The manuscript by Abu-Assi et al1 published in this issue of Revista Española de Cardiología addresses several important issues:
- What is the relevance of an internationally derived risk score for a contemporary Spanish population of patients presenting with acute coronary syndrome?
- Is the risk score applicable despite higher intervention rates than in the originally derived data set?
- Is the Global Registry of Acute Coronary Events (GRACE) risk score applicable to the ST elevation myocardial infarction (MI) and the non ST elevation acute coronary syndrome (ACS) cohorts in this population?
To address these questions, the authors prospectively collected information on consecutive patients admitted with a diagnosis of acute coronary syndrome between February 2004 and February 2009 in their institution. They present data from 1183 patients with confirmed ST elevation myocardial infarction, non-ST elevation myocardial infarction, and "unstable angina" (defined as typical chest pain with or without suggestive electrocardiographic changes and without a rise in plasma troponin concentration) for whom sufficient data was available to complete the GRACE risk score and whose vital status was known at 6 months. Data were available in 99% of the population for all the prognostic variables in the GRACE risk score and the authors were able to determine the vital status of all patients except 79 (6.3%).
Key findings were that the GRACE risk score accurately predicted outcomes in this contemporary Spanish population of patients with ACS, despite differences in clinical practice patterns as compared to the GRACE cohort.2 In their report, patients were 3 times more likely to be treated using an early intervention strategy (72% vs 27%) on their index admission, perhaps reflecting more contemporary practice in Europe and North America, and patients were approximately twice as likely to have a significant troponin rise as those in the GRACE cohort. At the same time, the use of thrombolytics was reduced 2.5-fold and balanced by a 3-fold increase in the use of invasive angiography and coronary revascularisation. In addition, the use of statin therapy and potent antiplatelet therapy (clopidogrel) was around 2-fold higher. Along with the increased use of invasive treatments and an increase in antiplatelet treatment, the risk of complications was around 2-3 times higher in this Spanish cohort than in the GRACE population, driven predominantly by the incidence of renal failure and major haemorrhage. Despite these differences, Abu-Assi et al show that the discriminatory capacity of the GRACE score was excellent, with the area under the ROC curve 0.86 (95% confidence interval, 0.81-0.92 for all patients), 0.90 (95% CI, 0.83-0.98 for those with ST elevation MI) and 0.86 (95% CI, 0.78-0.93 for those with non ST elevation MI).1
Thus, the authors have provided the first validation of the GRACE risk score in a Spanish hospitalised population of patients with ACS.
What is the Clinical Significance of these Findings?
Further, underlying this question, why do we need a risk score and are the risk characteristics not obvious in routine clinical evaluation? Clinically estimated scoring is commonly applied but the evidence suggests that without a systematic scoring system physicians do not estimate risk accurately. One study recently compared physicians' assessment of individual risk of 1956 patients enrolled into the Canadian ACS2 Registry between 2002 and 2003 with established and validated risk-scoring systems, and found only weak positive correlations.3 The authors particularly identify the misguided perception that young patients are perceived to be at higher risk than elderly patients, whereas it is clear from registry data that the opposite is true. Indeed the GRACE investigators assessed the rate of percutaneous coronary intervention following admission with an acute coronary syndrome in the GRACE cohort stratified into the 3 tertiles of cardiovascular risk as determined using the GRACE risk score. They demonstrated a clear treatment paradox, whereby those at lowest risk were 50% more likely to receive intervention than those in the highest risk group— perhaps demonstrating a risk-averse strategy or poor assessment of individual risk by physicians.4 Other investigators have demonstrated similar paradoxes in the use of evidence-based pharmacological treatments such as statins.5 Reflecting these findings, guidelines including those of the European Society of Cardiology6 and the ACC/AHA SCAI strongly recommend that patients with acute coronary syndrome should undergo risk stratification.
Why then is Risk Stratification so important?
Firstly, robust evidence from randomised trials demonstrates that specific treatment strategies including interventional therapy and more potent anti-platelet and anti-thrombotic therapies are particularly effective in higher risk patients. Conversely, the ACC/AHA guidelines provide a class III recommendation (something that should not be done) for interventional therapy among low risk stabilised patients with non-ST elevation ACS.7 Therefore, in order to guide these treatment strategies, there is a need to assess cardiovascular risk on an individual basis. This is key to ensuring both that patients likely to derive the most benefit from intervention receive appropriate care and that those unlikely to derive benefit are not given unnecessary and potentially risky treatments. This approach is attractive both in tailoring care for each individual patient and from a simple health economic standpoint.
What is the GRACE Risk Score and How is it derived?
The GRACE risk score was developed in a cohort of 21 688 patients enrolled into the multinational observational GRACE registry2 that now includes 123 hospitals across 14 countries in Europe, North and South America, Australia, and New Zealand. The GRACE registry was designed to reflect an unbiased population of patients with acute coronary syndrome, irrespective of their eventual hospital location and whether or not the admitting hospital had access to specialised cardiac intervention services. Predictors of outcome were derived based on the presenting clinical and biomarker characteristics of the patients. Nine factors were identified that independently predicted death or a combined outcome of death and myocardial infarction (age, heart failure, peripheral vascular disease, systolic blood pressure, Killip class, serum creatinine concentration, elevated cardiac enzymes, cardiac arrest on admission, and ST segment deviation on the electrocardiogram) and these were incorporated into a continuous model of cardiovascular risk (Figure).8 These 9 factors conveyed more than 90% of the predictive power of the full multivariable model and provide more robust discrimination than based on troponin alone (Figure). Interestingly, when adjusted for other factors sex is not a predictor of outcome. This model was subsequently validated both internally in a further 22 122 patients in the GRACE registry and externally in 12 142 patients with acute coronary syndrome in the Global Use of Strategies to Open Occluded Coronary Arteries (GUSTO) IIb dataset.2 The GRACE risk score shows excellent predictive accuracy both for death and the combined outcome of death and myocardial infarction at 6 months from the index event (c=0.82 and 0.70, respectively). The GRACE investigators recently updated the model to ensure accuracy based on patients treated in the current era.9
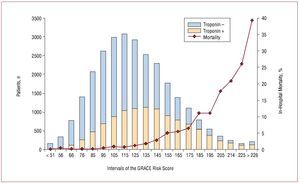
Figure. GRACE nomogram showing risk of in-hospital mortality in 27 406 patients following the incidence of non-ST segment elevation myocardial infarction by GRACE risk score. The bar chart describes the distribution of troponin positive (white bars) and troponin negative (black bars) patients according to GRACE score. The black line depicts the observed hospital mortality rates. Although troponin elevation shifts the distribution to the right, there is substantial overlap for any given level of risk. Figure reproduced with permission from Steg PG et al.
The results of the linked study by Abu-Assi et al1 are in line with other validation studies carried out in non-GRACE cohorts, where the GRACE score consistently out-performs the other available risk models,10 accurately predicting in-hospital mortality as well as 6-month outcome.11 The predictive accuracy for the incidence of recurrent myocardial infarction is, however, less good (c=0.64 for all patients). There is therefore a need to improve the predictive capacity for this important adverse outcome, and the search continues for additional risk markers such as NT-proBNP.12 Despite this limitation, the GRACE score is now widely established in independent analyses to be the best predictor of cardiovascular risk following acute coronary syndrome. A recent analysis performed by the NICE (National Institute for Health and Clinical Excellence, UK) group systematically compared a variety of scoring systems including TIMI (Thrombolysis In Myocardial Infarction), PURSUIT (Platelet glycoprotein IIb/IIIa in Unstable angina: Receptor Suppression Using Integrellin Therapy), GRACE, PREDICT, EMMACE (Evaluation of Methods and Management of Acute Coronary Events), AMIS (Acute Myocardial Infarction in Switzerland), and the UA (Unstable Angina) risk score, before testing the GRACE risk score in the completely unselected MINAP (Myocardial Infarction National Audit Project) dataset.13 The MINAP dataset includes 75 627 patients admitted to all hospitals in England and Wales over a 2-year period. The GRACE model performed extremely well (c=0.825, 95% confidence interval, 0.82-0.83), and NICE have proposed that the GRACE (or other validated scoring system) risk score should be applied in all patients as soon as they present to hospital, in order to stratify risk and to guide further treatment.
Is it Feasible to Apply a Risk Scoring System in Clinical Practice?
The GRACE risk score is a more complex algorithm, because it uses continuous variables like age and renal dysfunction, than other scores (for example the TIMI risk score where age is dichotomous <65 or >65). Calculating the GRACE risk score from a paper nomogram is not the most appropriate method of applying the scoring system in clinical practice. The algorithm can be freely downloaded to a hand-held device or to a computer and then entering the data and calculating the risk score takes less than 30 seconds. So can this be applied in clinical practice and do you need a doctor to estimate the risk score? This question was tested in South East Scotland by McLean and colleagues from a cohort of 7000 unselected patients presented to hospital with suspected cardiac pain.14 That study provided the evidence that cardiac nurses can accurately apply the GRACE risk score, in electronic format, and that despite the fact that it was tested in patients with "suspected cardiac pain" rather than "demonstrated ACS," it nevertheless provided robust risk prediction not only for outcomes but also for confirmation of an ACS diagnosis and length of hospital stay.
Summary
In summary, this study by Abu-Assi provides evidence of the validity of the widely accepted GRACE score, in contemporary cardiology practice.1 It adds to the evidence that this well-validated, simple to apply, risk score should be applied to all patients presenting with acute coronary syndrome in order to stratify risk and to guide further treatment—reducing the existing treatment paradoxes and with the aim of narrowing the gap between evidence and practice—. A universal adoption of this approach is likely to have a far greater impact on overall mortality and morbidity following acute myocardial infarction than the small improvements demonstrated in recent large scale drug trials, and we suggest that this important, and seemingly "low-tech," intervention should not be overlooked.
SEE ARTICLE ON PAGES 640-8
Full English text available from: www.revespcardiol.org
Both authors contributed equally to this work.
Disclosure: Dr Langrish is supported by a British Heart Foundation Clinical PhD Studentship. The GRACE project is supported by an unrestricted grant from Sanofi-Aventis (Paris, France). Dr Fox is the Duke of Edinburgh British Heart Foundation Chair of Cardiology, University of Edinburgh, UK.
Correspondence: Prof K. A. A. Fox,
Centre for Cardiovascular Science. University of Edinburgh, Chancellor's Building. 49 Little France Crescent. Edinburgh EH16 4SB. United Kingdom
E-mail: K.A.A.Fox@ed.ac.uk