The use of second-generation drug-eluting stents compared with bare-metal stents in patients with ST-segment elevation myocardial infarction reduces the rate of major adverse cardiac events. We aimed to evaluate the impact of sex on the performance of everolimus-eluting stents vs bare-metal stents in ST-segment elevation myocardial infarction at 2-year follow-up.
MethodsThis is a sub-study of the EXAMINATION trial that randomized 1498 patients with ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention to everolimus-eluting or bare-metal stents. Primary end point was combined all-cause death, any recurrent myocardial infarction, and any revascularization. All end points were analyzed according to sex at 2-year follow-up.
ResultsOf 1498 patients included in the trial, 254 (17.0%) were women. Women were older and had higher prevalence of hypertension and lower prevalence of smoking compared with men. In contrast with men, stent diameter was smaller in women. After multivariate analysis, the primary end point was similar between women and men (hazard ratio=0.95; 95% confidence interval, 0.66-1.37), and among women, between those treated with bare-metal vs everolimus-eluting stents (hazard ratio=2.48; 95% confidence interval, 0.95-6.46). Women showed a lower rate of repeat revascularization than men (hazard ratio=0.55; 95% confidence interval, 0.32-0.95) despite worse baseline characteristics. This difference was driven by better performance of the everolimus-eluting stent in women.
ConclusionsDespite poorer baseline clinical characteristics, women with ST-segment elevation myocardial infarction treated with percutaneous coronary intervention showed outcomes similar to men. The use of everolimus-eluting stents may represent an added value in women as it showed a reduced rate of repeated revascularization compared to men.
Keywords
In Europe, more than one million women die from ischemic heart disease every year. Mortality is higher in women than in men.1 Sex may exert an independent influence on the results after percutaneous coronary intervention (PCI)2 with a similar or even lower restenosis rate despite smaller vessels than men.3 In addition, women appear to have a greater medical advantage from treatment with drug-eluting stent (DES)4 and more specifically after second-generation DES.5
The use of DES compared with bare-metal stent (BMS) reduces restenosis rate and target lesion revascularization in patients with chronic stable coronary artery disease, including high-risk patients such as diabetics.6–9 Two trials have studied second-generation DES vs BMS in ST-segment elevation myocardial infarction (STEMI) patients. In the EXAMINATION (Evaluation of the Xience-V stent in Acute Myocardial INfarcTION) trial, the use of everolimus-eluting stent (EES) did not reduce the rate of the patient-oriented primary end point (combined all-cause death, any recurrent myocardial infarction, and any revascularization) compared with BMS; however, a significantly lower incidence of repeat revascularization and stent thrombosis was observed in patients with EES, compared to those with BMS10 at 2-year follow-up.11 In the COMFORTABLE AMI trial, there was a reduced rate of major adverse cardiovascular events (cardiac death, target vessel-related reinfarction and ischemia-driven target lesion revascularization) at one year with the use of biolimus-eluting stent compared with BMS.12 There is scarce information about the performance of second-generation DES in women with STEMI.
The objective of this study was therefore to analyze the impact of sex on EES vs BMS performance in patients with STEMI at 2-year follow-up.
METHODSThis is a substudy of the all-comers, multicenter, controlled, randomized, EXAMINATION trial (NCT00828087).10 The EXAMINATION Trial randomized 1:1 a total of 1498 patients with STEMI undergoing PCI to EES (Aience®, Abbott Vascular; Santa Clara, California, United States) or BMS (Multi-Link Vision®, Abbott Vascular). The rationale of the EXAMINATION trial has been previously reported.13 Briefly, all patients with STEMI within the first 48h after the onset of symptoms who underwent emergent PCI were eligible for the study.
Exclusion criteria included lesions requiring stent sizes < 2.25mm or > 4mm, STEMI caused by stent thrombosis, age < 18 years, pregnancy, patients with known intolerance to acetylsalicylic acid, clopidogrel, heparin, cobalt-chromium, or other stent components. Patients on chronic treatment with antivitamin-K agents were also excluded. The PCI was performed according to the standard medical practice. Either unfractionated heparin, bivalirudin, or glycoprotein IIb/IIIa inhibitors were used according to the operator criteria. Before PCI, loading doses of acetylsalicylic acid (≥ 250mg) and clopidogrel (≥ 300mg) were administered to the patient. Acetylsalicylic acid (≥ 100mg/day) was prescribed indefinitely and clopidogrel (75mg/day) was prescribed for ≥ 1 year in both groups.
All participating centers submitted and received the approval of their medical ethics committee for the protocol and for the informed consent. The study was conducted in compliance with the Declaration of Helsinki, BS EN ISO 14155 part 1 and part 2, and applicable local requirements. All patients provided written informed consent.
Study End PointsStudy end points have been previously reported.13 Briefly, the primary end point was the patient-oriented end point of all-cause death, any recurrent myocardial infarction, and any revascularization. Secondary end points included the device-oriented combined end point of cardiac death, target vessel myocardial infarction, and target-lesion revascularization; all-cause and cardiac death; recurrent myocardial infarction (World Health Organization extended definition)14; target lesion revascularization; target-vessel revascularization; stent thrombosis (according to the Academic Research Consortium definitions);15 device and procedure success; and major and minor bleeding. All clinical events were adjudicated by an independent clinical event committee (Cardialysis, Rotterdam, The Netherlands) according to the Academic Research Consortium definitions.15 For the purpose of this substudy, all end points were analyzed according to sex (female group vs male group).
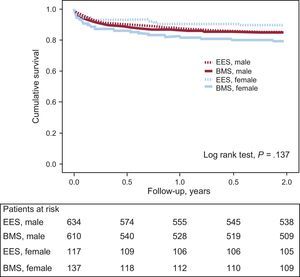
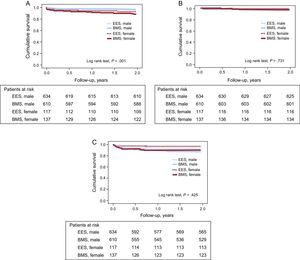
Statistical AnalysisThe study cohort was stratified according to sex (women vs men). Sex group analysis was prespecified in the EXAMINATION trial.10 Continuous variables were explored for normal distribution using the Kolmogorov-Smirnov test. Variables following normal distribution were expressed as mean (standard deviation) and non-normally distributed variables were expressed as median [inter-quartile range]. Categorical variables were expressed as count (percentage). Baseline characteristics for each sex were compared using Student t test for continuous variables and chi-square test for categorical variables. Survival curves between 4 groups (EES, male; BMS, male; EES, female; BMS, female) were constructed for assessment of primary end point using the Kaplan Meier method and compared with the log rank test.
To evaluate the association between sex and the end points, proportional hazard Cox regression analyses were developed. An exploratory univariate analysis between sex and treatment variables was performed. Covariables with a clinical justification or P<.10 were entered in the Cox-models and an interaction term between treatment and sex was included in the model. If the P value of the interaction term was < .05, effect modification was considered to be present. A significant interaction between treatment group and sex was observed with the following end points: a) all-cause death; b) any revascularization; c) target lesion revascularization, and d) target vessel revascularization. Cox regression analyses were performed for each end point. Cox model was selected according to the Akaike information criterion. The proportional hazard assumption for the Cox model was tested visually with the use of a Log-Log plot to ensure parallelism. Final Cox models for each end point with Akaike information criterion measure, C-statistics, and interaction term P-values are provided in the supplementary material.
Results were reported as hazard ratios (HR), together with the 95% confidence intervals (95%CI). The statistical power was evaluated to detect differences between study groups with a 2-sided type I error rate α of .05. All P values were 2-tailed, with statistical significance set at a level of P < .05. Statistical analyses were performed using version 2.1 of the R statistical program (R Development Core Team).
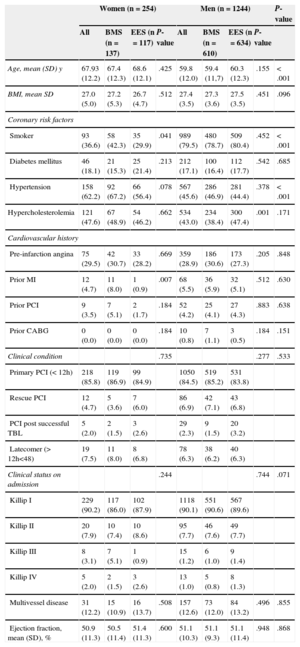
RESULTSBaseline Demographic, Clinical and Procedural CharacteristicsOut of 1498 patients randomized in the trial, a total of 254 (17.0%) women received BMS (n=137; 53.9%) or EES (n=117; 46.1%). The 1244 male patients received either BMS (n=610; 49.0%) or EES (n=634; 51.0%). Baseline demographic and clinical characteristics of all patients are depicted in Table 1. Women were older, fewer were smokers, and they had a higher prevalence of hypertension than men. Among women, those allocated to BMS had a higher prevalence of prior myocardial infarction and a higher prevalence of smoking.
Baseline Demographic and Clinical Characteristics
| Women (n=254) | Men (n=1244) | P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All | BMS (n=137) | EES (n=117) | P-value | All | BMS (n=610) | EES (n=634) | P-value | ||
| Age, mean (SD) y | 67.93 (12.2) | 67.4 (12.3) | 68.6 (12.1) | .425 | 59.8 (12.0) | 59.4 (11,7) | 60.3 (12.3) | .155 | < .001 |
| BMI, mean SD | 27.0 (5.0) | 27.2 (5.3) | 26.7 (4.7) | .512 | 27.4 (3.5) | 27.3 (3.6) | 27.5 (3.5) | .451 | .096 |
| Coronary risk factors | |||||||||
| Smoker | 93 (36.6) | 58 (42.3) | 35 (29.9) | .041 | 989 (79.5) | 480 (78.7) | 509 (80.4) | .452 | < .001 |
| Diabetes mellitus | 46 (18.1) | 21 (15.3) | 25 (21.4) | .213 | 212 (17.1) | 100 (16.4) | 112 (17.7) | .542 | .685 |
| Hypertension | 158 (62.2) | 92 (67.2) | 66 (56.4) | .078 | 567 (45.6) | 286 (46.9) | 281 (44.4) | .378 | < .001 |
| Hypercholesterolemia | 121 (47.6) | 67 (48.9) | 54 (46.2) | .662 | 534 (43.0) | 234 (38.4) | 300 (47.4) | .001 | .171 |
| Cardiovascular history | |||||||||
| Pre-infarction angina | 75 (29.5) | 42 (30.7) | 33 (28.2) | .669 | 359 (28.9) | 186 (30.6) | 173 (27.3) | .205 | .848 |
| Prior MI | 12 (4.7) | 11 (8.0) | 1 (0.9) | .007 | 68 (5.5) | 36 (5.9) | 32 (5.1) | .512 | .630 |
| Prior PCI | 9 (3.5) | 7 (5.1) | 2 (1.7) | .184 | 52 (4.2) | 25 (4.1) | 27 (4.3) | .883 | .638 |
| Prior CABG | 0 (0.0) | 0 (0.0) | 0 (0.0) | .184 | 10 (0.8) | 7 (1.1) | 3 (0.5) | .184 | .151 |
| Clinical condition | .735 | .277 | .533 | ||||||
| Primary PCI (< 12h) | 218 (85.8) | 119 (86.9) | 99 (84.9) | 1050 (84.5) | 519 (85.2) | 531 (83.8) | |||
| Rescue PCI | 12 (4.7) | 5 (3.6) | 7 (6.0) | 86 (6.9) | 42 (7.1) | 43 (6.8) | |||
| PCI post successful TBL | 5 (2.0) | 2 (1.5) | 3 (2.6) | 29 (2.3) | 9 (1.5) | 20 (3.2) | |||
| Latecomer (> 12h<48) | 19 (7.5) | 11 (8.0) | 8 (6.8) | 78 (6.3) | 38 (6.2) | 40 (6.3) | |||
| Clinical status on admission | .244 | .744 | .071 | ||||||
| Killip I | 229 (90.2) | 117 (86.0) | 102 (87.9) | 1118 (90.1) | 551 (90.6) | 567 (89.6) | |||
| Killip II | 20 (7.9) | 10 (7.4) | 10 (8.6) | 95 (7.7) | 46 (7.6) | 49 (7.7) | |||
| Killip III | 8 (3.1) | 7 (5.1) | 1 (0.9) | 15 (1.2) | 6 (1.0) | 9 (1.4) | |||
| Killip IV | 5 (2.0) | 2 (1.5) | 3 (2.6) | 13 (1.0) | 5 (0.8) | 8 (1.3) | |||
| Multivessel disease | 31 (12.2) | 15 (10.9) | 16 (13.7) | .508 | 157 (12.6) | 73 (12.0) | 84 (13.2) | .496 | .855 |
| Ejection fraction, mean (SD), % | 50.9 (11.3) | 50.5 (11.4) | 51.4 (11.3) | .600 | 51.1 (10.3) | 51.1 (9.3) | 51.1 (11.4) | .948 | .868 |
BMI, body mass index; BMS, bare-metal stent; CABG, coronary artery bypass graft; EES, everolimus-eluting stent; MI, myocardial infarction; PCI, percutaneous coronary intervention; SD, standard deviation; TBL, thrombolysis.
Data are expressed as No. (%) or mean (standard deviation).
Compared with men, women had a lower use of manual thrombectomy and IIb/IIIa inhibitor. Women allocated to EES had a higher use of manual thrombectomy than those treated with BMS. Overall, smaller stents were implanted in women than in men (Table 2).
Procedural Characteristics, Biomarkers, and Antiplatelet Treatment at 1-year Follow-up
| Women (n=254) | Men (n=1244) | P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All | BMS (n=137) | EES (n=117) | P-value | All | BMS (n=610) | EES (n=634) | P-value | ||
| Manual thrombectomy | 150 (59.1) | 73 (53.3) | 77 (65.8) | .043 | 826 (66.4) | 408 (66.9) | 418 (65.9) | .722 | .025 |
| Maximal stent diameter, mean SD, mm | 3.07 (0.42) | 3.10 (0.41) | 3.00 (0.43) | .273 | 3.23 (0.45) | 3.20 (0.50) | 3.30 (0.40) | .161 | < .001 |
| ST segment resolution post PCI > 70% | 144 (64.6) | 84 (68.3) | 60 (60.0) | .198 | 708 (62.7) | 354 (64.2) | 354 (61.2) | .297 | .598 |
| cTnI, mean SD, ng/mL | |||||||||
| Pre-procedure | 9.97 (32.03) | 6.42 (14.50) | 14.27 (44.70) | .096 | 10.00 (36.67) | 9.08 (29.58) | 10.87 (42.34) | .463 | .990 |
| Peak | 47.18 (88.13) | 45.10 (74.20) | 49.00 (99.30) | .756 | 58.95 (101.34) | 63.60 (108.20) | 53.90 (93.10) | .139 | .130 |
| Antiplatelet regimen | |||||||||
| GPIIb/IIIa inhibitor | 114 (44.9) | 60 (43.8) | 54 (46.2) | .706 | 671 (53.9) | 325 (53.3) | 346 (54.6) | .647 | .008 |
| 1 year | |||||||||
| ASA | 212 (85.4) | 116 (84.7) | 96 (82.1) | .599 | 1107 (90.6) | 545 (89.3) | 562 (88.6) | .943 | .016 |
| Clopidogrel | 205 (85.4) | 107 (78.1) | 98 (83.8) | .933 | 1061 (90.2) | 497 (81.5) | 564 (89.9) | .578 | .028 |
ASA, acetylsalicylic acid; BMS, bare-metal stent; cTnI, cardiac troponin I; EES, everolimus-eluting stent; GPIIb/IIIa, Glycoprotein-IIb/IIIa; PCI, percutaneous coronary intervention; SD, standard deviation.
Data are expressed as No. (%) or mean (standard deviation).
Adherence to dual antiplatelet therapy at 1 year was lower in women, compared with men (Table 2).
Clinical OutcomesMen vs WomenClinical outcomes between women and men are shown in Table 3. After 2 years of follow-up, both the patient-oriented primary end point (Figure 1) and the device-oriented end point (Figure 2) were similar between women and men.
Summary of Study End Points at 2-year Follow-up, Stratified by Sex
| Women (n=254) | Men (n=1244) | P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All | BMS (n=137) | EES (n=117) | P-value | All | BMS (n=610) | EES (n=634) | P-value | ||
| Primary end point (death/MI/any revascularization) | 40 (15.7) | 28 (20.4) | 12 (10.3) | .026 | 197 (15.8) | 101 (16.6) | 96 (15.1) | .494 | .972 |
| Death (all cause) | 23 (9.1) | 15 (10.9) | 8 (6.8) | .255 | 46 (3.7) | 22 (3.6) | 24 (3.8) | .867 | < .001 |
| Myocardial infarction | 4 (1.6) | 3 (2.2) | 1 (0.9) | .627 | 18 (1.4) | 9 (1.5) | 9 (1.4) | .934 | .497 |
| Any revascularization | 18 (7.1) | 14 (10.2) | 4 (3.4) | .035 | 150 (12.1) | 81 (13.3) | 69 (10.9) | .195 | .022 |
| Device-oriented end point (cardiac death/TV MI/clinically driven revascularization) | 25 (9.8) | 17 (12.4) | 8 (6.8) | .137 | 119 (9.6) | 64 (10.5) | 52 (8.2) | .165 | .797 |
| Target-lesion revascularization | 8 (3.1) | 7 (5.1) | 1 (0.9) | .053 | 56 (4.5) | 34 (5.6) | 17 (2.7) | .010 | .332 |
| TV revascularization | 10 (3.9) | 8 (5.8) | 2 (1.7) | .092 | 85 (6.8) | 47 (7.7) | 29 (4.6) | .021 | .084 |
| Nontarget vessel revascularization | 11 (4,3) | 9 (6.6) | 2 (1.7) | .058 | 87 (7,0) | 43 (7.0) | 44 (6.9) | .940 | .118 |
| Definitive/probable stent thrombosis | 3 (1.2) | 3 (2.2) | 0 (0.0) | .107 | 25 (2.0) | 17 (2.8) | 10 (1.6) | .143 | .374 |
| Major bleeding | 4 (1.6) | 3 (2.2) | 1 (0.9) | .394 | 16 (1.3) | 8 (1.3) | 8 (1.3) | .938 | .715 |
| Minor bleeding | 14 (5.5) | 9 (6.6) | 5 (4.3) | .424 | 43 (3.5) | 22 (3.6) | 21 (3.3) | .776 | .119 |
BMS, bare-metal stent; EES, everolimus-eluting stent; MI, myocardial infarction; TV, target vessel.
Data are expressed as No. (%).
A significantly higher rate of death was observed in women than in men. After multivariate analysis, this difference was no longer significant (HR=1.4; 95%CI, 0.75-2.72).
Women had a lower rate of repeat revascularization than men, even after adjusting for possible confounders (HR=0.55; 95%CI, 0.31-0.95). The statistical power to detect differences in the rate of repeat revascularization, from 12.1% in men to 7.1% in women, was 73.3%.
No difference in definitive/probable stent thrombosis was observed between women and men. Rates of major and minor bleeding were similar in both groups.
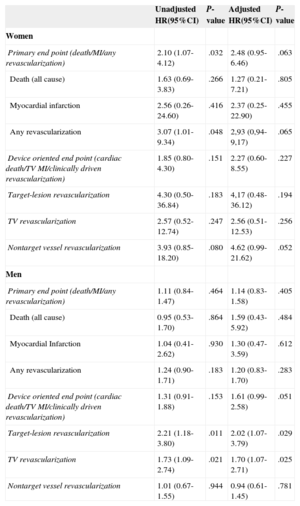
Everolimus-eluting Stent vs Bare-metal Stent in WomenClinical outcomes between EES vs BMS in women are depicted in Table 4. The primary end point was significantly higher in women treated with BMS than in those treated with EES (HR=2.1; 95%CI, 1.07-4.12). After multivariate analysis, this difference was no longer significant (HR=2.49; 95%CI, 0.95-6.46). The statistical power—with a 2-sided type I error rate α of .05 to detect a reduction in the rate of primary end point in women from 20.4% in the BMS group to 10.3% in the EES group—was 59.9%. With the assumption of the same 2-sided type I error rate, the statistical power was 20.1%, 12.0%, and 56.1%, respectively, to detect a reduction in the rate of death from 10.9% in the BMS group to 6.8% in the EES group, myocardial infarction from 2.2% in the BMS group to 0.9% in the EES group, and in any revascularization from 10.2% in the BMS group to 3.4% in the EES group.
Summary of Cox Proportional Hazard Models (Bare-metal Stent vs Everolimus-eluting Stent by Sex) at 2 Years Follow-up
| Unadjusted HR(95%CI) | P-value | Adjusted HR(95%CI) | P-value | |
|---|---|---|---|---|
| Women | ||||
| Primary end point (death/MI/any revascularization) | 2.10 (1.07-4.12) | .032 | 2.48 (0.95-6.46) | .063 |
| Death (all cause) | 1.63 (0.69-3.83) | .266 | 1.27 (0.21-7.21) | .805 |
| Myocardial infarction | 2.56 (0.26-24.60) | .416 | 2.37 (0.25-22.90) | .455 |
| Any revascularization | 3.07 (1.01-9.34) | .048 | 2,93 (0,94-9,17) | .065 |
| Device oriented end point (cardiac death/TV MI/clinically driven revascularization) | 1.85 (0.80-4.30) | .151 | 2.27 (0.60-8.55) | .227 |
| Target-lesion revascularization | 4.30 (0.50-36.84) | .183 | 4,17 (0.48-36.12) | .194 |
| TV revascularization | 2.57 (0.52-12.74) | .247 | 2.56 (0.51-12.53) | .256 |
| Nontarget vessel revascularization | 3.93 (0.85-18.20) | .080 | 4.62 (0.99-21.62) | .052 |
| Men | ||||
| Primary end point (death/MI/any revascularization) | 1.11 (0.84-1.47) | .464 | 1.14 (0.83-1.58) | .405 |
| Death (all cause) | 0.95 (0.53-1.70) | .864 | 1.59 (0.43-5.92) | .484 |
| Myocardial Infarction | 1.04 (0.41-2.62) | .930 | 1.30 (0.47-3.59) | .612 |
| Any revascularization | 1.24 (0.90-1.71) | .183 | 1.20 (0.83-1.70) | .283 |
| Device oriented end point (cardiac death/TV MI/clinically driven revascularization) | 1.31 (0.91-1.88) | .153 | 1.61 (0.99-2.58) | .051 |
| Target-lesion revascularization | 2.21 (1.18-3.80) | .011 | 2.02 (1.07-3.79) | .029 |
| TV revascularization | 1.73 (1.09-2.74) | .021 | 1.70 (1.07-2.71) | .025 |
| Nontarget vessel revascularization | 1.01 (0.67-1.55) | .944 | 0.94 (0.61-1.45) | .781 |
95%CI, 95% confidence interval; HR, hazard ratio; MI, myocardial infarction; TV, target vessel.
Women treated with EES had a lower rate of repeat revascularization, compared to women treated with BMS. This association did not reach statistical significance after adjusting for confounders (HR=2.93; 95%CI, 0.94-9.17). Women treated with EES showed a trend towards a lower risk of definitive or probable stent thrombosis than women treated with BMS (2.2% vs 0.0%; P=.107). All events were numerically higher in the BMS group, without reaching statistical significance.
DISCUSSIONThe major findings of this study can be summarized as follows: a) no differences in primary end point were found between men and women or between women treated with EES and those treated with BMS; b) women with STEMI had higher long-term mortality than men; however, after multivariate adjustments, this difference was no longer significant, and c) women had a lower risk of repeat revascularization after STEMI than men.
Although women with STEMI had higher mortality when compared with men after 2 years of follow-up, after adjustment of differences in clinical profile and treatment, sex was not an independent risk factor for death after STEMI. Our results are consistent with several studies that describe sex-related differences in clinical profile, treatment, and outcomes among patients with STEMI.16–19 Differences in age, treatment, and commorbid conditions may partially explain this finding.20–22 In addition, it has been shown that women with STEMI are treated less frequently with primary PCI, due to delay in diagnosis secondary to the presence of atypical symptoms.23
A lower use of effective therapies in women, compared with men, has been associated with a poorer prognosis. In our study, use of manual thrombectomy and glycoprotein inhibitors IIb/IIIa was less frequent in women than in men. Despite the previous difference, postprocedural ST-segment resolution was similar between both groups.
In our study, women had a lower rate of revascularization than men. The difference was primarily driven by a lower rate of revascularization among women treated with EES. Target-lesion revascularization showed a lower trend without reaching statistical significance. Women treated with EES had the lowest revascularization rate of all groups. Women and men allocated to BMS had similar rates of revascularization. It has been suggested that women are at highest risk for lumen compromise in response to neointimal formation due to smaller-sized vessels than men.4 The fact that women have a lower risk of restenosis despite their worse baseline characteristics has been called the “sex paradox”.2,24–26 A recent study that evaluated the impact of sex on first-generation DES performance found a reduced rate of repeat revascularization in women, compared with men. after the use of paclitaxel-eluting stents27 and sirolimus-eluting stents.28 Lansky et al29 evaluated the role of sex in the efficacy of EES compared with paclitaxel-eluting stents, in a post hoc analysis. After 1 year of follow-up, women treated with EES had a significantly lower rate of repeated revascularization than women treated with paclitaxel-eluting stents.29 Nakatani et al26 demonstrated that female sex is independently associated with lower neointimal obstruction and maximum cross-sectional narrowing in patients receiving zotarolimus-eluting stents; conversely, women patients who received BMS had a higher neointimal obstruction than men, although the finding was no longer significant after adjusting for baseline characteristics, suggesting an absence of sex differences with respect to neointimal hyperplasia after BMS implantation.26 The reason for this paradox has not been clearly elucidated. Interaction between diabetes and sex have been suggested as a possible cause.3 However, women and men in our study had a similar prevalence of diabetes. We also found an almost significant lower rate of nontarget vessel revascularization in EES vs BMS among women, which could be related to the study design: the treatment allocation was not blinded to the operators, and a different strategy could be followed regarding the treatment of nonculprit lesions.
Plaque composition may play a role in the observed differences in outcomes. A recent study confirmed a sex-specific difference in the extent and composition of coronary plaque. Ruiz-Garcia et al30 imaged the in vivo characteristics and composition of untreated nonculprit lesions with grayscale and radiofrequency intravascular ultrasound in patients with acute coronary syndromes. Women younger than 65 years of age had a lower number of nonculprit lesions, fibroatheromas, and total lesion length than men. Plaque ruptures were also observed more frequently in men than in women.30 The sex-related differences in plaque characteristics disappeared with age. In uncontrolled studies, referral bias could explain a lower revascularization rate in women compared with men.31
After initial concerns about the use of DES in STEMI patients, safety and efficacy of DES in STEMI have been reported in several trials with similar rates of death, reinfarction, and stent thrombosis, and a reduced rate of angiographic and clinical restenosis, with the greatest benefits among patients at high risk for restenosis with BMS.10,12,32 Our findings are reassuring and confirm that there are no sex-related safety issues after EES use in women with STEMI.
LimitationsOur findings are the result of the analysis of a negative trial and should be interpreted as hypothesis-generating; also, revascularization was clinically driven, which might have led to reduced use in women because of less referral for repeat catheterization rather than less restenosis. Also, due to the high type II error rates (40.1% for the primary end point, 79.9% for death, 88% for myocardial infarction, and 43.9% for any revascularization) our results must be interpreted with caution.
A lower use of manual thrombectomy in women should be taken into account when interpreting the results. Finally, menopausal status was not evaluated in this study; however, given the age of the women included in the EXAMINATION trial it is likely that most participants were postmenopausal.
ConclusionsDespite their worse baseline characteristics, women with STEMI treated with PCI had outcomes similar to men, with a lower rate of repeat revascularization.
CONFLICTS OF INTERESTNone declared.
Antonio Serra, Hospital Universitario de Sant Pau, Barcelona, Spain; Rosana Hernández-Antolín, Hospital Universitario San Carlos, Madrid, Spain; Vicente Mainar, Hospital General de Alicante, Alicante, Spain; Marco Valgimigli, University Hospital Ferrara, Ferrara, Italy; Maurizio Tespili, University Hospital Bolognini Seriate, Bergamo, Italy; Pieter den Heijer, Amphia Ziekenhuis, Breda, The Netherlands; Armando Bethencourt, Hospital Son Espases, Palma de Mallorca, Spain; Nicolás Vázquez, Hospital A Coruña, A Coruña, Spain; Bianca Backx and Gerrit-Anne van Es, Cardialysis, Rotterdam, The Netherlands.