Measurement of natriuretic peptides may be recommended prior to echocardiography in patients with suspected heart failure. Cut-off point for heart failure diagnosis in primary care is not well established. We aimed to assess the optimal diagnostic cut-off value of N-terminal pro-B-type natriuretic peptide on a community population attended in primary care.
MethodsProspective diagnostic accuracy study of a rapid point-of-care N-terminal pro-B-type natriuretic peptide test in a primary healthcare centre. Consecutive patients referred by their general practitioners to echocardiography due to suspected heart failure were included. Clinical history and physical examination based on Framingham criteria, electrocardiogram, chest X-ray, N-terminal pro-B-type natriuretic peptide measurement and echocardiogram were performed. Heart failure diagnosis was made by a cardiologist blinded to N-terminal pro-B-type natriuretic peptide value, using the European Society of Cardiology diagnosis criteria (clinical and echocardiographic data).
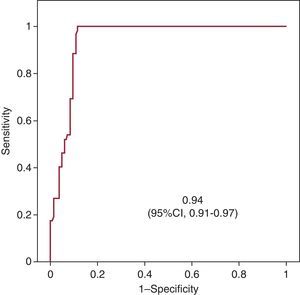
ResultsOf 220 patients evaluated (65.5% women; median 74 years [interquartile range 67-81]). Heart failure diagnosis was confirmed in 52 patients (23.6%), 16 (30.8%) with left ventricular ejection fraction <50% (39.6 [5.1]%). Median values of N-terminal pro-B-type natriuretic peptide were 715 pg/mL [interquartile range 510.5-1575] and 77.5 pg/mL [interquartile range 58-179.75] for patients with and without heart failure respectively. The best cut-off point was 280 pg/mL, with a receiver operating characteristic curve of 0.94 (95% confidence interval, 0.91-0.97). Six patients with heart failure diagnosis (11.5%) had N-terminal pro-B-type natriuretic peptide values <400 pg/mL. Measurement of natriuretic peptides would avoid 67% of requested echocardiograms.
ConclusionsIn a community population attended in primary care, the best cut-off point of N-terminal pro-B-type natriuretic peptide to rule out heart failure was 280 pg/mL. N-terminal pro-B-type natriuretic peptide measurement improve work-out diagnosys and could be cost-effectiveness.
Keywords
.
IntroductionThe prevalence of heart failure (HF) and its associated morbidity and mortality has increased exponentially over recent decades. A prompt diagnosis considerably improves the prognosis of HF,1 but it can be difficult to establish in disease stages showing few symptoms, in which clinical criteria have little specificity. Diagnostic errors are common when the evaluation is based solely on the patient's signs and symptoms, and in primary care HF is erroneously diagnosed in up to 40% of cases.2 Furthermore, the initial diagnosis is only confirmed by echocardiography in one third of patients, and more than half the diagnoses of HF are made without evidence of ventricular dysfunction.3.
The most widely used additional objective examination to investigate ventricular function in primary care is Doppler echocardiography. Nonetheless, this valuable test is not accessible to all physicians in our setting and it is often performed after a considerable delay,4 which further contributes to delaying the final assessment of the clinical picture..
Thus, it is evident that other elements are needed to optimize the diagnostic algorithm of HF, which is based on an appropriate clinical history and physical examination, analyses to rule out triggering factors, and an electrocardiogram (ECG), and thereby to improve the efficiency of echocardiographic study in primary care. Currently, a fast, simple test is available to facilitate the clinical evaluation: determination of natriuretic peptides (B-type natriuretic peptide [BNP] and its N-terminal fraction [NT-proBNP]) in venous blood or urine.5 These biomarkers enable selection of patients who should undergo a confirmatory echocardiography study and allow reasonable exclusion of the initial suspected HF diagnosis in others..
Natriuretic peptides are hormones with diuretic and vasodilator effects, mainly secreted in the left ventricle as a mechanism to compensate for pressure overload. Concentrations of this biomarker are increased in patients with HF6 and in other structural heart diseases such as valve disease and atrial fibrillation.7 Age, deteriorated renal function, and certain conditions such as chronic obstructive lung disease are other causes of elevated natriuretic peptide concentrations. In contrast, treatment with diuretics, beta blockers, and inhibitors of the renin-angiotensin-aldosterone axis decrease the plasma concentrations of these substances..
The cut-off points used to rule out HF have been clearly established in emergency rooms and specialized centers, where natriuretic peptides have shown proven value for screening and diagnosing patients with suspected HF because of their high sensitivity and excellent negative predictive value.8 Furthermore, the prognostic utility of urinary peptide has been compared to that of plasma determination in patients with acute HF.9 Nonetheless, there is little available data on the usefulness of natriuretic peptides in primary care in Spain.10 Few studies have assessed the added value of peptides in diagnosing patients with suspected systolic HF or preserved left ventricular ejection fraction (LVEF) in this setting, despite the fact that the test can be carried out in the physician's consulting room and the results obtained in less than 15min. In addition to being advantageous from the diagnostic viewpoint, this biomarker would be cost-effective: unnecessary echocardiography requests could be avoided, thereby reducing cost and delays.11.
The aim of this study was to evaluate the diagnostic utility of a rapid point-of-care test for plasma NT-proBNP determination as a screening element for detecting systolic or diastolic HF in an ambulatory population seen in primary care, to characterize the optimal cut-off point that will enable reasonable exclusion of HF while significantly increasing the post-test probability of having HF according to the sensitivity, specificity and predictive values for detecting ventricular dysfunction, and to assess the cost effectiveness of this test..
Methods Study Design and PopulationThis is an observational, analytical study evaluating a diagnostic test, performed in two primary care centers in the city of Barcelona. The centers are staffed by 28 general practitioners and have a catchment population of 40 000 inhabitants..
All consecutive patients in whom echocardiography was requested by a primary care physician to investigate suspected HF were invited to participate, regardless of their comorbidities or current medical treatment. All the participating general practitioners received information about the study and specific training in the criteria and diagnostic algorithms used in HF. Eight general practitioners did not request any echocardiographic examination during the study period..
We excluded patients with a previous diagnosis of HF or severe valve disease in the digitized clinical history, those included in a home care program, and those who did not give their consent to participate in the study..
ProceduresAll patients eligible for an initial visit with a general practitioner were contacted by telephone to be enrolled. At the initial visit, patients were informed of the characteristics of the study and the following were undertaken: a) a clinical interview that collected the patient's demographic characteristics, baseline clinical data, treatments, and emergency room visits for HF; b) a clinical history, focusing on the Framingham criteria and the patient's functional class; c) a physical examination evaluating signs of HF; d) an ECG; e) chest X-ray, and f) NT-proBNP determination using a rapid point-of-care diagnostic test. In a subsequent contact, patients were referred to the study reference hospital, where Doppler echocardiography was carried out..
The final diagnosis of HF was made by a single cardiologist in the HF unit of the reference hospital to reduce interobserver variation in the diagnosis. The specialist, who was blinded to the NT-proBNP findings, based the assessment on the individual data obtained for each patient in the enrollment visit (clinical history, physical examination, ECG, chest X-ray) and echocardiography to establish the diagnosis, strictly following the criteria of the European Society of Cardiology (ESC). The diagnosis was based on the presence of signs and symptoms of HF and objective evidence of a structural or functional cardiac abnormality at rest..
The NT-proBNP sensitivity, specificity, positive and negative predictive values, and receiver operating characteristic (ROC) curve were then determined, based on the diagnosis of HF made by the cardiologist..
Reading the ElectrocardiogramAll ECGs were performed with a 12-channel system and were interpreted by the general practitioner who carried out the enrollment visit. Specific evaluation was made of rhythm disturbances, the electric axis, intraventricular conduction, enlargement of the cardiac chambers, established necrosis, and repolarization abnormalities. The ECGs were reported as being normal or abnormal, according to whether or not any of these electrocardiographic changes were present..
N-terminal pro-B-type Natriuretic Peptide DeterminationAll patients underwent venous blood extraction, collected in heparinized tubes. NT-proBNP determination was performed on a Cobas h 232® system from Roche Diagnostics, which uses an immunochromatographic reagent strip to obtain quantitative NT-proBNP results in whole blood (150 μL) at point of care. The test results were obtained in 12min. The instrument was calibrated using 1 code chip every 10 measurements. Plasma NT-proBNP values are expressed in pg/mL (analytical range, 60-3000 pg/mL)..
Doppler EchocardiographyEchocardiographic study was carried out with a General Electric Vivid 7® system using a 3.5 MHz transducer; analyses were performed with an EchoPAC®. The cardiologists who performed echocardiography had access to the clinical information included on the referral sheet and were blinded to the patients’ NT-proBNP results..
The following echocardiographic variables were collected: indexed systolic and diastolic cardiac chamber diameters, left ventricular wall thickness, indexed left ventricular mass, left ventricular systolic function parameters (fractional shortening and LVEF calculated by the modified Simpson method) through the apical 4-chamber view, and left ventricular diastolic function parameters by the left ventricular filling curve and tissue Doppler measured in the lateral mitral ring (Sa, Ea, and Aa waves, E/Ea ratio, deceleration time, E/E’ ratio)..
The LVEF was measured in all patients, and systolic ventricular dysfunction was established as LVEF<50%. HF with preserved LVEF was defined based on normal or slightly abnormal (≥50%) LVEF findings with evidence of diastolic dysfunction, defined as abnormal left ventricular relaxation or diastolic rigidity, according to the diagnostic algorithm proposed in the consensus statement of the Heart Failure and Echocardiography Associations of the ESC.12.
The study met the requisites set down in the Declaration of Helsinki and all patients gave written consent for participation..
Statistical AnalysisCategorical values are described as percentages and continuous variables as the mean (standard deviation) or median [interquartile range], depending on whether or not distribution was normal (analyzed with the Kolmogorov-Smirnov test). Differences between the study groups were analyzed with the chi-square test for categorical variables and with the Student t test or Mann-Whitney U test for quantitative variables. The sensitivity, specificity, predictive values, likelihood ratios and ROC curves were calculated using the diagnosis of HF established by the cardiologist blinded to NT-proBNP results as the reference standard. To determine which variables were independently associated with NT-proBNP concentrations, multivariate linear regression analysis was performed (enter method) with NT-proBNP as the dependent variable and age, sex, ECG, body mass index, glomerular filtration rate, HF diagnosis and treatment with renin-angiotensin-aldosterone inhibitors, beta blockers, and loop diuretics. SPSS 12.0 software was used for the data analysis..
Comparison With Other Cut-off PointsWe compared the cut-off considered to be optimal in our study with other cut-off points commonly used in the literature, from the guidelines of the ESC13 and the National Institute for Health and Clinical Excellence (NICE)14; the cut-off recommended by the manufacturer (greater agreement in ambulatory patients)15; and the triple cut-off described by Hildebrandt et al.16 to detect systolic ventricular dysfunction in primary care. To this end, the sensitivity, specificity, and predictive values of these proposed NT-proBNP cut-offs were determined in our population..
ResultsThe enrollment period was January 2007 to June 2009. A total of 221 patients were contacted by telephone and only 1 patient declined to participate. All patients included went to the initial visit, at which time ECG and chest X-ray were performed in those who had not undergone these studies, and echocardiography was performed. Thus, the study included 220 patients (65.5% women), with a median age of 74 [67-81] years. The demographic, clinical, and treatment-related data are depicted in Table 1, which shows a predominance of elderly persons, women, and patients with hypertension. The initial suspected diagnosis of HF was confirmed in 52 patients (23.6%), among whom 16 (30.8%) had systolic ventricular dysfunction with a mean LVEF of 39.6 (5.1)% and 36 (69.2%) had LVEF≥50%, meeting the echocardiographic criteria of HF with preserved LVEF. No patient without HF had depressed LVEF. Patients with a final diagnosis of HF showed relatively few symptoms, were of advanced age, and had high comorbidity (an elevated number had a history of hypertension, atrial fibrillation, renal failure, and obesity). Only 2 patients had a strictly normal ECG (both had positive Framingham criteria), and more than three fourths of patients were already receiving diuretic treatment (Table 1)..
Table 1. Demographic Characteristics, and Clinical and Treatment Data
| Total (n=220) | Final diagnosis HF (n=52) | Final diagnosis no HF (n=168) | P | |
| Age, years | 73.2±19.2 | 76.5±10.3 | 72.2±9.9 | .005 |
| 74 [67-81] | 79 [71-83.75] | 74 [66-80] | ||
| Sex, female | 144 (65.5) | 26 (50) | 118 (70.2) | .007 |
| BMI | 30.4±4.9 | 29.6±5.3 | 30.2±4.8 | .188 |
| Glomerular filtrate | ||||
| >60 mL/min | 168 (76.4) | 30 (57.7) | 138 (82.1) | <.001 |
| 30-60 mL/min | 52 (23.6) | 22 (42.3) | 30 (17.8) | |
| Functional class | ||||
| I | 24 (10.9) | 2 (3.8) | 22 (13) | <.001 |
| II | 190 (86.4) | 44 (84.6) | 146 (87) | |
| III | 6 (2.7) | 6 (11.5) | 0 | |
| Comorbidities | ||||
| Stroke | 26 (11.8) | 8 (4.8) | 18 (34.6) | .362 |
| IHD | 38 (19.3) | 14 (26.9) | 24 (14.2) | .035 |
| Hypertension | 190 (85.6) | 48 (92.3) | 142 (84.5) | .152 |
| Hyperlipidemia | 80 (36.4) | 18 (34.6) | 62 (36.9) | .764 |
| Diabetes | 40 (18.2) | 10 (19.2) | 30 (17.8) | .822 |
| COPD | 26 (11.8) | 8 (15.3) | 18 (10.7) | .362 |
| CA due to AF | 38 (19.3) | 32 (61.5) | 6 (3.6) | <.001 |
| Obesity (BMI>30) | 107 (48.6) | 21 (40.4) | 86 (51.2) | .173 |
| Smoker or ex-smoker | 62 (28.2) | 22 (42.3) | 40 (23.8) | .010 |
| Treatments | ||||
| ACE inhibitors or ARB | 134 (61.5) | 38 (73.1) | 96 (57.1) | .049 |
| Beta blockers | 54 (24.5) | 20 (38.5) | 34 (17.8) | .008 |
| Loop diuretics | 60 (27.3) | 28 (53.9) | 32 (19) | <.001 |
| Thiazide | 60 (27.3) | 14 (26.9) | 46 (27.4) | .948 |
| Spironolactone | 6 (2.7) | 2 (3.8) | 4 (2.4) | .571 |
| Digoxin | 12 (5.4) | 10 (19.2) | 2 (1.2) | .001 |
| Normal ECG | 86 (39.1) | 2 (3.8) | 84 (50) | <.001 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blockers; BMI, body mass index; CA due to AF, complete arrhythmia caused by atrial fibrillation; COPD, chronic obstructive pulmonary disease; HF, heart failure; IHD, ischemic heart disease.
The data express no. (%), median [interquartile range], or mean±standard deviation.
Median NT-proBNP concentration was 715 [510.5-1575] (290-3000) pg/mL in patients with a diagnosis of HF and 77.5 [58-179.75] (32-1741) pg/mL in those in whom the HF diagnosis was not confirmed..
The ROC curve obtained for the diagnosis of HF was 0.94 (95% confidence interval [95%CI] 0.91-0.97) (Figure). The optimal cut-off point of NT-proBNP to rule out HF was 280 pg/mL. None of the patients with a diagnosis of HF presented values lower than this figure, even though many of them were receiving specific treatment (73.1% angiotensin converting enzyme [ACE] inhibitors or angiotensin receptor blockers [ARB], 38.5% beta blockers, and 53.9% loop diuretics)..
Figure. Area under the receiver operating characteristic curve (95% confidence interval) for an N-terminal pro-B-type natriuretic peptide cut-off of 280 pg/mL. 95%CI, 95% confidence interval.
Twenty patients who had NT-proBNP concentrations>280 pg/mL did not receive a diagnosis of HF..
In our series, NT-proBNP values were significantly higher in men, patients older than 75 years, those with a glomerular filtration rate<60mL/min, those with abnormal ECG findings, and patients receiving ACE inhibitors or ARB, with beta blockers and with diuretics (Table 2). On multivariate analysis, HF (P<.001), body mass index (P=.039) and glomerular filtration (P<.001) retained statistical significance..
Table 2. N-terminal Pro-B-type Natriuretic Peptide Concentrations and Clinical Variables
| Total (n=220) | Final diagnosis HF (n=52) | |||
| NT-proBNP, pg/mL | P | NT-proBNP, pg/mL | P | |
| HF | 715 (510.50-1575.25) | <.001 | ||
| No HF | 77.5 (58-179.75) | |||
| Age | ||||
| ≤75 years | 68 (58-294.50) | <.001 | 724 (475-1.254) | .404 |
| >75 years | 216.5 (89.50-688) | 715 (548.25-1610.25) | ||
| Sex | ||||
| Men | 266.5 (62.25-760.25) | <.001 | 739 (477-1228.25) | .714 |
| Women | 92.5 (59-267.50) | 650 (539-1641.75) | ||
| BMI | ||||
| <30 | 126 (59.50-668) | .262 | 1.212 (531-1612) | .021 |
| ≥30 | 114 (59-317) | 588 (419.50-847.50) | ||
| Glomerular filtration | ||||
| ≥60 mL/min | 87 (58.25-225.50) | <.001 | 589 (480.25-1212.75) | .240 |
| <60 mL/min | 599.5 (183.25-1292.75) | 864.5 (550.25-1748.50) | ||
| ACE inhibitors | ||||
| Yes | 198 (73.75-588.50) | <.001 | 650 (474.50-1276.25) | .056 |
| No | 68.5 (58-183.75) | 1.213.5 (550.25-1748.5) | ||
| Beta blockers | ||||
| Yes | 201 (65.75-338) | .021 | 715 (548.25-1292.75) | .573 |
| No | 98.5 (59-302.25) | 755 (434.75-1692.75) | ||
| Loop diuretics | ||||
| Yes | 495.5 (125-760.25) | <.001 | 639 (475.75-1214.25) | .205 |
| No | 88.5 (58.25-225.50) | 1033.5 (535.25-1692.75) | ||
| ECG | ||||
| Normal | 70 (58-155) | <.001 | 739 (521.75-1584.75) | .074 |
| Abnormal | 227.5 (68.25-738) | 419.5 (414-425) | ||
ACE, angiotensin-converting enzyme; BMI, body mass index; ECG, electrocardiogram; HF, heart failure; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
Our cut-off point differs from the values recommended in various clinical practice guidelines (400 pg/mL) and the manufacturer's recommendations (125 pg/mL). Hence, we compared our results with those obtained after applying these NT-proBNP cut-offs to our population. The sensitivity, specificity, and predictive values of our cut-off and the others tested in the individuals in our study are shown in Table 3. In patients with a diagnosis of HF, 6 cases (11.5%) had NT-proBNP values<400 pg/mL (all with atrial fibrillation, receiving ACE inhibitors treatment, and in functional class II) and 57 of those without a diagnosis of HF had NT-proBNP values of >125 pg/mL..
Table 3. Recommended Diagnostic Cut-off Points Applied to Our Population
| Group (cut-off point) | Sensitivity | Specificity | Positive predictive value | Negative predictive value | Positive probability | Negative probability |
| Present study (280 pg/mL) | 1 | 0.88 | 0.72 | 1 | 8.33 | 0 |
| ESC guidelines 2008 13 | ||||||
| NICE guidelines 2010 14 (400 pg/mL) | 0.88 | 0.90 | 0.73 | 0.96 | 8.80 | 0.13 |
| Manufacturer's recommendations (Europe) (125 pg/mL) | 1 | 0.66 | 0.48 | 1 | 2.94 | 0 |
| Hildebrandt et al. 16 (to detect systolic dysfunction) <50 years (50 pg/mL), 50-75 years (75 pg/mL) >75 years (250 pg/mL) | 1 | 0.70 | 0.50 | 1 | 3.33 | 0 |
ESC, European Society of Cardiology; NICE, National Institute for Health and Clinical Excellence.
Lastly, incorporation of natriuretic peptides in the diagnostic algorithm of HF led to improvements in the diagnosis (in patients with NT-proBNP>280 pg/mL, the probability of having HF increased from 23.6% pre-test to more than 72% post-test; positive probability of 8.33) and to more efficient use of additional testing. Echocardiographic study would only have been necessary in 72 patients with NT-proBNP>280 pg/mL vs the 220 initial requests, which represents a saving of 67% of the echocardiograms performed..
DiscussionThis study shows that HF detection in primary care is difficult and complex, involving a high percentage of suspected cases that are ultimately not confirmed. The percentage of patients who received a final diagnosis of HF (23.6%) in our study is somewhat lower than the rates reported elsewhere in this setting, such as the 25% described by Wright et al.17 and the 34% reported by Zaphiriou et al.18 Our results are a reflection of the activity in daily clinical practice in primary care, and the diagnosis of HF was made through confirmation by a cardiologist following assessment of the patients’ symptoms and the additional tests performed..
The median NT-proBNP concentrations in patients with and without HF in our study were 715 [510.5-1575] and 77.5 [58-179.75] pg/mL, respectively. These values differ from those reported by Zaphiriuou et al.,18 who described a median of 1537 [166-21,854] pg/mL in patients with HF and 202 [22-2323] pg/mL in those without HF, and the reported results of Wright et al.,17 with medians of 1300 (1450) and 277 (304.5) pg/mL, respectively. We believe that these disparate results are related to differences in the study designs and the populations included..
It is beyond question that a rapid method for NT-proBNP determination to exclude the diagnosis of HF in the physician's consulting room in 12min is highly useful. In our study, carried out in an ambulatory population seen in primary care, the best NT-proBNP cut-off value to rule out HF was 280 pg/mL (sensitivity, 1; specificity, 0.88; positive predictive value, 0.72; negative predictive value, 1), with an area under the ROC curve of 0.94 [0.91-0.97]. This performance is even better than the results obtained in studies directed toward diagnosing systolic HF alone in ambulatory populations, such as the reports by Fuat et al.19 and Gustafsson et al.,20 with cut-off points for excluding HF of 150 pg/mL (sensitivity, 0.94; specificity, 0.40; positive predictive value, 0.48; negative predictive value, 0.92) and 125 pg/mL (sensitivity, 0.97; specificity, 0.46; positive predictive value, 0.15; negative predictive value 0.99) and areas under the ROC curve of 0.81 and 0.87, respectively. Our study required the consensus echocardiographic criteria of diastolic dysfunction published in 2007, which were not applied in previous studies. If we had not used these criteria, the area under the ROC curve would have been 0.79 and the optimal cut-off would have been lower, close to 100 pg/mL, and very similar to that reported in the primary care studies..
NT-proBNP determination has proven to be useful and accurate for ruling out the diagnosis of systolic HF, and some authors have even proposed different cut-off points depending on the age of the patient.8, 16 It was not our aim to seek cut-offs according to age, but instead to find a rapid point-of-care determination that would reasonably exclude the need for additional tests, regardless of the patient's characteristics. In any case, none of the patients diagnosed with HF presented values below 280 pg/mL independently of their age..
If we had applied other NT-proBNP cut-off points to our population, such as the 400 pg/mL recommended in the ESC and the latest NICE consensus guidelines, 11.5% of final HF diagnoses would have been excluded (false negatives); hence, we believe that the NT-proBNP value to rule out HF should be lower. If, however, we had used the most widely agreed upon cut-off for ambulatory patients (125 pg/mL), there would have been 57 false-positive results instead of the 20 false positives in our study; that is, the false-positive rate would have almost tripled and the negative predictive value would not have changed..
Lastly, the use of natriuretic peptide analysis as a screening element prior to echocardiography in patients with suspected HF attended in primary care can provide support for the initial suspected diagnosis (in our study the pre-test probability of HF was <25% and the post-test probability was close to 75%) and will optimize the decision-making process, by improving accessibility to electrocardiography and reducing health costs. In our case, use of the NT-proBNP cut-off of 280 pg/mL to exclude the diagnosis of HF would have avoided 67% of echocardiographic studies. Taking into consideration that the mean cost of an NT-proBNP determination is less than half the cost of an echocardiogram, we believe that this would be a cost-effective measure that would establish the diagnosis faster. Nonetheless, based on our study, we can only propose this as a hypothesis; further studies designed for this purpose are needed to confirm this idea. Other authors, such as Wright et al.,17 have reported improvements in ambulatory diagnosis of HF by incorporation of natriuretic peptides in the decision algorithm (a 21% diagnostic improvement vs 8% in the group without peptide analysis). Fuat et al.19 avoided 25% of referrals for additional testing, Goode et al.21 avoided 38% of echocardiograms, and Aspromonte et al.22 reported a 31% saving. However, natriuretic peptide determination can never replace echocardiography, which provides data on myocardial morphology and function in addition to confirming the clinically suspected diagnosis of HF..
LimitationsThe main limitation of this study is the fact that the sample could not be stratified by variables such as age, sex, weight, or renal function because of the small number of patients with a final diagnosis of HF. Although the results from recent studies seem to indicate that age would be the only clinically relevant factor for establishing different cut-off points, mainly in systolic HF,8, 13 we did not find differences in NT-proBNP values according to age in patients diagnosed with HF. Second, the final diagnosis of HF was made by a single cardiologist and the decision was not made by consensus with other experts..
ConclusionsThe best NT-proBNP cut-off point to exclude HF in an ambulatory population attended in primary care is 280 pg/mL, which showed an area under the ROC curve of 0.94 (95%CI, 0.91-0.97). Incorporation of natriuretic peptide determination in primary care improves the diagnostic algorithm of HF, selection of patients needing echocardiographic study, and optimization of healthcare resources, in a setting where a high percentage of initially suspected cases of HF are not confirmed due to difficulties in early stages of the diagnostic process. We believe that the cut-off value obtained and the method used are the most useful for our daily clinical practice..
FundingThis study was funded by the XII Ayuda para la Investigación de la Sociedad Catalana de Medicina Familiar y Comunitaria (XII Research Help from the Catalan Society of Family and Community Medicine)..
Conflicts of interestJ.M. Verdú participated as a speaker in a congress and in a doctoral course sponsored by Roche Diagnostics..
J.M. Verdú, M. Domingo and J. Lupón received honoraria from Roche Diagnostics for their participation in writing other manuscripts for a book..
Acknowledgments
The authors would like to thank Aurora Díaz, registered nurse in the Sant Martí de Provençals Primary Care Team, for her generous collaboration in this study..
Received 28 November 2011
Accepted 11 January 2012
Corresponding author: Equip d’Atenció Primària Sant Martí de Provençals, Fluvià 211, 08020 Barcelona, Spain. verdujm@gmail.com