Keywords
INTRODUCTION
During the percutaneous treatment of a bifurcation lesion, the main vessel stent is necessarily deformed when the side branch (SB) is dilated through the stent struts. Bench studies have been performed1-3 and certain theoretical considerations may be drawn from them. However, there are no in vivo follow-up studies that focus on the technical strategies that might preserve original main vessel stent geometry, or on the impact the degree of this stent deformation may have on late patient outcome. The purpose of this study is to investigate the 6-month intravascular ultrasound (IVUS) appearance of the parent vessel stent in patients with bifurcation lesions treated in the era of drug-eluting stents as well as the influence of technical factors on IVUS parameters.
PATIENTS AND METHOD
Patients
Our series comprises 55 patients with bifurcation lesions treated by rapamycin-eluting stents (RES) between June 2002 and June 2004 who had 6 month angiographic and ultrasonic re-evaluation. All patients fulfilled the following inclusion criteria: 1) lesion located in a major bifurcation point regardless of morphology and angulation; 2) main vessel >2.5 mm diameter; 3) SB≥2.25 mm diameter; 4) significant stenosis in both main vessel and SB origin. Patients with diffuse SB lesions were excluded. Written informed consent was obtained from all patients.
Procedure
The technique of RES implantation has been described previously.4,5 Balloon dilation of the SB or of the both vessels was performed first, followed by RES deployment in the parent vessel. The SB was then re-wired and balloon dilation of the ostium was repeated across the metallic structure of the stent. Whether to stent the SB origin or not was dictated by a randomization process between June 2002 and April 2003, and according to the criteria of the operator in patients treated between June 2003 and June 2004, so all our patients were treated with provisional or T stenting. The decision to perform final kissing balloon or balloon dilation beyond the stent limits was at the discretion of the operator. The same balloon used for stent deployment at the main vessel was also used for the final kissing balloon inflation with a second balloon of the same diameter as the reference SB. The inflation pressure was lower than for stent deployment (6-12 atmospheres). The balloon/artery ratio for each distal branch was close to 1. In the hemodynamic laboratory, patients received a bolus of 1-2 mg/kg of intravenous unfractionated heparin continuing with low-molecular-weight heparin (Fragmin®) 10 000 IU antiXa/day, ticlopidine 500 mg/day, and aspirin 150 mg/day for the first month. After this initial regimen, patients continued with clopidogrel and aspirin for 1 year. Protamine was administered at the end of the procedure allowing immediate removal of the femoral sheath. We used the CAAS II version 4.1.1 (Pie Medical Imaging, Maastricht, Netherlands) for quantitative coronary angiography, with the dye-filled catheter as a reference. Quantitative parameters were obtained at baseline condition, immediately post-procedure and at follow-up.
Follow-up Study
Patients were followed up closely by telephone and further cardiac catheterization was scheduled at 6-month evaluation or earlier in the presence of symptoms. Quantitative coronary angiography was performed at follow-up and quantitative measurements were obtained in the same selected view. Restenosis was defined as a >50% stenosis at follow-up.
All IVUS studies were obtained after a bolus (450 μg) of intracoronary nitroglycerin. A 64-element, 3.5 F monorail catheter (EndoSonics®) was used in every study. Intrastent ultrasound-measurements were obtained in the main vessel at the edges, at the minimal lumen diameter, immediately under the SB origin and at the maximal stent diameter. Proximal and distal references were examined at 1 cm from the stent borders. The following measurements were obtained at each site: external elastic lamina area, stent area and lumen area.
Statistics
Data are expressed as mean±standard deviation. A Student-Fisher unpaired t test was used to compare quantitative data from different groups of patients. Linear correlation between balloon inflation pressures and IVUS parameters was assessed with the Pearson correlation coefficient (r). A value of P<.05 was considered statistically significant.
RESULTS
Baseline and Procedural Data
Baseline clinical data are shown in Table 1. Most of patients presented an unstable clinical condition at hospital admission and 26 were diabetics. The bifurcation site was most frequently located at the left anterior descending artery/diagonal branch. The angiographic and procedural characteristics are summarized in Table 2. The use of platelet glycoprotein IIb/IIIa inhibitors at the discretion of the researchers was used in 53% of the patients.
In-Hospital and 1-Month Outcome
Angiographic success was obtained in all patients. One patient developed a non Q-wave myocardial infarction according to the immediate post-procedure serial creatine kinase determinations. The post procedure peak of creatine kinase was 102±127 IU/L. At the main vessel, the angiographic minimal lumen diameter increased after the procedure from 0.81±0.5 mm to 2.71±0.4 mm, while at the side branch, the minimal lumen diameter changed from 0.87±0.4 mm to 1.96±0.4 mm.
Clinical and Angiographic Follow-up
The mean follow-up period was 11±3 months. The 6-month angiographic re-evaluation revealed a reduction in minimal lumen diameter at the main vessel stent from 2.71±0.4 mm to 2.44±0.5 mm, and at the level of the side branch from 1.96±0.4 mm to 1.7±0.4 mm. Two patients developed restenosis at the main vessel stent and one at the SB origin. The site of restenosis was at the body of the stent distally to the bifurcation point in one patient (Figure 1) and immediately under the side branch origin in the other (Figure 2). The patient with restenosis at the SB had previously been treated with stents in both branches and final kissing balloon inflation. Repeat target lesion revascularization was required in the 2 patients with restenosis at the main vessel, while the patient with SB restenosis was followed by medical treatment. Remote site revascularization of a non bifurcated lesion treated with bare metal stents occurred at 6 months in 2 patients. No additional major adverse cardiac events were observed at follow-up in the remaining 51 patients.
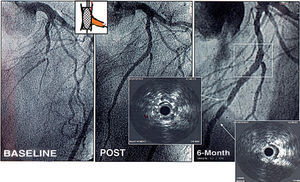
Figure 1. Bifurcation lesions at left anterior descending artery-diagonal branch treated by stenting of a long segment at the main vessel and balloon dilation of diagonal branch. At follow-up 2 sites of severe intra-stent restenosis were seen at the body of the stent but outside the bifurcation point (square).
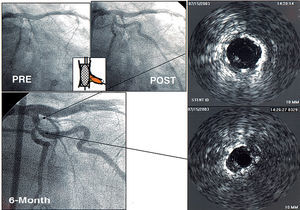
Figure 2. Patient with a bifurcation lesion treated by main vessel stenting and balloon dilation of side branch. At 6 month re-evaluation, focal restenosis developed at the stent immediately under the side branch origin. Stent underexpansion as well as neointimal proliferation can be observed in the IVUS study.
Six Months IVUS
Table 3 summarizes the 6-month follow-up IVUS findings at different sites of the parent vessel stent. A small difference between the stent and lumen area was observed as a consequence of a reduced neointimal proliferation. The mean stent area along the stented bifurcation was not uniform. So, the stent and luminal areas immediately under the SB origin were significantly smaller than at maximal stent expansion (7.0±2.1 and 6.7±1.8 mm² vs 5.5±1.4 vs 5.1±1.3 mm²; P<.05) (Figure 3 and 4). The influence of kissing balloon on this stent deformation and 6 month IVUS parameters are summarized in Table 4. As can be seen there were no significant differences between the proximal and distal references and border measurements. A small but significant difference appeared in the stent area at maximal lumen between patients with and without kissing inflation as a result of double balloon inflation in the proximal part of the stent (Figure 5). However, in terms of lumen or stent areas there were no differences at the site of the stent immediately under the side branch (Table 4 and Figure 6). IVUS measurements were similar between patients with or without SB stenting (Table 5). The balloon/artery ratio at the main vessel did not influence the lumen or stent areas at the point immediately under the SB origin or at minimal lumen diameter. The following IVUS measurements were taken in patients with a balloon/artery ratio≥1 (n=31) as compared with those with balloon/artery ratio<1 (n=24): 1) stent area at minimal lumen diameter 5.0±1.6 versus 5.0±1.1 mm² (P=NS); 2) stent area under SB 5.6±1.5 versus 5.5±1.2 mm² (P=NS); 3) lumen area at minimal lumen diameter 4.5±1.5 versus 4.6±1.1 mm² (P=NS); and 4) lumen area under SB 5.1±1.4 versus 5.0±1.2 mm² (P=NS). There was no correlation with inflation pressures during stent implantation and stent underexpansion. The correlation coefficients between inflation pressure and IVUS parameters were as follows: 1) stent area at minimal lumen diameter, r=0.18 (P=NS); 2) stent area under SB, r=0.12 (P=NS); 3) lumen area at minimal lumen diameter, r=0.21 (P=NS); and 4) lumen area under SB, r=0.13 (P=NS). The relationships between ageographic miss and the related 6-month IVUS parameters are summarized in Table 6. The proximal and distal lumen areas at the level of the border were almost identical in patients with or without balloon dilation beyond the stent limits. Furthermore none of our patients developed restenosis at stent borders.
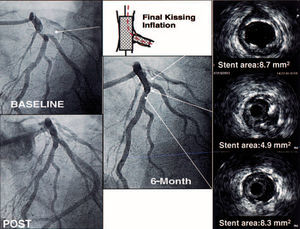
Figure 3. Bifurcation lesion at left anterior descending artery-diagonal branch, treated by stenting both vessels. Final kissing inflation was used and a significant main vessel stent underexpansion can be observed immediately under the side branch origin, compared with proximal or distal main vessel stent sites.
Figure 4. Bifurcation lesion at left main treated by stenting of the left main-left anterior descending artery and balloon dilation of the circumflex origin. The IVUS immediately under the circumflex origin shows some degree of stent underexpansion, however, the six-month angiographic follow-up study shows an excellent result on the entire bifurcation.
Figure 5. Bifurcation lesion at the left anterior descending artery-diagonal branch, treated by stenting of both vessels. The kissing balloon inflation gave a high proximal stent area, but the point immediately under the diagonal origin shows a reduction in stent area as compared with proximal or distal stent segments.
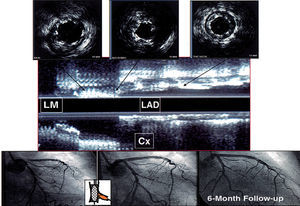
Figure 6. Example of a patient with a bifurcated lesion at the right coronary artery. The main vessel stent maintains homogeneous geometry after side branch dilation, and no deformation can be observed despite the absence of kissing balloon inflation. 1. Proximal stent. 2. At the level of the side branch. 3. Immediately after side branch origin. 4. Distal stent. Right panel: longitudinal reconstruction of the stented bifurcation.
DISCUSSION
Late IVUS findings after successful drug eluting-stent implantation has been recently reported in non bifurcated lesions and complex lesions.6-10 These studies have demonstrated the efficacy of drug eluting-stenting in inhibiting neointimal proliferation in de novo and in-stent restenosis lesions. Contrary to bare-stent treatment,11 drug-eluting stenting does not seem to need aggressive stent expansion to obtain late success. However some authors have suggested that stent underexpansion immediately after the procedure was associated with a higher restenosis rate in certain coronary lesion subsets.12
Main Vessel Stent Deformation in Bifurcated Lesions
In vitro studies have revealed stent deformation when opening struts to dilate a side branch.1-3 Final kissing-balloon has been proposed to avoid this phenomenon, based on these studies. However, there is no in vivo information as yet available. Our study suggests that some degree of stent underexpansion under the side branch origin is a frequent finding after RES treatment of bifurcation lesions. This stent deformity is not prevented by kissing balloon inflation (Table 4) or by the type of SB treatment (Table 5). The lack of plaque shifting in bench studies may also account for the disagreement between our findings and the in vitro studies. An aggressive dilation of the SB is not needed in these experimental models. On the other hand, during the experimental studies the researcher may alternatively inflate the balloons with more or less pressure to obtain adequate stent geometry. In vivo, few balloon inflations are performed by operators without continuous monitoring of stent deformity. Although this deformation may be responsible for an increase in restenosis, our findings do not support this theory. Thus, only 1 patient developed restenosis under the side branch origin (Figure 2). As can be seen in this figure, beside the stent deformation, an associated neointimal proliferation caused a severe focal restenosis. Our findings are consistent with other angiographic follow-up studies13 that also found the side branch origin to be the most frequent site for restenosis, while the main vessel stent showed a low restenosis rate.
Another interesting point to be discussed is whether or not the procedure should be completed with kissing balloon inflation. Although it has been systematically recommended during the bare-stent era,14 there were no studies that demonstrated a significant reduction in restenosis or late events after final kissing inflation.15 In the current drug-eluting stent era the need for final kissing inflation has again emerged, and authors practising crush stenting have recommended the systematic use of this approach given the improved late outcome in patients with kissing balloon.16-18 However, we think that recommendations for crushing are not applicable for provisional or T stenting. After parent vessel stenting, the series of crushing techniques compare kissing inflation vs no side branch post dilation; in contrast, we compare side branch post dilation sequentially or simultaneously with the main vessel (kissing). This means that in crush-treated patients, the group with no kissing dilation did not undergo side branch post dilation. This factor may possibly account for an increase in restenosis rates at the side branch origin.16-18
Our findings are not applicable to the treatment of bifurcation lesions with bare metal stents or other drug-eluting stents with higher late loss rates than RES. In these cases, a lower stent area after the procedure may be responsible for restenosis if moderate neointimal proliferation occurs.
Dilation Beyond Stent Limits and Border Restenosis
Restenosis in the segments adjacent to the proximal and distal edge of the stent has been an additional concern when radioactive or drug eluting-stents have been used.19,20 In the SIRIUS trial, edge restenosis occurred in 5.8% of the patients.20 Avoiding balloon dilation outside the stent limits seems to be a reasonable strategy, however, the influence of this maneuver on late IVUS border appearance has not yet been studied. Our study shows a nearly identical lumen area at the proximal and distal stent border in patients with or without geographic miss. On the other hand, none of our IVUS re-evaluated patients developed restenosis at stent borders. So, RES appears to have a protective effect against edge restenosis in patients with or without balloon dilation beyond the stent limits.
Study Limitations
The sample size may be small and, consequently, insufficient to reveal small statically significant differences between groups. The lack of randomization in the technique (kissing balloon or geographic miss) may lend bias to the study results, since the decision to use one strategy or the other was at the discretion of the operator. Finally, the absence of immediate IVUS study may make our findings more difficult to interpret.
Conclusions
Six month IVUS studies in patients treated with RES showed some degree of stent underexpansion under the SB origin after provisional or T stenting of the bifurcation lesion. This minor stent deformity was not prevented by kissing balloon inflation or by the type of SB treatment and had no significant impact on restenosis rates. IVUS border measurements are similar in patients with or without balloon inflation beyond the non-stented segment (geographic miss).
Received March 21, 2005.
Accepted for publication July 4, 2005.
Correspondence: Dr. M. Pan.
AININCAR.
Apartado Postal 2.031. 14080 Córdoba. España.
E-mail: grupo_corpal@arrakis.es