Percutaneous structural heart interventions have rapidly expanded. Currently, most tertiary hospitals perform percutaneous procedures such as transcatheter aortic valve implantation (TAVI), mitral valve repair, left atrial appendage closure, and septal defect closure. In this setting, cardiac imaging plays a fundamental role in preoperative planning, intraoperative echocardiographic monitoring, and postoperative follow-up. For this reason, interventional echocardiographers are integral members of the medical teams involved in these procedures.
Fluoroscopy remains indispensable to any interventional procedure because it allows a wide field of view and visualization of medical devices, but it exposes health care staff to ionizing radiation. Radiation protection and interventional cardiology units addressed this issue some time ago by creating radiation protection systems for interventional cardiologists, providing mandatory courses on radiation protection, and implementing the well-established recommendations of scientific societies.1,2 However, radiation protection strategies for interventional echocardiographers vary significantly from center to center and are often deficient.
Recent publications have shown that radiation exposure among interventional echocardiographers is a major problem.3–5 McNamara et al.4 found that, during edge-to-edge mitral valve repair, radiation exposure per procedure was 10-fold higher among interventional echocardiographers than among interventional cardiologists and sonographers despite the use of protective shields (10.5 vs 0.9μSv, respectively; P<.001). Crowhurst et al.5 found an 82% reduction in the radiation received after the introduction of protective shields.
Given the situation, the Cardiac Imaging Association and the Interventional Cardiology Association of the Spanish Society of Cardiology (SEC) have drawn up the following recommendations with the aim of increasing the safety of interventional echocardiographers.
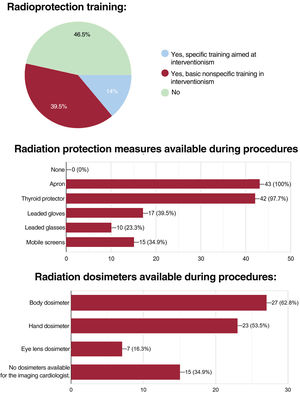
CURRENT STATE OF RADIATION PROTECTION FOR INTERVENTIONAL ECHOCARDIOGRAPHERS IN SPAINTo ascertain the current state of radiation protection strategies in Spain, the SEC Cardiac Imaging Association conducted a survey of interventional echocardiographers. Responses were received from 42 cardiologists working in 33 hospitals across all autonomous communities in Spain. Mean age was 44.4±8.2 years and 58.1% were women. Mean work experience in interventional procedures was 7.7±5.8 years; the number of days the respondents spent per week on procedures was as follows: 1 day (74.4%), 2 days (11.6%), 3 days (11.6%), and 4 days (2.3%). The types of procedures reported were as follows: atrial appendage closure (88%), interatrial defect closure (81%), edge-to-edge mitral valve repair (79%), mitral valve repair (51%), tricuspid valve repair (51%), and aortic valve replacement (42%). The survey showed that there had been limited training in radiation protection and limited access to radiation protection equipment (figure 1). In total, 46.5% had not received training in radiation protection and only 34.9% had access to protective screens. Furthermore, 34.9% of the interventional echocardiographers did not have dosimeters for measuring radiation exposure and those who did have them were largely unaware of the cumulative dose.
Current status of radiation protection for interventional echocardiographers in Spain. Forty-two interventional echocardiographers from 33 centers in Spain participated in the survey. The figure shows the results of questions on radiation protection training and access to radiation protection equipment.
For interventional cardiology personnel, the greatest source of radiation exposure is the radiation scattered from the patients themselves. In general, controlling the dose received by patients also minimizes the dose received by the laboratory personnel. However, protective equipment is needed to keep the occupational dose below the legal limits and as low as reasonably achievable (the ALARA principle).
All personnel working inside laboratories during interventional cardiology procedures are classified as exposed workers, generally category A, and therefore it is mandatory for them to have personal lapel dosimeters (placed under the leaded apron), wrist/ring dosimeters, and eye lens dosimeters.6
Dose limits are established by Spanish Royal Decree 1029/2022, which approved the regulations on protecting health against risks arising from ionizing radiation exposure (table 1).7
Limit of dose from occupational exposure
| Dose magnitude | Occupational dose limit |
|---|---|
| Effective dose | 20 mSv over 1 complete year |
| Equivalent dose to the lens of the eye | 100 mSv over 5 consecutive complete years and a maximum dose of 50 mSv over 1 complete year |
| Equivalent dose to the hands and feet | 500 mSv over 1 complete year |
Interventional cardiologists work in catheterization laboratories on a daily basis. A good approach to monitoring radiation exposure among them is to determine the annual cumulative radiation dose; however, in the case of interventional echocardiographers, this approach may underestimate the real risk of exposure to the repeat high peak spikes to which they are exposed.
Personal protective equipment for interventional cardiology workers includes leaded aprons, thyroid protectors, and leaded glasses and gloves, the main protective equipment being leaded aprons and thyroid protectors.
The use of new composite materials reduces their weight by about 30% over lead vinyl of equivalent thickness. Equivalent lead thicknesses range from 0.25mm to 0.5mm. A good compromise between protection and apron weight is a thickness of 0.35mm with overlap at the front, which provides twice the equivalent thickness. Aprons should be individualized to improve ergonomics and facilitate optimal protection. This is particularly relevant for female workers to ensure adequate protection of the lateral and axillary breast tissue.
In addition to the structural shielding of the room itself, extra shielding is needed, such as suspended or rolling partition screens. Protective screens should be available for interventional cardiologists and imaging cardiologists.8
Other protective items that may be used include disposable curtains and leaded surgical gloves. Disposable protective curtains can reduce the dose received by personnel, but should only be used when they do not interfere with the interventional procedure.
Although leaded surgical gloves reduce the dose received due to radiation scatter by 30% to 40%, they decrease the sensitivity of the hands. In addition, they offer very little protection if the hands are positioned in the direct beam (which should not be done), because this leads to the dose being increased via the automatic dose control of the X-ray equipment. Given they provide a false sense of security, their widespread use is not recommended.1
The International Commission on Radiological Protection (ICRP) reviewed tissue reactions,9 and recommended a significant reduction in the dose received by the eye lens. This recommendation was implemented by European Union legislation in Directive 2013/59/EURATOM,10 which highlighted the relevance of using eye lens protection and monitoring the dose received by the eye lens. In 2018, the ICRP also provided recommendations on radiological protection in interventional procedures.11 Ceiling and floor-mounted screens can provide sufficient protection for personnel positioned behind them, whereas leaded glasses are an alternative for any other personnel remaining in the room. Typically, their thicknesses is equivalent to 0.5mm of lead and should offer sufficient lateral protection.
Dosimeters are integrated in X-ray equipment to monitor the doses received by patients and assist in reducing doses received by personnel. Information from these devices can be transferred to the patients’ dose record. As a minimum, records should be made of the dose area product (Gy/cm2), the air kerma at the procedure reference point (Gy), and fluoroscopy time.
Dose rates are substantially higher during image acquisition than during fluoroscopy; therefore, fluoroscopy time should be minimized and the fewest images per second should be taken to achieve the clinical objective.
Dose reduction can also be enhanced by the correct positioning of X-ray tubes and imaging systems in relation to the patient, using collimation, positioning the personnel inside the room within the low scatter radiation zone, and training personnel in radiation protection (first- and second-level interventional courses).
Finally, personnel should be as far from the X-ray source as possible, because radiation intensity follows the inverse square law: thus, increasing the distance from 40cm to 80cm results in a 4-fold decrease in radiation intensity.
SAFETY CONSIDERATIONS SPECIFIC TO INTERVENTIONAL ECHOCARDIOGRAPHERSThe main consideration concerning radiation protection strategies for interventional echocardiographers is their close proximity to the radiation source. Their position varies according to the characteristics of the center and the procedure to be performed. Based on the potential risk of radiation exposure, procedures can be divided into 3 groups:
- 1.
Procedures with postoperative transthoracic assessment: TAVI.
- 2.
Procedures with transesophageal and fluoroscopic guidance mainly in anteroposterior (AP) or oblique projections of less than 30°. This group includes the following procedures:
- •
Septal defect closure.
- •
Mitral valve repair.
- •
Left atrial appendage closure.
- •
Paravalvular leak closure.
- •
Percutaneous mitral edge-to-edge and tricuspid valve repairs.
- •
- 3.
Procedures with transesophageal and fluoroscopic guidance in oblique projections of more than 30°. This group includes percutaneous repair using the Cardioband device or percutaneous implantation of prostheses other than aortic valve prostheses.
TAVI procedures have been performed for more than 20 years. Increased experience of the procedure has brought about a decrease in its complexity, which has led to TAVI being performed using fluoroscopy alone. Thus, interventional echocardiographers can stay outside the room and, when needed, evaluate the result at the end of the procedure. These procedures carry the lowest risk of radiation exposure and do not require special radiation protection systems.
Procedures with transesophageal and fluoroscopic guidance mainly in AP or oblique projections of less than 30°These procedures comprise the majority of structural interventional procedures. During these procedures, interventional echocardiographers typically position themselves at the patient's side (right or left). Fluoroscopy can be maintained over most of the duration of the procedure in AP or oblique projections of less than 30°, which avoids collisions between the equipment and echocardiographers. Procedures lasting several hours, such as edge-to-edge tricuspid valve repair, present a high risk of radiation exposure in the absence of protective shields. In such procedures, tubes frequently need to be changed to gastric and esophageal positions. In less complex procedures (eg, septal defect closure), there is a significant decrease in the risk of radiation exposure.
Echonavigation systems can significantly reduce the use of fluoroscopy. These systems fuse echocardiographic and X-ray fluoroscopic imaging, thereby increasing anatomical information and reducing the need to use cine loops to provide enhanced radiological detail, as has been demonstrated in patients with congenital heart disease.12
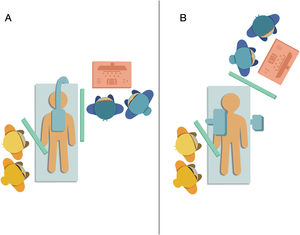
Procedures with transesophageal and fluoroscopic guidance in projections of more than 30°: percutaneous procedures using the Cardioband deviceAn infrequently used type of repair is percutaneous implantation of the Cardioband device (Edwards Lifesciences, United States) for the treatment of tricuspid regurgitation (14% of percutaneous tricuspid procedures according to data from the TriValve registry).13 Such interventions typically begin with interventional echocardiographers beside the patient. This procedure take several hours to perform and involves significant doses of fluoroscopic radiation because of the need for frequent coronary angiograms to assess the potential interference of the device with the coronary artery. In addition, unless protective screens are used, this procedure carries a very high risk of radiation exposure; moreover, even when they are used, risk remains high due to repeated collisions between fluoroscopy tubes and screens, which may eventually lead to the procedure being abandoned. During these procedures, it is beneficial to change the position of fluoroscopes and interventional echocardiographers to avoid repeated collisions and optimize radiation protection (figure 2).
Positions of interventional echocardiographers in the catheterization laboratory. In procedures with oblique projections of less than 30°, interventional echocardiographers can be positioned beside the patient (A). However, the tube is in constant movement in procedures using Cardioband devices (Edwards Lifesciences, United States), and so it would be easier to work by changing the position of the fluoroscope and ultrasound arms (B). Figure created by Helena Capellades.
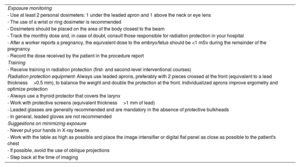
The recommendations for the radiological protection of interventional echocardiographers are summarized in table 2.
Recommendations for radiation protection among interventional echocardiographers
| Exposure monitoring |
| - Use at least 2 personal dosimeters: 1 under the leaded apron and 1 above the neck or eye lens |
| - The use of a wrist or ring dosimeter is recommended |
| - Dosimeters should be placed on the area of the body closest to the beam |
| - Track the monthly dose and, in case of doubt, consult those responsible for radiation protection in your hospital |
| - After a worker reports a pregnancy, the equivalent dose to the embryo/fetus should be <1 mSv during the remainder of the pregnancy |
| - Record the dose received by the patient in the procedure report |
| Training |
| - Receive training in radiation protection (first- and second-level interventional courses) |
| Radiation protection equipment- Always use leaded aprons, preferably with 2 pieces crossed at the front (equivalent to a lead thickness>0.5 mm), to balance the weight and double the protection at the front. Individualized aprons improve ergometry and optimize protection |
| - Always use a thyroid protector that covers the larynx |
| - Work with protective screens (equivalent thickness>1 mm of lead) |
| - Leaded glasses are generally recommended and are mandatory in the absence of protective bulkheads |
| - In general, leaded gloves are not recommended |
| Suggestions on minimizing exposure |
| - Never put your hands in X-ray beams |
| - Work with the table as high as possible and place the image intensifier or digital flat panel as close as possible to the patient's chest |
| - If possible, avoid the use of oblique projections |
| - Step back at the time of imaging |
Interventional cardiology procedures should be performed in an environment that is radiologically safe for both patients and health care personnel. This Spanish national survey shows that interventional echocardiographers are exposed to inadequate radiation protection. These groundbreaking recommendations highlight the relevance of completing radiation protection training and having adequate radiation protection equipment and dosimeters available to increase the safety of interventional echocardiographers.
FUNDINGNone declared.
CONFLICTS OF INTERESTNone declared.
.
We thank Helena Capellades for her artistic skills in the creation of figure 2.