To the Editor,
The association between sinus node dysfunction (SND) and sleep apnea-hypopnea syndrome (SAHS) is well recognized.1 Recently, our group confirmed an elevated prevalence of SAHS in patients with SND.2 In addition, there is indirect evidence of an association between atrial fibrillation and SAHS,3 and of bradyarrhythmia reversion with noninvasive nasal ventilation.4,5 We present a patient with both diseases, and in whom SAHS treatment with noninvasive nasal ventilation (continuous positive airway pressure [CPAP]) completely reversed sinus node dysfunction.
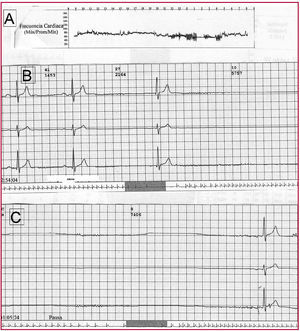
The patient was a 52-year-old man, smoker, hypertensive, and obese, with no other relevant history. He consulted his cardiologist for severe asthenia and a weight gain of about 15 kg in the past 6 months. The physical examination was normal, except for a body mass index of 39 and bradycardia of 54 bpm. The electrocardiogram (ECG) confirmed sinus bradycardia with a PR interval of 220 ms and right bundle-branch block. Holter monitoring was consistent with SND, with an average heart rate of 51 bpm (range, 31-86 bpm), an occasional run of self-limiting atrial tachycardia, and pauses of up to 5.7 s in the daytime and 7.4 s at night (Figure 1). The echocardiogram was strictly normal, except for mild diastolic dysfunction. The patient had brought a stress test, performed 18 months earlier for atypical chest pain, in which 13 metabolic equivalents (MET) and a maximum heart rate of 156 bpm had been achieved. He was sent to our department for implantation of a dual-chamber pacemaker. On further questioning, the patient denied syncope or presyncope, complaining basically of asthenia and drowsiness during the day. Despite a lack of consistency between the Holter findings and the symptoms, pacemaker implantation was proposed based on the latter; however, the patient did not accept. In view of symptoms indicating SAHS, he was referred to the sleep unit to rule out this condition. He presented an Epworth Sleepiness Scale score of 11, and the polysomnography showed an apnea-hypopnea index per hour (AHI/h) of 47, indicating that the patient met the SAHS criteria. Continuous positive airway pressure treatment at a pressure of 12 cm H2O was started, and weight loss was recommended.
Figure 1. Upper panel (A) indicates the heart rate trend throughout the tracing (mean, 51 bpm; range, 31-86 bpm). Lower panel (B) shows the daytime pause of 5.7 s. Lower panel (C) shows the nighttime pause of 7.4 s.
After 3 months of CPAP treatment, the patient was completely asymptomatic, from both the respiratory and cardiologic viewpoint. The baseline heart rate was now 72 bpm and repeat Holter showed absence of SND criteria, with a mean ventricular rate of 66 bpm (range, 48-110 bpm) (Figure 2). Daily or nighttime pauses are not observed.
Figure 2. Heart rate trend in the second Holter performed 3 months after initiating CPAP treatment. CPAP indicates continuous positive airway pressure.
The patient was followed for 2 years and has remained asymptomatic to the time of writing. Two new Holter tests are consistent with the last one described.
This case illustrates the close relationship between these two diseases, not only because of the high prevalence of SAHS in patients with sinus node dysfunction, as was shown by our group,2 but also because of the relationship between the most prevalent arrhythmia in SND, atrial fibrillation, and SAHS.3
The decrease of bradyarrhythmia in patients with SAHS treated with CPAP is nothing new. Grimm et al4 demonstrated this decrease after CPAP treatment, and Simantirakis et al5 observed a reduction in all rhythm disorders detected by an implantable Holter device in patients with SAHS 6 months after CPAP. In this regard, the interest of our case lies in the complete disappearance of sinus node dysfunction on Holter monitoring with CPAP treatment, making pacemaker implantation unnecessary.
Outcomes as spectacular as those seen in this patient may only occur in sinus node dysfunction of extremely short evolution, with little electrical repercussion on the atrium. In fact, the patient's stress test one and a half years before consultation in our department showed normal sinus function. In patients with SAHS of longer evolution with greater atrial electric disease, any regression may be only partial or may require longer CPAP treatment to produce positive electrical remodeling.
Lastly, as a practical recommendation, patients with asymptomatic SND should be tested for the possible coexistence of SAHS, since treatment of this condition could improve SND, thus avoiding future pacemaker placement .