Keywords
INTRODUCTION
The ST-Elevation Myocardial Infarction (STEMI) requires the non-delayed use of one of 2 established treatments, fibrinolysis or mechanical re-perfusion, to reopen the artery that caused the infarction. The primary percutaneous coronary intervention (PPCI) has shown to be the reperfusion treatment of choice for patients with STEMI in experienced centres where a door-to-balloon delay is predicted to be less than 90-120 minutes.1,2 This technique decreases mortality, reinfarction, cerebral infarctions and haemorrhaging complications when compared to fibrinolytic treatments, according to that shown in recent meta-analyses.3,4 Nevertheless, the generalisation of its use is restricted by the absence of adequately equipped hospitals and experienced personnel to carry it out. Patient transfer strategies have been developed to resolve this inconvenience by taking patients from centres with no haemodynamic possibilities to specialised centres with PPCI alerts 24 hours a day. These protocols have proved in multiple randomised studies and meta-analysis to be safe, feasible and more effective than local fibrinolysis.5-9
Nevertheless, this strategy produces an overload for the interventionist hospital that has to cover its own patients and those from the peripheral centres with a limited amount of resources. The flow of said patients after performing the interventionist procedure is not clearly defined and is currently a controversial topic.10
The goal of this study is to evaluate the safety of an early return protocol to the referral centres of patients with acute myocardial infarction transferred to an interventionist hospital for PPCI.
METHODS
Acute Myocardial Infarction Galician Care Program (PROGALIAM in Spanish)
Since 2005, the Galician Health Service (SERGAS, in Spanish) launched a program for primary percutaneous coronary interventions called PROGALIAM.11 This is a health care program for STEMI at the regional level where 9 hospitals without coronary interventionism, 3 interventionist hospitals and the Medical Emergency 061 Service participate. Our centre (A Coruña University Complex, CHUAC, in Spanish) is the reference for primary percutaneous coronary interventions in northern Galicia and it covers a population of 1,030,752 inhabitants. According to the program, the patients with STEMI that arrive to the hospitals with haemodynamic laboratories and that are candidates for reperfusion treatment as defined in the clinical practice guidelines,1,2 are treated
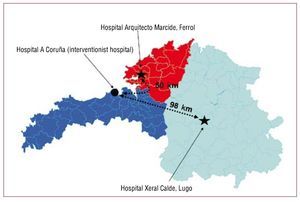
using urgent primary percutaneous coronary interventions. Those patients that first arrive to a non-interventionist hospital are rapidly transferred to our centre by means of the 061 Medical Ambulance Services to receive this treatment. The transfer is highly recommended there is a delay > 2 hours between onset of symptoms and arrival at the centre; onset if they arrive within the first 2 hours but can be safety transferred to the haemodynamic laboratory in < 110 minutes, and in patients with symptoms and signs of heart failure, cardiogenic shock or in those with absolute contraindications for fibrinolysis. Our centre accepts transfers from 4 such hospitals, located between 50 and 150 km away. The decision to activate the interventionist team is handled by the physician in charge of the Intensive Care Unit of the non-interventionist hospitals or directly by the 061 doctor and always by agreement with the interventionist cardiologist. The program allows for complete access to PPCI 24 hours a day, 7 days a week. After the procedure, if the patient is asymptomatic and haemodynamically stable, and no additional interventionist procedures are foreseen, the 061 medical ambulances once again handle the transfer of the patient to the Intensive Care Unit of the referral hospital (in our centre, this is possible with the Arquitecto Marcide Hospital in Ferrol and the Xeral Calde Hospital in Lugo) (fig. 1). In this waiting period before returning, the patients is kept in a bed that is especially assigned for the PROGALIAM program, located in the Intermediate Care Unit of the Cardiology Floor. If said bed were occupied, the patient would be kept in the Emergency area or in the Intensive Care Unit. The protocol was approved by the ethics committees of the hospitals involved.
Figure 1. Northern area of the PROGALIAM Interventionist Hospital and associated hospitals with Coronary Units where the returns can be made. The transfer distance is also shown.
Study population and criteria for the return of patients
All of the patients that arrived with typical angina pain persisting more than 30 minutes with an ST elevation ≥ 1mm in ≥ 2 continuous derivations (or reciprocal depression ≥ 1mm in the V1 or V2 derivations, or a block of the left branch of the bundle of His and within the first 12 hours after the first symptoms were PPCI candidates. Patients with symptoms > 12 hours, with an absence of vital signs or with a questionable diagnosis were habitually excluded from the protocol. There are no restrictions within the program based on age, gender, clinical status or comorbidities.
The parameters used to decide if a patient is suited to be returned or not include the absence of chest pain, the presence of haemodynamic stability (systolic Blood Pressure > 90 mmHg and Heart rate < 100 bpm), and freedom from vasoactive support or ventricular support devices (intraaortic balloon pump)] and acute severe congestive heart failure [use of endovenous diuretic drugs at high doses, need for high-flow oxygen (FiO2 ≥ 50%) or need of mechanical ventilation], with the final decision taken by the medical team in charge of the patient to carry out said return. Likewise, patients with left main artery disease were excluded from the protocol. For certain patients, the return had to be delayed for technical reasons, including the presence of heart failure awaiting adequate treatment, the realisation of a second procedure the next day (treatment of significant lesions different from that causing the problem) or arrival during night hours, which could overload the 061 Medical Units or cause discomfort for the patients due to beginning percutaneous coronary interventions during the night shift.
A group of patients from the area of the interventionist hospital, treated with a primary percutaneous coronary intervention in the same period, of similar clinical characteristics and eligible under the defined criteria and therefore eligible for the early return, were used as a control group. The haemodynamic team prospectively selected patients for the control group who did not present any complications in the first 24 hours after being admitted to the hospital.
Treatment protocol
All of the patients received 250mg of salicylic acid when diagnosed and before being transported to the catheterization laboratory. The use of IIb/ IIa platelet receptor antagonists [Abciximab, (Reopro©), initial dose 0.25mg/kg followed by a perfusion of 0.125µg/kg/min during 12 hours] was determined by the criteria of the doctor that initially treated the patient, but it was highly recommended in the protocol. The administration of the initial dose of 300mg of Clopidogrel was carried out in the referral hospital or during the transfer as determined by the doctor responsible for the patient. If not received a similar dose was administered after the percutaneous coronary intervention and before leaving the laboratory. During the catheterisation, between 5,000 and 10,000IU of non-fractioned Heparin were administered depending on if anti IIb/IIIa drugs were used and following the clinical guidelines.12,13 A dose of 200 to 300 micrograms of intra-coronary nitro-glycerine was administered before the percutaneous coronary intervention.
Definitions of the events
All of the events were evaluated in the first 30 days after the index procedure. The events in the patients of the control group were evaluated by doctors of the Interventional Cardiology Unit of our hospital by reviewing the clinical history or by telephone calls if necessary. Regarding the events of the returned group, doctors from the referral hospitals were in charge of the follow-up in the same manner.
Definition
Readmission: readmission due to cardiovascular causes in any centre. Ischemic complications: anginalike chest pain accompanied by electrocardiographic changes and/or re-elevation of myocardial damage markers after the PPCI. Stroke: new transitory or permanent neurologic deficit. Death: death due to any cause during the follow-up period. Major cardiovascular events: occurrence of any of the previously mentioned events.
Statistical analysis
The results are presented as mears ± 1 Standard Deviation (SD) for the normally distributed continuous variables, as medians (inter-quartile range) for the non-Gaussian distributed continuous variables and as percentages for the categorical variables. The categorical variables were compared using the Chi-Square test or Fisher's exact test. The quantitative variables were analysed using the Student's t-distribution or the Mann-Whitney U test depending on the presence or not of a normal distribution. An analysis of logistical regression adjusted for age, gender, cardiovascular risk factors, use of abciximab, presence of multi-vessel disease, the ejection fraction, the success of the procedure and the time since symptoms appeared until the reperfusion was used to evaluate the independent effect of the return of the patients regarding the incidence of major cardiovascular events after 30 days. The variables in the model were introduced in blocks. All of the statistical analyses were performed using the SPSS 15.0 statistical package for Windows (SPSS, Chicago, Illinois).
RESULTS
In the period between the 1st of June, 2005, and the 31st of March, 2005, 279 patients (40% of the total number of PPCI performed) were transferred from hospitals equipped with a Coronary Unit to have the PPCI performed in our centre. Of them, 200 (72%) were newly returned to their referral hospitals and 79 (28%) stayed at our centre until they were discharged. During this same period, 432 patients of our catchment area were treated with PPCI, of which 297 (68%) were used as the control group for comparison with the returned group.
The clinical and angiographic characteristics of the patients included in the study are shown in table 1. Table 2 details the reasons why some of the 279 patients were not returned to the referral centres; 7 o these patients died in the first 30 days (8.8%).
Cardiovascular events after 30 days
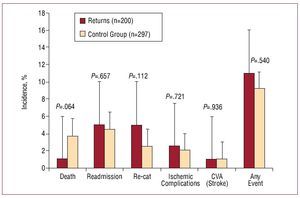
Significant differences were not observed concerning the following occurrences: death (1% vs. 3.7%, p=0.064), readmission (5% vs. 4.5%, p=0.657), ischemic complications (2.5% vs. 2%, p=0.721), new catheterisation (5% vs. 2.5%, p=0.112), stroke (1% vs. 1%, p=0.936) or any cardiovascular event (11% vs. 9.2%, p=0.540) between the patients of the returned group and those from the control group during the follow-up period (fig. 2). Incidence of re-infarction secondary to a subacute thrombosis of the treated vessel was observed in 2% of the returned group and in 1.3% of the control group, without significant differences (p=0.570). Conventional stents were used in all of the cases.
Figure. 2. Bar graph showing the number of cardiovascular events in the follow-up period. CVA indicates cardiovascular accident (stroke); Re-cat, recatheterisation.
In a logistic regression analysis adjusted for potential confounding variables, the return of the patients was not significantly associated with the occurrence of cardiovascular events in the follow-up period (odds ratio 1.32, confidence interval 95%, 0.62-2.8). The results of the multi-variable analysis are shown in table 3.
Descriptive analysis of the group of returned patients
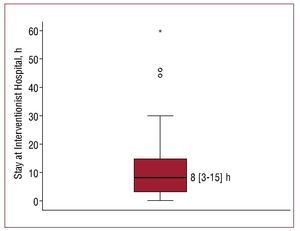
In the early return group, the hospital stay in the interventionist centre was highly variable, but the median was 8 hours (inter-quartile range 3-15 hours), (figure 3). 63% of the patients stayed < 12 hours and only 2.4% stayed > 24 hours in the interventionist centre.
Figure. 3. Box diagram showing the distribution of the hours of hospital stay of the patients in the interventionist hospital.
No complications were observed (ischemic complications, sustained ventricular arrhythmias, bradi-arrhythmias that required stimulation, haemodynamic instability, stroke, severe heart failure or bleeding in the puncture site) in the return of the patients to the referral centre.
The low mortality stands out for the entire series, with only 2 deaths (1%) in the first 30 days. Of them, only one can be attributed to cardiovascular causes related with the infarction, while the other was due to an oesophageal rupture in the days after the catheterisation. This patient had been remitted for suspicions of anterior STEMI without having shown lesions in the coronary angiography.
In the follow-up period, 10 patients (5%) had a new catheterisation performed during the first month after the event. Of them, 4 (2%) cases were urgent catheterisations for sub-acute thrombosis of a conventional stent and two of these patients had been discharged from their reference hospital. The other 6 patients had elective catheterisations performed in 2 of them, the procedure was repeated during their initial stay in the interventionist centred two of these patients by residual dissections in the first catheterisation; in other 3 patients, the angiograph was repeated because of chest pain without any obvious new coronary alteration, after being returned to their referral centres. In this last group, 2 patients had been discharged and were readmitted to their referral centre coronary angiography.
After being discharged from the referral centre, 9 patients (4.5%) were readmitted for different causes. Of them, 4 cases were readmitted for a new catheterisation because of suspicions of ischemic complications, and in only 2 of them, a new coronary lesion was found to be responsible for the process (corresponding to 2 of the sub-acute thromboses of the conventional stents). The causes of admission for the other 5 patients were heart failure (2 patients), pre-syncope, atrial fibrillation and kidney failure. No major bleeding was observed in patients that had the interventionperformed via the femoral route and there were only minor bruises in the puncture site in 2 cases without clinical repercussions. No vascular complications were detected in the patients that had the PPCI performed via the radial route.
DISCUSSION
This study demonstrates, for the first time, the results of a study that specifically evaluates the safety and feasibility of a protocol that contemplates the early return of patients transferred for PPCI to their referral centres.
Different studies have demonstrated that the PPCI is a cost-effective strategy when compared to fibrinolysis.14-18 Initially associated to greater health care costs, as time has gone by, it is now the strategy that allows for a greater adjustment of the resources related to quality of life. This benefit is maintained in the analyses even after adding the cost of using the coronary stents.14 The benefit obtained is due to a lower number of events in the PPCI group as it is related with a more definitive and permanent coronary reperfusion than with fibrinolysis. This results in a shorter hospital stay and a lower number of repeated procedures and readmissions during the follow-up period, which could notably decrease costs. Recently, Selmer et al18 have published that this benefit is extended for longer than 5 years after the infarction, with an increase in the life expectancy of almost a year in the PPCI group.
The strategies that consist in transferring patients to perform the PPCI have been analysed in various randomised studies confirming their superiority when compared with local fibrinolysis when the inherent delay to this strategy is not excessive and is adjusted to that recommended in the practical clinical guidelines.5-8 One problem that has yet to be resolved is the healthcare and economic overload that the maintenance of this program implies when offering PPCI to the majority of the population in the interventionist hospital that must cover those patients in their area along with those from the surrounding areas, with limited resources. On the other hand, in the non-interventionist hospitals, those patients that are not considered for PPCI are usually handled with fibrinolytic treatment or without any reperfusion treatment that, as already described, is associated to an increase in the use of resources and healthcare expenses. Thus, a strategy that is consistent with the transfer and return of patients to their referral centres entails a double benefit; on one hand, it allows for a generalised access to the PPCI, with the clinical benefit that this implies, and on the other hand, it decreases the possible use of resources not only in the interventionist centre, that would not be obligated to handle the hospital stay of these patients, but also in the non-interventionist hospital, as the patients treated with PPCI would be cost-effective for them. This strategy not only decreases the hospital stays in the interventionist hospital, but it also increases the well-being of the patient and his or her family and promotes collaboration with the doctors that remit the patients. Up to today's date, we only dispose of one study in existing literature where data is shown regarding the return of patients transferred for PPCI.19 In this study, Margheri and cols. describe a cohort of 135 patients treated using PPCI of which 92 had been transferred from peripheral hospitals. Of these, 81 (88%) could be returned to their referral centres. This return was carried out in the first 2 hours after the procedure. Nevertheless, in this article, no specific criteria are defined to carry out the transfer nor are the cardiovascular events of this group of patients specifically analysed. Likewise, it is interesting that 12% of the returned patients were returned with an intra-aortic balloon inserted. Regarding this initial publication, our study shows a longer stay in the interventionist hospital, with various explanations for this finding. First of all, the return program after primary percutaneous coronary intervention is something relatively new and still in the initial phases of the protocol; the lack of experience led to a longer transfer waiting time. Another reason for the longer waiting times is that a large number of patients arrive during the night shift. In this case, to avoid the discomfort of the patient and his or her family and to avoid overloading the 061 medical units, it was decided that the transfer would be delayed until the next morning, thus incrementing the waiting time for the return. The availability of the 061 Medical Unit also produces a delay, given their multiple responsibilities for emergency response. And finally, in certain occasions, the patients had to stay, waiting to return, in units other than the Cardiology Unit, which was also associated to an increase in the waiting time for the transfer.
The greatest concern regarding the use of this strategy is its safety, given that it implies the transfer of patients that have suffered a recent coronary event and an invasive medical procedure. These patients are in a potentially unstable clinical situation and their mobilisation implies risk. Nevertheless, our results point to the fact that the early transfer of adequately selected patients is completely safe. It is of great importance that no clinical events were reported during the transfers, and the frequency of the cardiovascular events studied in the 30 day follow-up period is similar to or lower than those previously reported regarding PPCI treatment.20,21 It also does not differ from the events presented in a cohort with a similar clinical profile, not returned because it pertained to the same area as the interventionist hospital. Nevertheless, in spite of having selected a cohort of similar clinical characteristics, there were differences between the groups regarding the use of abciximab, the temporary delays in applying treatment and length of hospital stay. The first difference can be explained by the fact that the use of abciximab before transfer was strongly recommended in the protocol of the program, while its use in our own hospital depended on the criteria of the doctor that treated the patient in that moment and of the delay foreseen until the patient would arrive to the catheterisation laboratory. When the patient was evaluated in the emergency room of our centre and the catheterisation laboratory was available, the patient was transferred immediately and the decision to administer abciximab was postponed until the results of the procedure were known. Regarding the delays, the differences observed are inherent to the nature of the groups. The returned patients are transferred to other centres and, therefore, their delays are greater. Nevertheless, said delays did not act as predictors of events in the multivariable analysis, reflecting reports by Antoniucci et al.22 an d by De Luca23 et al that the prognosis of patients with low-risk STEMI are less dependent on the temporary delays. And finally, the hospital stay in the referral centre of the returned patients completely depended on the doctors in charge of the patients. Given that there were not many medical complications in this group, the longest delay of their stay did not seem due to purely clinical motives.
Although a greater number of patients of the return group underwent coronary angiography during the first 30 days, this difference was not significant. This increase is probably related to the low threshold of the medical team in charge of the patient to request a new catheterisation if angina symptoms reappeared. Within this group, the group of patients with sub-acute thrombosis of the vessel treated deserves special attention. This phenomenon is infrequent and unpredictable and those cases that happened after discharge had been admitted more often than that recommended in the guidelines.24
When handling this complication, it is essential to maintain an adequate flow of communication between the non-interventionist hospitals and our centre so that, once a complication is diagnosed, the transfer system can be activated again and the transfer can be performed without excessive delays. Following these lines, the second revascularisation of the patients where sub-acute thrombosis of the stent had been identified was carried out within certain time intervals similar to those of the first procedure and none of these patients died during the follow-up period. In our opinion, this tight collaboration is essential for the program to be successful.
Finally, we must point out that if this cohort of patients conforms a highly selective group within those patients with STEMI, it is very numerous, as 72% (CI 95%: 66% to 77%) of the patients remitted from hospitals with Coronary Units could be returned early on to their referral hospital. In the group of non-returned patients, 28 patients were included that had stayed in the interventionist hospital to undergo a second elective interventionist procedure or to undergo a stratification test in case of multi-vessel disease. These patients remained stable and without adverse complications during their stay and they could be subsidiaries to form part of the return group in the case of ambulatory transfers for elective percutaneous coronary interventions, increasing the proportion of returnable patients to 82% (CI 95%: 77% to 86%).
Limitations of the study
This study has various limitations. Firstly, it is a descriptive study of a specially selected cohort of patients that does not represent the totality of infarcted patients and those included within a myocardial infarction care program that was not available in all of the hospitals. Specifically, the returned patients have to meet certain clinical criteria that include them in a low-risk profile, they are returned to hospitals with coronary units and the return is done in a medical ambulance that has the same resources available as those that carry out the transfer of the patient from the referral hospitals to the interventionist centre. This strategy cannot be generalised and applied to other hospitals that do not have these resources. The time of the stay in the interventionist hospital is variable and in some cases surpasses 24 hours. More studies are needed that explore if inferior times or even immediate returns are an equally safe strategy.
CONCLUSIONS
The return of patients transferred for PPCI to their referral centres is a safe and feasible strategy when it is applied to a selected group of patients and after a variable time of observation in the interventionist hospital. More studies are needed to confirm this first experience, as well as analysing the possibility of the immediate transfer after the interventionism in those patients that are eligible for transfer.
ABBREVIATIONS
PPCI: primary percutaneous coronary intervention
STEMI: ST-elevation myocardial infarction
SEE ARTICLE ON PAGES 1350-2
Correspondence: Dr. R. Estévez-Loureiro.
Departamento de Cardiología. Complejo Hospitalario Universitario. As Xubias, 84. 15006 A Coruña. España.
E-mail: roiestevez@hotmail.com
Received April 29, 2009.
Accepted for publication June 25, 2009.