 were excluded because they had some form of ischemic cardiopathy and 3317 were excluded because we had no data on their SEP. Differences were seen between cases and controls included and not included in the study because we had no data on their SEP: a larger number of cases and controls were excluded than included, and there was a larger proportion of women. Finally 1369 cases were matched with their respective controls.
Figure 1. Diagram of the registration, screening, and inclusion of participants in the study. AMI indicates acute myocardial infarction; IC, ischemic cardiopathy; SEP, socioeconomic position.
Table 1 shows the clinical characteristics, social class and level of education of both groups. Globally mean age was 58 (SD, 10), and 14.7% of the participants were women. In the group of patients with AMI there was a larger proportion of individuals in the least favored classes (P=.002) and with a level of education of primary studies or less (P<.001). The patients with AMI also had a greater prevalence of cardiovascular risk factors (P<.001), except for obesity (P=.083).
The participants with a higher level of education were younger than those with primary studies, they were mostly men and they had a lower proportion of hypertension, dyslipidemia, diabetes, overweight and obesity (Table 2). The percentage of former smokers increased with educational level (Table 2). When differences were analyzed taking into account social class, similar results were seen although there was no greater prevalence of dyslipidaemia and diabetes in underprivileged classes nor differences between groups in smoking habits (Table 3).
Table 4 shows the raw and adjusted odds ratio of presenting an AMI according to level of education and social class. The association between level of education and risk of AMI had a linear and inverse gradient that was independent of cardiovascular risk factors.
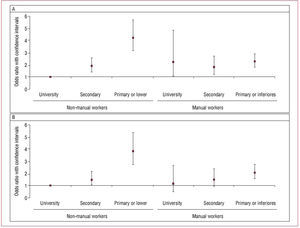
Analyzing the 2 SEP indicators available in the study and their relationship with AMI, we saw that in the crude model there was significant interaction between social class (P=.011) and level of education (P<.001). Therefore, we carried out a stratified analysis by social group, defining 2 groups based on occupation (manual or non-manual) and analyzed the association between level of education and AMI risk in each group (Figure 2). In the group of non-manual workers we saw a clear linear association between level of education and AMI risk that was independent of cardiovascular risk factors. In the group of manual workers, no association was seen between level of education and risk of AMI, although it was possible to observe an excess of risk with respect to non-manual workers, with university studies and odds ratios that ranged between 1.84 (95% CI, 1.23-2.73) and 2.3 (95% CI, 1.8-2.91) according to level of education. The excess of risk in manual workers with university or secondary education was no longer significant when it was adjusted for cardiovascular risk factors, but continued to be statistically significant in the primary education group.
Figure 2. Association between level of education and risk of AMI stratified by social class based on occupation. A: model 1, adjusted by age and sex. B: model 2, adjusted by age, sex, diabetes, dyslipidemia, hypertension, smoking, and anthropometric measurements.
DISCUSSION
In our study we saw a linear inverse association between SEP and the risk of AMI. Level of education is inversely associated, and independent of cardiovascular risk factors, with the risk of AMI in the group of non-manual workers. However, the level of education is not associated with AMI risk in manual workers. On the other hand, the group of manual workers has a greater risk of AMI than non-manual workers; this excess risk is related to a greater prevalence of risk factors in the group of individuals with secondary and university studies, but it is independent of cardiovascular risk factors in the population group with primary studies or less.
Several studies have analyzed and confirmed the relationship between SEP and risk of suffering cardiovascular events and global mortality.2-9,18-23 In Spain, the existence of an association between level of education and cardiovascular and global mortality has also been confirmed using mortality data from the city of Barcelona during the period 1992-2003,10 although no data have been published on the relationship with AMI.
On analyzing the relationship between different indicators of SEP and risk of AMI, we saw that globally and in our population these two indicators are closely correlated, although the relationship between social class based on occupation and risk of AMI did not have such a clear linear gradient as the one seen in relation to level of education. However, there was an interaction between level of education and social class that modulated the risk of suffering an AMI. In other populations an interaction between these 2 indicators has already been described in association with a healthy diet.24 These results suggest that both indicators provide additional information to define risk associated with SEP.
Many studies,3,5,6,11,25-27 also in Spain,28 have detected a greater prevalence of cardiovascular risk factors in less favoured social classes. For this reason, it has been suggested that the relationship between SEP and risk of AMI could be mediated by an accumulation of risk factors in underprivileged groups.29,30 The results of our study, as in others,7-9,31,32 suggest that both in manual workers and in non-manual workers the association seen between the group with a lower level of education and the risk of AMI is independent of classical cardiovascular risk factors. On the other hand, the excess risk observed in manual workers with secondary or university studies was mediated by cardiovascular risk factors. These results are relevant and suggest that in addition to classical risk factors there may be other factors related to level of education that could explain the excess risk in these underprivileged classes. Among these factors we could include family,8 work3,3 or financial34 stress and the social class of the father35 and other social determinants of health such as physical and social environments (safety and violence, support and social cohesion or social norms),36 which were not assessed in our study. The level of education, as well as economic level, also reflects important aspects of the formation of a person during childhood, the process of learning and skill acquisition which condition subsequent decisions on life-style and attitudes related to health.11,37
Another aspect that could influence this association is related to equity of access to health services. Differences in the accessibility of the health system may condition inequalities of health that account for a worse risk profile and greater morbidity and mortality. In a study carried out in Spain, a country where health care is universal and free, it was seen that family income was inversely associated with consultation of the family doctor, and directly with consultation of specialists, but was not associated with hospital admittance.38 This suggests that people with low socioeconomic levels consult general physicians to obtain a solution to most of their health problems and that only a few patients are sent to other more specialized care, and/ or that many consultations of general physicians are not due to health problems, but reflect other social needs.38 Although we could think that people of underprivileged social classes receive less preventive treatment that could account for the greater prevalence of risk factors, the ICAR study carried out in Spain in patients with ischemic cardiopathy did not show any differences in this sense, at least in relation to secondary prevention.39
During the last decades, the health authorities and scientific societies have expended a lot of effort on prevention of cardiovascular disease, directing their efforts to control of cardiovascular risk factors. However, and as the results of our study would suggest, especially in the population group with primary studies or less, cardiovascular disease is also related to certain social issues that include social inequalities due to economic income, social exclusion, work instability, lack of social support and lack of educational opportunities.40 In this context, the most recent European guidelines establish that social factors must be taken into account when designing comprehensive programs for cardiovascular prevention.41 These general guidelines should be specific for each population and adapt to local conditions keeping in mind the characteristics of the target population.
Study Characteristics and Limitations
One of the main characteristics of this study is its population, since we consecutively registered all the patients who were admitted for AMI to the reference hospital of the area of interest. The controls are also representative of the population of origin of the cases. Having selected controls matched for age, sex, and year of registration/recruitment allows us to interpret the magnitude of the association of our results as a relative risk.42
One of the limitations is that we were not able to include more cases of AMI as some died before reaching hospital. Another limitation of this study is that we lacked information on occupation or educational level which meant that we had to exclude participants (for example, housewives, as we did not have any information on the occupation of the household wage earner). This group of participants was older and there was a larger percentage of women, most of them housewives older than the ones included in study. The eldest group had a lower socioeconomic level, so that by excluding some of these cases we believe we favored the null hypothesis and therefore the magnitude of the association observed could be an under-estimation of the real state of affairs.
Although we used self-statements made by the study participants to determine the prevalence of risk factors, a recent study has shown that self-stated variables have a high degree of concordance with data registered in clinical histories.43
CONCLUSIONS
There is an inverse association between SEP and the risk of suffering an AMI. Level of education and social class based on occupation are indicators that provide additional information. Level of education is the indicator that captures excess risk associated with SEP independently of prevalence of cardiovascular risk factors, suggesting that in the subgroup of population with a low level of education other social health factors determine this excess risk.
ACKNOWLEDGMENTS
We wish to acknowledge all the participants and researchers of the REGICOR study without whom the study would not have been possible. This project was financed by the Spanish Ministry of Innovation and Science, Carlos III Institute/FEDER (Red HERACLES RD06/0009); the Health Research Fund (FIS 94/0539, FIS96/0026-01, FIS 97/1117, FIS99/0655, FIS99/0013-01 and FIS 99/9342); and the Agencia de Gestión de Ayudas Universitarias y de Investigación de la Generalitat de Catalunya (Agency for University Assistance and the Research Agency of the Catalonian Government), (2009 SGR 1195).
ABBREVIATIONS
AMI: acute myocardial infarction
CVD: cardiovascular disease
REGICOR: registre Gironí del Cor (Girona Heart Register)
SEP: socio-economic position
SEE EDITORIAL ON PAGES 1015-8
Full English text available from: www.revespcardiol.org
Correspondence: Dr. R. Elosua.
Grupo de Epidemiología y Genética Cardiovascular. Instituto Municipal de Investigación Médica.
Dr. Aiguader, 88. 08003 Barcelona. Spain
E-mail: relosua@imim.es
Received December 4, 2009.
Accepted for publication March 31, 2010.