In a recent article published in Revista Española de Cardiología, Gabaldón-Pérez et al.1 present a study on the prognostic value of magnetic resonance imaging (MRI) findings in a large cohort of chronic coronary syndrome patients older than 70 years (n=2486). The MRI study involved visual determination of myocardial perfusion with the use of adenosine and measurement of myocardial fibrosis with gadolinium enhancement. Analysis of the data provided the following main results: first, the ischemia burden predicted overall mortality, and second, there was an association between myocardial revascularization and mortality in patients with severe ischemia, defined as 5 cardiac segments showing hypoperfusion. This was the optimal cutoff according to the ROC curve exploring the association between the extent of ischemia and mortality.
Although the first result would be expected, it is a robust finding and the authors should be congratulated for demonstrating it with a relatively new technique in the study of chronic coronary syndrome in elderly patients. However, the second finding seems more controversial and deserves a discussion in parallel to the results of the recent ISCHEMIA2 trial.
In this and other studies,1,3,4 MRI is one of the major stratifiers implemented in chronic coronary syndrome, together with stress echocardiography5,6 and methoxy-isobutyl-isonitrile single photon emission tomography (MIBI-SPECT),7,8 with the advantage that the first 2 techniques use “green” technology. Furthermore, MRI compares very favorably with MIBI-SPECT and coronary computed tomography-derived fractional flow reserve.9 In patients with normal findings on perfusion MRI, the annualized risk of events is 1%, a value similar to that found for normal stress results using other imaging techniques, and the risk of events rises proportionally to the ischemia burden.10 However, perfusion MRI is performed much less often than other techniques, particularly in comparison to nuclear methods. In the ISCHEMIA2 trial, MRI was used in only 5% of participants, whereas stress echocardiography was used in 21%, MIBI-SPECT in 50%, and conventional stress testing without imaging in 24%.11
The data regarding the prognostic value of ischemia are compelling, whichever the imaging technique used, and the study by the Valencia group1 provides additional information in this line. Nonetheless, recent specific analyses of the ISCHEMIA trial according to the degree of ischemia (mild, moderate, or severe) and the angiographic grade on the Duke Coronary Artery Disease index showed that ischemia did not predict total mortality, not even severe ischemia, although a severe angiographic grade (eg, 6 points on the Duke index) was found to be predictive.11 Irrespective of this consideration, once again, revascularization was unable to prevent death or other events over and above medical treatment alone, whatever the degree of ischemia. Even in patients with multivessel disease (n=1456) including the proximal left anterior descending artery (a group the ISCHEMIA researchers may have been reluctant to include), the study arm receiving invasive treatment did not fare better than those treated conservatively. At this point it should be noted that the ISCHEMIA study2 was not designed to assess the role of ischemia in prognosis, as most of the patients included had moderate or severe ischemia (inclusion criteria) and there was no ischemia-free control group. The central laboratory of the study deemed that only 606 patients (12%) had no or mild ischemia, whereas the remaining patients (89%) had a moderate or severe degree, and all were randomized to receive either optimal medical treatment (OMT) or OMT plus revascularization. Although the protocol initially included only patients with moderate or severe ischemia, those with no or mild ischemia were also randomized.
The ISCHEMIA2 trial was actually designed to assess the impact of revascularization on outcomes in patients with chronic coronary syndrome and significant ischemia (89% of patients). In this sense, it is a randomized study with a rigorous design in which all participants had coronary artery disease. Furthermore, it is an industry-independent study with little loss to follow-up (< 1%). The primary endpoint was a composite of cardiovascular death, myocardial infarction, hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest. Total mortality was also evaluated. Risk factor control was excellent, with a median blood pressure value of 129/74mmHg and low-density lipoprotein cholesterol of 64mg/dL in the last study visits. At the end, it was reported that 100% of participants were taking antiplatelet drugs, 95% statins (66%, high intensity), and 69% angiotensin converting-enzyme inhibitors/angiotensin II receptor blockers.2
Therefore, in light of the ISCHEMIA2 findings, the results regarding the possible benefit of revascularization in patients with severe ischemia (5 hypoperfused segments on MRI) in the study by Gabaldón-Pérez et al.1 may be somewhat questionable. Of note, just as ISCHEMIA was not designed to determine the impact of ischemia on events, the study by Gabaldón-Pérez et al.1 was not designed to determine the relationship between ischemia and the benefit of revascularization. There was a borderline P value for this association (P=.046) and no difference in mortality between revascularized and nonrevascularized patients with severe ischemia. There was, however, a difference in patients without severe ischemia, although this result may have been due to an excess of surgical mortality. Therefore, as was seen in ISCHEMIA, revascularization did not provide a benefit over OMT in patients older than 70 years with extensive ischemia on MRI.
In a recent larger observational study,4 the same authors did find this association when a cutoff of 5 segments was used for ischemia, after which revascularization could be beneficial. These findings prompted a call for an exclusive randomized study with MRI, which could be more precise than other imaging techniques to resolve the issue. Again, this view is not supported by the ISCHEMIA data. Revascularization was no better than OMT in the subset of patients with severe ischemia, defined as those with ≥15% affected myocardium on MIBI-SPECT, at least 4 dyssynergic segments on stress echocardiography, ischemia ≥25% on MRI, or angina together with an ST segment decrease on stress testing without imaging and ≤7 METs.
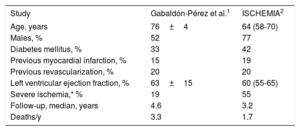
Obviously, the clinical characteristics of patients in the study by Gabaldón-Pérez et al.1 and those of the ISCHEMIA trial are not comparable (table 1). The ISCHEMIA protocol excluded patients with a left main coronary artery lesion (8%) and left ventricular ejection fraction <35%, whereas such patients may have been included in the studies by the Valencia team1,4 and may have benefited from revascularization. In fact, of all the subgroups analyzed in ISCHEMIA—patients with diabetes,12 severe ischemia,11 severe coronary disease,11 or kidney failure13—only patients with a history of heart failure or left ventricular ejection fraction 35% to 45%14 showed a prognostic benefit from revascularization. Similarly, in the STICH study, a benefit of surgical revascularization over OMT at 10 years was found in patients with ischemic ventricular dysfunction.15 Of note, the main indication for MRI in 20% of patients in the study by Gabaldón-Pérez et al.1 was to assess myocardial viability. Although late gadolinium enhancement was not an independent predictor of death in this study, MRI determination of myocardial fibrosis is a robust marker of myocardial viability and it is likely that the viability-ischemia ratio assisted clinical decisions on revascularization, at least in some patients.
| Study | Gabaldón-Pérez et al.1 | ISCHEMIA2 |
|---|---|---|
| Age, years | 76±4 | 64 (58-70) |
| Males, % | 52 | 77 |
| Diabetes mellitus, % | 33 | 42 |
| Previous myocardial infarction, % | 15 | 19 |
| Previous revascularization, % | 20 | 20 |
| Left ventricular ejection fraction, % | 63±15 | 60 (55-65) |
| Severe ischemia,* % | 19 | 55 |
| Follow-up, median, years | 4.6 | 3.2 |
| Deaths/y | 3.3 | 1.7 |
Severe ischemia was defined by at least 5 hypoperfused cardiac segments on magnetic resonance imaging in Gabaldón-Pérez et al.1 and by hypoperfusion ≥25% on magnetic resonance imaging (≈ 4 segments), ≥15% affected myocardium on methoxy-isobutyl-isonitrile single photon emission tomography (MIBI-SPECT), at least 4 dyssynergic segments on stress echocardiography, or angina with ST segment descent and ≤7 METs on conventional stress testing in the ISCHEMIA trial.2
One of the strengths of the ISCHEMIA study is the rigorous application of medical treatment in both arms, with quarterly medical visits and continuous recommendations to adhere to OMT, as well as central control of the laboratory analyses. It is difficult to conform to all these aspects in real-world observational studies, but in view of the results, it is likely necessary.
Whereas this1 and other studies3–7,9 have demonstrated the importance of ischemia as a prognostic marker in chronic coronary syndrome, ischemia measurement in coronary patients receiving the required preventive therapy is actually of less consequence, as the conservative approach is just as effective as invasive treatment in these patients. This indicates that revascularization should be reserved for cases in which symptomatic therapy fails. At this point, simple evaluation of symptoms with a stress test may suffice, rather than implementing more costly and demanding ischemia tests.16 Perhaps, as is drawn from the ISCHEMIA study, it may be more important to first determine the symptoms instead of determining the ischemia. In other words, we should first ask ourselves what, if any, symptoms are present in our patient, rather than how much ischemia.
FUNDINGThis study received no financial support.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.