To the Editor,
Ischemic heart disease is one of the leading causes of morbidity and mortality in adults. However, it is uncommon in children and presentation is usually atypical due to a different underlying disease entity. This can lead to diagnostic errors, delay appropriate treatment and increase vital risk.1
Our case shows how a systemic disease and an anatomical variation, both of which are low risk in isolation and relatively common, can lead to a potentially fatal situation when they occur simultaneously.
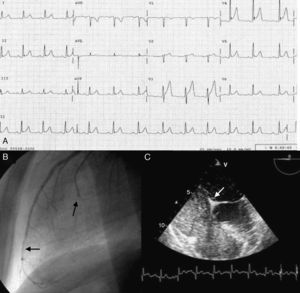
We describe the case of 13-year-old boy who was admitted to the emergency department of our hospital with a symptom of oppressive central chest pain of 6 hours’ duration which began while resting. The initial electrocardiogram showed mild ST-segment elevation in multiple leads, more striking in the precordials, and which was interpreted as early repolarization (Figure 1A); troponin T and creatine kinase levels were elevated (0.9μg/dL and 315mg/dL, respectively).
Figure 1. A: electrocardiogram; poor R wave progression in V2, mild ST-segment elevation more marked in V3-V4 with peaked T wave; B: coronary angiography; C: contrast transesophageal echocardiogram.
The patient was previously asymptomatic and the only family history of note were 3 previous episodes of deep vein thrombosis (DVT) in his father and a negative thrombophilia screen conducted 10 years previously.
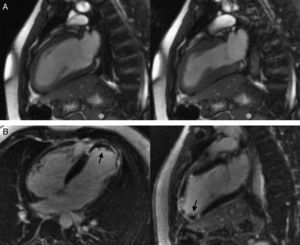
Given the initial suspicion of acute myopericarditis, a transthoracic echocardiogram was performed that only identified a patent foramen ovale (PFO). As the patient remained completely asymptomatic after conventional analgesia, cardiac magnetic resonance imaging was performed to confirm the initial suspicion (8h after the onset of symptoms). Late gadolinium enhancement with an ischemic-related pattern (subendocardial) showed severe apical and anterior apical hypokinesia (Figure 2A) of the left ventricle in the same areas (Figure 2B), leading to the diagnosis of acute myocardial infarction (AMI). An apical thrombus was also detected.
Figure 2. Cardiac magnetic resonance imaging.
Nine hours after symptom onset an urgent coronary angiography was performed showing thrombotic occlusions of the distal anterior descending artery and the first diagonal branch (Figure 1B, arrows). Both thrombi were successfully aspirated using an aspiration catheter (Pronto®; Vascular Solutions, Minneapolis, United States).
Subsequently, the PFO was studied by transesophageal echocardiography. The Valsalva maneuver led to a strong right-left shunt (Figure 1C). The leading causes of AMI in children were ruled out: anomalous origin of the coronary artery, mediastinal tumors and drug abuse. Platelet function and coagulation factors were analyzed and a heterozygous prothrombin G20210A mutation was detected. Other studies were negative (factor V Leiden mutation, antithrombin III, antiphospholipid syndrome, etc.).2
Heterozygotes for this mutation present elevated prothrombin levels, which increase protein S inhibition, an activated protein C cofactor; there is also a reduction of protein C-independent anticoagulant activity. This favors the appearance of DVT.3
Given the diagnosis of AMI probably secondary to vein thrombosis with paradoxical embolism and thrombus in the ventricular apex, we initially maintained the patient under anticoagulation therapy with unfractionated heparin and with acenocoumarol at discharge.
Although DVT was not detected and a control MRI showed that the apical thrombus had been eliminated, we decided to perform PFO closure to shorten anticoagulant treatment, since this impacts on the quality of life, especially at such a young age, and to prevent new paradoxical embolisms. Six months after the AMI, percutaneous closure was performed using a 25-mm Amplatzer PFO occluder. This allowed us to replace the anticoagulants with antiplatelet agents, based on previous experience with similar cases.1
At 2-year follow-up, the patient remains asymptomatic and has a normal level of activity for his age, with residual mildly depressed systolic function due to non-viable infarcted tissue in the apical region.
The risk caused by this prothrombin polymorphism should not be underestimated as it affects 2%-6% of the general population. Mutations at other levels with a synergetic effect may exist which await description.2
It is important to emphasize that ischemic heart disease should be borne in mind when a child or adolescent is admitted to the emergency department with a symptom of chest pain and an abnormal electrocardiogram, thereby reducing delays in applying the appropriate treatment. An early echocardiogram that shows regional wall motion abnormalities may be the key to establishing the indication for urgent coronary angiography.
.
Corresponding author: ijamat@gmail.com