Patients at high risk of suffering cardiovascular events require medical treatment to optimize their lipid profile. The present analysis evaluates the lipid profiles among Spanish patients receiving statin therapy in the international DYSIS study.
MethodsDYSIS is a multinational cross-sectional study carried out in Canada and Europe (n=22,063). In Spain, 3710 patients treated with statin therapy for at least 3 months were included. We compared data relating to demographic parameters and cardiovascular risk profile.
ResultsComplete lipid profiles of 3617 patients were recorded. Regarding the high cardiovascular risk patients with complete lipid profiles (n=2273), 78.9% had a disorder in at least one of the three main lipid parameters: low-density lipoprotein cholesterol (LDLc), high-density lipoprotein cholesterol (HDLc) and/or triglycerides. LDLc was not within target levels in 61.4% of these high risk patients; HDLc was abnormal in 25.3%, and triglycerides were elevated in 37.8%. Overall, LDLc was outside the target range in 63.1%, and 20.7% (n=668) of those treated with statins were normal for all parameters.
ConclusionsMost patients in this study who received statin therapy, particularly those at high cardiovascular risk, were not at the normal lipid parameter levels according to cardiovascular guidelines. Although it is necessary to wait for the final results of current studies on the use of combined lipid-modifying treatments, the management of lipid levels in Spain still has potential for improvement.
Keywords
Lipid metabolism disorders are one of the main determinants of cardiovascular risk.1 A significant proportion of patients, particularly those with ischemic cardiopathy (IC), metabolic syndrome, type 2 diabetes mellitus (DM), and diverse risk factors, have complex lipid disorders which are not limited to high levels of low-density lipoprotein cholesterol (LDLc) or total cholesterol (TC). These patients also have reduced levels of high density lipoprotein cholesterol (HDLc) and/or high triglyceride (TG) levels.2,3,4 The INTERHEART5 study showed the central role of dyslipidemia as one of the determinants of cardiovascular risk, mainly from myocardial infarction. In our field, Medrano et al6 estimated that dyslipidemia is responsible for 20% of coronary disease cases.
Many clinical trials have shown that treatment aimed at reducing LDLc, especially statins, effectively reduces the risk of cardiovascular disease in patients with a high risk of suffering vascular disease, in particular myocardial infarction.7,8,9 However, even with appropriate levels of LDLc, there is a high residual risk of atherothrombotic complications related to low HDLc and high TG. According to the recommendations of the United States National Cholesterol Education Program (NCEP-ATP III), drug treatment should be started to correct these lipid disorders, especially in high risk cases.10 Epidemiological studies have shown that a 1% reduction in HDLc values leads to a 2% to 3% increase in the risk of IC. Those studies agreed that low HDLc levels represent an independent risk factor for IC.11,12 The United Kingdom Prospective Diabetes Study (UKPDS) showed that an increase in HDLc of 4mg/dL is associated with a 15% decrease in the number of cardiovascular events.13
In Spain, several epidemiological studies have analyzed the prevalence of lipid disorders.14,15 However, there is very little information on persistent dyslipidemia in patients treated with statins.
The present study, the Dyslipidemia International Survey-Spain (DYSIS-Spain), is part of a multinational cross-sectional cohort study (DYSIS) carried out in 11 European countries and Canada,16 with the following aims:
– To estimate the prevalence of persistent lipid disorders (not meeting the target levels of LDLc, TC, HDLc, and TG) in patients treated with statins.
– To describe the cardiovascular risk profile and lipid-lowering treatment of different groups: patients with IC, DM, and patients with a high cardiovascular risk.
– To investigate the predictors of persistent lipid abnormalities.
Data were analyzed from the DYSIS-Spain study, which included a total of 22,063 patients. DYSIS-Spain is a multi-center, non-interventional, observational study performed in 477 Spanish healthcare centers (3710 patients; lipid profile was obtained from 3617 patients and the complete profile from 3225). Only data that was in the patients’ medical records was obtained, and the management of participating patients was not changed. The protocol was approved by the Galicia Ethics Committee. All patients gave their written consent before participating in the study. The protection of personal data was guaranteed and randomized audits were carried out in 1% of the centers to check the data.
DoctorsDoctors were chosen from outpatient departments that included a mean of 7 consecutive patients in the study who met the eligibility criteria. The specialty of the participating doctors was recorded (primary care, internists, cardiologists and endocrinologists).
PatientsPatients were included who were over 45 years of age, had been treated with statins for at least 3 months at the time of the medical visit, and whose lipid profile (for at least one of the 3 lipid parameters) had been documented within the previous 6 months. The data requested in the case report form were obtained from the clinical examination or a review of patient medical records. The data were recorded in a single medical visit. Given the study's observational design, safety assessments were not carried out as part of the protocol.
Documented ParametersParticipating doctors were asked to document the following parameters during the medical visit: sex, age, race, weight, height, and waist circumference. Lipid parameters were taken from the most recent lipid analysis performed during the last 6 months and when the patient had been under treatment with statins for at least 3 months. The following parameters were collected: TC, LDLc, HDLc and TG; in addition, risk factors were documented and a record was made of whether the doctor was from primary care, internal medicine, cardiology, or endocrinology. Patients were defined as diabetic if they had been previously diagnosed, had glycemia ≥126 mg/dL in the last available analysis, or if they were being treated with antidiabetic drugs and/or insulin. High fasting glycemia was defined as glycemia ≥100 mg/dL in the last available analysis. Metabolic syndrome was defined in accordance with the definition of the International Diabetes Federation.17 Waist circumference was measured in a standing position, at the mid-point between the iliac crest and the last rib on the mid-axillary line (cut-off values: ≥102 cm for men and ≥88 cm for women). Patients were defined as hypertensive if they had been previously diagnosed, were under anti-hypertension treatment, or had a blood pressure ≥140/90 mmHg. Current smokers were those who smoked at that time or had given up smoking within the last year, and ex-smokers were those who had given up smoking over 1 year earlier. Patients were considered to have a family history of premature cardiovascular disease if any first-degree relative (parents, brothers or sisters) had suffered early atherosclerotic cardiovascular disease (<55 years old in men and <65 years old in women). Patients were considered to have a sedentary lifestyle if they did not perform regular physical activity (walking for a minimum of 20 to 30min 3 to 4 days per week, or equivalent). Alcohol consumption was recorded as the mean number of units of alcohol per week.
Patient history of cardiovascular disease was recorded: IC (previous myocardial infarction or coronary by-pass, surgery, or percutaneous angioplasty), cerebrovascular disease (previous stroke or transient ischemic attack), peripheral arteriopathy (intermittent claudication with or without revascularization), chronic heart failure (class II-IV of the New York Heart Association [NYHA]).
MedicationThe information regarding chronic medication focused on treatment with statins. The indication was recorded, along with the name of the drug, daily dose taken at the time of the medical visit, and when the last lipid analysis was performed. Furthermore, other lipid-modifying treatments (cholesterol absorption inhibitors, bile acid sequestrants, fibrates, and nicotinic acid) taken at the time of the visit and before the last lipid analysis were recorded. Treatment with anti-hypertensive, anti-diabetic and antiplatelet drugs was also registered.
Data AnalysisThe categorical variables were presented as absolute values and percentages, the continuous variables as means (standard deviation) or medians [interquartile interval].
A multivariate regression analysis was performed to detect predictors of abnormal LDLc, HDLc and TG values. The odds ratio (OR) was adjusted for age, sex, family history of premature cardiovascular disease, tobacco smoking, sedentary lifestyle, alcohol consumption >2 units/week, body mass index ≥30 (obesity), waist circumference >102cm in men and >88cm in women, hypertension, DM, IC, cerebrovascular disease, heart failure, peripheral arteriopathy, blood pressure ≥140/90 mmHg, equivalent to simvastatin 20-40 mg/day compared with simvastatin 10 mg/day, equivalent to simvastatin ≥80 mg/day compared with simvastatin 10 mg/day, ezetimibe, and the doctor's medical specialty. A retrospective selection was used (α=.05) to identify the parameters associated with the dependent variables. All the statistical analyses were two-tailed and significance was set at P<.05. Analysis was carried out with the SAS 9.1 software.
Due to the descriptive aim of the study, a formal test of the hypothesis was not performed. The sub-groups were defined before the study: patients only with IC, only with DM, with DM or IC but without cardiovascular risk ≥5% according to their European Society of Cardiology (ESC) SCORE,1 and patients without DM or CI but with a cardiovascular risk <5%. A post-hoc analysis was performed to assess the differences in patient characteristics and in treatment between the sub-groups.
ResultsOf the 477 participating doctors, 68.8% were from primary care, and 31.2% were specialists (internists, cardiologists and endocrinologists).
Patient Characteristics and Level of RiskThe baseline characteristics are shown in Table 1. Of the 3710 patients, 98.4% were Caucasian, and the mean age was 64.8 years. There were slightly more men (52.7%) and a high prevalence of cardiovascular risk factors. The women (47.2%) were older, and had a higher prevalence of obesity and metabolic syndrome.
Table 1. Patient Characteristics.
| Patients | 3710 |
| Age (years) (media±DE) a | 64.8 (10.1) |
| Caucasian (%) | 98.4 |
| Family history of premature IC (%) | 19.9 |
| Smokers (%) | 18.6 |
| Hypertension (%) | 69 |
| SBP (mm Hg) (media±DE) b | 134.2 (14.5) |
| DBP (mm Hg) (media±DE) c | 78.2 (9.6) |
| Waist circumference (cm) (media±DE) d | 98.3 (12.4) |
| BMI (kg/m2) (media±DE) | 28.9 (4.5) |
| BMI≥30 (kg/m2) (media±DE) | 35.1 |
| Metabolic syndrome (IDF) (%) | 61.2 |
| ESC risk level | |
| High risk (CVD, diabetes and/or risk SCORE ≥5%) (%) | 71.2 |
| CVD (%) | 35.7 |
| Diabetes mellitus | 39 |
| Risk SCORE ≥5% (%) without CVD and diabetes | 11.3 |
| Risk SCORE<5% (%) without CVD and diabetes | 28.8 |
| Lipid parameters | |
| LDLc (mg/dL) (media±DE) e | 119.6 (38.6) |
| HDLc (mg/dL) (media±DE) f | 50.2 (15.4) |
| Total cholesterol (mg/dL) (media±DE) g | 200.7 (46.3) |
| Triglycerides (mg/dL) (mediana [RIQ]) h | 124.6 [98-178] |
BMI, body mass index; IC, ischemic cardiopathy; CVD, cardiovascular disease; DBP, diastolic blood pressure; ESC, European Society of Cardiology; HDLc, high density lipoprotein cholesterol; IDF, International Diabetes Federation; LDLc, low density lipoprotein cholesterol; SBP, systolic blood pressure; RIQ, interquartile interval.
a Data available from 3654 patients.
b Data available from 3702 patients.
c Data available from 3702 patients.
d Data available from 3535 patients.
e Data available from 3504 patients.
f Data available from 3496 patients.
g Data available from 3681 patients.
h Data available from 3612 patients.
Most of the patients (71.2%, with a higher frequency of men) had a risk of ≥5% according to the ESC SCORE, and had been diagnosed with clinical cardiovascular disease or DM.
TreatmentNearly half of the patients (45.7%) were receiving chronic treatment with atorvastatin. The proportion of other statins used is shown in Figure 1A. Most received a moderate-potency statin (equivalent to simvastatin 20-40mg/day) (Figure 1B). Regarding the use of other lipid-lowering drugs, 17.4% were taking ezetimibe, 3.6% fibrates, 0.1% nicotinic acid, and 0.3% resins.
Figure 1. A: percentage of patients receiving baseline treatment with different types of statins. B: potency of the statin dose according to the patients’ cardiovascular risk. *Statin dose: potency 1 is equivalent to simvastatin 5mg/day; potency 2: simvastatin 10mg/day; potency 3: simvastatin 20mg/day; potency 4: simvastatin 40mg/day; potency 5: simvastatin 80mg/day; and potency 6: simvastatin ≥160mg/day.
Lipid DisordersThe lipid parameters were obtained from 3617 patients who had one or more parameters in their medical records; a complete lipid profile was obtained from 3225 of these patients. Despite statin treatment, 68% did not meet TC targets (<200 mg/dL), and 63.1% did not meet LDLc targets (<100 mg/dL in high-risk patients and <120 mg/dL in low-risk patients). High TG levels (≥150 mg/dL) were recorded in 36.8% and low HDLc levels (<40mg/dL in men and <50mg/dL in women) in 23.2% (Table 2).
Table 2. Lipid Abnormalities (Percentage of Patients) According to the European Society of Cardiology in All the Patients.
| Total patientsn=3617 | High risk a n=2574 | CVDn=1321 | Diabetes without CVDn=846 | ESC-SCORE ≥5%n=407 | ESC-SCORE<5%n=1043 | |
| TC outside target levels b | 68 | 65.5 | 56.4 | 70.2 | 85.3 | 74.1 |
| LDLc outside target levels c | 63.1 | 60.7 | 51.3 | 64.7 | 83.2 | 68.9 |
| Low HDLc (<40 mg/dL [men] and 50 m/dL [women]) d | 23.2 | 25.7 | 30.9 | 23.6 | 13.8 | 17 |
| High TG (>150 mg/dL) e | 36.8 | 38.1 | 36.1 | 42.1 | 36.3 | 33.7 |
CVD, cardiovascular disease; ESC: European Society of Cardiology; HDLc, high-density lipoprotein cholesterol; LDLc, low-density lipoprotein cholesterol; TC, total cholesterol; TG, triglycerides.
a High risk: CVD, diabetes, and/or ESC-risk SCORE ≥5%.
b TC ≥200mg/dL in patients with ESC-risk SCORE<5%, and TC ≥180mg/dL in patients with ESC-risk SCORE ≥5%, diabetes and/or CVD; data available for 3594 patients.
c LDLc ≥115mg/dL in patients with ESC risk SCORE<5%, and LDLc ≥100mg/dL in patients with ESC risk SCORE ≥5%, diabetes and/or CVD; data available from 3420 patients.
d Data available from 3346 patients.
e Data available from 3525 patients.
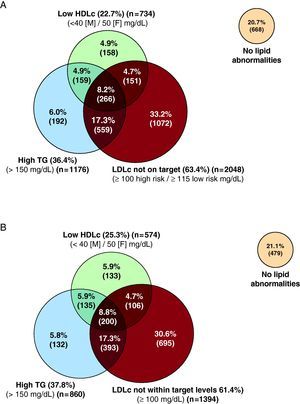
There was a high frequency of combined disorders: 35.1% had 2 or 3 simultaneous lipid disorders, while 8.2% had abnormal levels in the 3 lipid parameters (Figure 2A).
Figure 2. A: individual and combined lipid abnormalities in all the Spanish patients included in the DYSIS study. B: individual and combined lipid abnormalities in the patients with a high cardiovascular risk. Definition of levels of risk in accordance with the European Society of Cardiology; guidelines for the prevention of cardiovascular disease. HDLc, high-density lipoprotein cholesterol; LDLc, low-density lipoprotein cholesterol; F: female; M: male; TG, triglycerides.
Of the 2,273 high-risk patients for whom a complete lipid profile was available, 78.9% had abnormal concentrations of one of the 3 main lipid parameters. Figure 2 summarizes the individual and combined lipid abnormalities of this group (high risk with at least one abnormal level of the lipid parameters). In this group, 61.4% did not achieve the target levels of LDLc, 25.3% were not within the target levels of HDLc, and 37.8% had high TG. As for combined lipid disorders, non-target levels of LDLc, low HDLc, and/or high TG were found in 30.8% of the patients, and target LDLc, low HDLc and/or high TG levels were detected in 17.6% (Figure 2B).
When analyzed by risk sub-groups, the patients with cardiovascular disease showed a better control of lipid parameters, except for HDLc, than the diabetic group or those with an ESC SCORE ≥5% (Table 2).
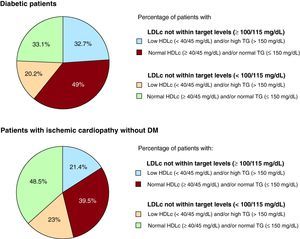
Among the diabetic patients, 33.1% showed no lipid abnormalities, 49% had non-target levels of LDLc with normal concentrations of HDLc and TG, 32.7% had non-target LDLc, low HDLc and/or high TG, and 20.2% had target LDLc and/or low HDLc and/or high TG. Among the patients with IC but without DM, 48.5% showed no lipid alterations, 39.5% had non-target levels of LDLc with normal concentrations of HDLc and TG, 21.4% had non-target LDLc, low HDLc and/or high TG, and 23% had target LDLc and/or low HDLc and/or high TG (Figure 3).
Figure 3. Lipid profile in diabetic patients and in patients with ischemic cardiopathy but with concomitant diabetes mellitus. Data calculated from 1702 Spanish patients with a complete lipid profile (LDLc, HDLc and TG). DM, diabetes mellitus; HDLc, high-density lipoprotein cholesterol; LDLc, low-density lipoprotein cholesterol; TG, triglycerides.
Predictors of Lipid AbnormalitiesThe multivariate analysis identified several variables that were independently associated with abnormal lipid levels (Table 3). Being female, a family history of premature cardiovascular disease, tobacco smoking, a sedentary lifestyle, high alcohol consumption, and blood pressure >140/90mm Hg were independently associated with having non-target levels of LDLc. On the other hand, a history of IC, cerebrovascular disease, and being seen by a specialist were associated with a better control of LDLc and inadequate control of HDLc. Treatment with high doses of statins was associated with a greater control of LDLc levels and low HDLc values. DM was associated with a worse control of HDLc and TG. A family history of premature cardiovascular disease, a sedentary lifestyle, and tobacco smoking were independent risk factors for having abnormal levels in the 3 lipid parameters.
Table 3. Independent Predictors of Abnormalities in High Density Lipoprotein Cholesterol, Low Density Lipoprotein Cholesterol and Triglycerides Levels in Multivariate Logistic Regression Models *
| LDLc outside target levels (≥100/115 mg/dL) | Low HDLc (<40/50 mg/dL) | High TG (>150 mg/dL) | LDLc outside target levels, low HDLc and high TG | |||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age ≥70 years | NS | NS | 0.64 (0.52-0.79) | <.0001 | 0.6 (0.5-0.72) | <.0001 | 0.46 (0.31-0.67) | <.0001 |
| Female | 1.25 (1.03-1.51) | .0211 | NS | NS | 0.64 (0.53-0.76) | <.0001 | NS | NS |
| Family history of premature IC | 1.32 (1.07-1.63) | .0109 | 1.33 (1.06-1.66) | .0123 | 1.31 (1.07-1.59) | .0081 | 1.51 (1.07-2.12) | .0179 |
| Smokers | 1.35 (1.07-1.7) | .0115 | NS | NS | 1.31 (1.07-1.61) | .0105 | 1.77 (1.26-2.49) | .001 |
| Sedentary lifestyle | 1.24 (1.05-1.47) | .0122 | NS | NS | 1.39 (1.18-1.64) | <.0001 | 1.76 (1.28-2.43) | .0005 |
| Alcohol consumption>2 units/week | 1.38 (1.14-1.67) | .0011 | NS | NS | NS | NS | NS | NS |
| BMI>30 (obesity) | 0.76 (0.64-0.91) | .0025 | NS | NS | NS | NS | NS | NS |
| Waist circumference>102 (men) or >88cm (women) | NS | NS | 1.27 (1.05-1.54) | .0144 | 1.43 (1.2-1.69) | <.0001 | NS | NS |
| Hypertension | 0.73 (0.6-0.88) | .0013 | NS | NS | NS | NS | NS | NS |
| Diabetes mellitus | NS | NS | 1.58 (1.31-1.92) | <.0001 | 1.42 (1.21-1.68) | <.0001 | 1.44 (1.06-1.97) | .0208 |
| IC | 0.59 (0.48-0.72) | <.0001 | 1.56 (1.25-1.93) | <.0001 | 0.81 (0.66-0.98) | .035 | NS | NS |
| Cerebrovascular disease | 0.62 (0.45-0.84) | .0024 | 1.54 (1.11-2.14) | .0094 | NS | NS | NS | NS |
| Heart failure | NS | NS | NS | NS | NS | NS | NS | NS |
| Peripheral artery disease | NS | NS | NS | NS | NS | NS | NS | NS |
| 20-40 mg/day equivalent compared with simvastatin 10 mg/day | 0.71 (0.56-0.89) | .0038 | 1.64 (1.23-2.18) | .0007 | NS | NS | NS | NS |
| ≥80 mg/day equivalent compared with simvastatin 10 mg/day | 0.42 (0.31-0.57) | <.0001 | 1.77 (1.24-2.53) | .0018 | NS | NS | NS | NS |
| Ezetimibe | NS | NS | NS | NS | NS | NS | 0.52 (0.3-0.89) | .018 |
| Specialist (cardiologist/endocrinologist/internist/other) | 0.52 (0.43-0.62) | <.0001 | 1.4 (1.15-1.71) | .0009 | NS | NS | 1.4 (1.02-1.92) | .0388 |
BMI, body mass index; CI, confidence interval; HDLc, high-density lipoprotein cholesterol; IC, ischemic cardiopathy; LDLc, low-density lipoprotein cholesterol; NS, non significant; OR, odds ratio; TG, triglycerides.
* The models contain the following variables: age, sex, first-degree relative with history of premature cardiovascular disease, tobacco smoking, sedentary lifestyle, alcohol consumption >2 units/week, BMI≥30 (obesity), waist circumference >102cm in men and >88cm in women, hypertension, diabetes mellitus, IC, cerebrovascular disease, heart failure, peripheral arteriopathy, blood pressure ≥140/90 mmHg (systolic/diastolic), 20-40 vs 10mg/day simvastatin equivalent, ≥ 80 vs 10 mg/day simvastatin equivalent, ezetimibe, and medical specialty. A retrospective selection was made (α=.05).
The results of this extensive study (DYSIS-Spain) show that, despite treatment with statins, only a fifth of patients achieve normal lipid values, or those recommended by current clinical practice guidelines.1,10,11 Furthermore, the large majority of high-risk patients continue to have one or more of the parameters of dyslipidemia.
Although many cross-sectional epidemiological studies have analyzed the prevalence of dyslipidemia in populations with different levels of cardiovascular risk,14,15,18,19,20 this is the first study in Spain to analyze the characteristics of a large cohort of patients with cardiovascular risk treated with statins. Furthermore, previous studies usually focused on LDLc, without performing a more complete analysis of the patients’ lipid profile. In addition to observing that a high proportion of patients do not meet target levels of LDLc, a significant proportion of cases are seen to have low HDLc and high TG. This was seen both when LDLc levels were under control and when they were not, which highlights the importance of trying to improve patients’ overall lipid profile, particularly in high-risk cases.
In recent years, several studies have analyzed the target lipid levels in the general population and among patients in primary care settings.21,22,23,24 In the US NHANES study of 1111 patients with dyslipidemia, 85% had abnormal values of LDLc, HDLc and/or TG; 35% showed more than 2 abnormal lipid levels, while 42% had abnormal values of HDLc and/or TG with or without high LDLc.25
While most studies into dyslipidemia have centered on LDLc in accordance with the recommendations of the NCEP ATP III,26 our study takes a wider perspective and also considers HDLc, TG, and TC values.
Our results show that there is often more than one disturbance in the plasma level of lipids; in the whole group of Spanish patients, 35.1% had 2 or 3 simultaneous abnormalities, and 1 in 12 (8.2%) had 3 abnormal parameters. Furthermore, the presence of other risk factors and comorbidities such as DM and IC lead to a significant increase in the overall cardiovascular risk.
The recommended target lipid levels are achieved more often in patients with clinical cardiovascular disease, and in particular with IC, than in diabetic patients without IC and other high-risk cardiovascular patients (SCORE>5%). However, 78.9% of the high-risk patients included in the study failed to achieve the recommended targets for LDLc, and 38.9% also had abnormal levels of HDLc and/or TG despite lipid-lowering treatment, mainly with statins. It is important to remember what several authors have highlighted with regard to the efficacy of doubling the dose of statins after treatment with an initial dose: this double dose only results in a 6% decrease in LDLc levels, with a slight effect or no effect on HDLc and TG.27,28
We observed a high prevalence of low HDLc and high TG levels in our study. A reciprocal relationship has been described between plasma concentrations of HDLc and the incidence of IC.29,30 The PROCAM cohort confirmed this association, even after adjusting for other risk factors.31,32 Although several studies have observed a linear relationship between levels of TG and the incidence of IC, a multivariate analysis did not confirm this.31 This could be due to the significant biological and analytical variability within and between subjects,33 as well as the high prevalence of additional anomalies in HDLc and LDLc levels.6 However, in accordance with the recent consensus on the management of dyslipidemia in high-risk patients, treatment to raise HDLc and lower TG is classified as having secondary importance.7
The multivariate analysis identified numerous variables associated with one or more lipid abnormalities. Tobacco smoking, a sedentary lifestyle, and an increase in waist circumference were associated with poor control of at least one of the 4 lipid abnormalities analyzed. Although DM was associated with target levels of LDLc being achieved more often, nearly two-thirds of diabetic patients did not achieve them. Furthermore, there was a significant association between DM and a worse control of HDLc and TG levels. These findings are not uncommon in diabetic patients treated with statins; they often have relatively low levels of LDLc but abnormal HDLc and TG levels.34,35 Although these abnormalities are characteristic of diabetic patients, these results lead us to believe that not all the necessary measures are taken to reduce lipid levels.
In this study, being treated by a specialist was associated with a greater control of LDLc and TG, mainly due to the use of higher doses of statins and the combined use of ezetimibe. The fact that high doses of statins are associated with low HDLc may indicate that the doctor is trying to achieve a greater decrease in LDLc to mitigate the risk from low HDLc levels, the treatment options for which are more limited. In our study, the moderate doses of statins, equivalent to simvastatin at 20 to 40mg/day, were the most commonly used. This factor undoubtedly affects the results. Of the high-risk patients, over 50% were treated with doses equivalent to simvastatim 40 or 80mg/day. Nonetheless, within the international DYSIS study, Spain has more deficient control of LDLc compared with the overall mean values obtained from all the countries involved.16
In the recent 2L Registry, which included patients hospitalized for high-risk cardiovascular events, the mean initial dose of simvastatin used was 25mg/day, and 31mg/day on discharge. In our study, ezetimibe combined with statins was used in 14.7% of patients, compared with 13% in the 2L Registry at the baseline visit.36
We observed a high prevalence of abnormalities in HDLc and TG levels, independent of LDLc levels, in this group of patients treated with statins. Similar data were found in a recent analysis of the NHANES, in which the use of therapy targeting HDLc and TG was <12%.25
Four earlier studies, all focusing on LDLc target levels, analyzed the determinants of lipid control in clinical practice. In the Vascular Protection Registry and Guidelines Oriented Approach to Lipid Lowering,37 which included high-risk outpatients, the factors associated with therapeutic success were: elderly patients, DM, IC, previous angioplasty or coronary surgery, and statins. These results are in agreement with those published by other studies.38,39,40
The DYSIS-Spain study has several strengths and limitations. It is a cross-sectional observational study including data from the consecutive patients of 477 doctors. Therefore, it provides a more representative view of usual clinical practice. However, the participating doctors are particularly motivated and have greater knowledge of lipid-lowering treatments, and this could lead to a higher degree of compliance with the recommended guidelines. Also, it cannot be ruled out that the data from the patients who refused to participate in the study could have affected our results. Furthermore, other variables could be valid predictors of achieving lipid targets. The register in this study does not take into account possible modifications in the lipid-lowering therapy; furthermore, treatment compliance is often worse in “real life” settings.
ConclusionsMost of the patients treated with statins in Spain, especially those with a high cardiovascular risk, do not meet recommended lipid targets and/or have a high frequency of abnormal HDLc and TG levels. The results of the DYSIS-Spain study show that significant differences exist between the recommendations in the guidelines and clinical practice, as well as highlighting the need for a more intensive and integrated management of dyslipidemia in high-risk patients. In particular, in secondary prevention and in diabetic patients, therapy should not focus solely on meeting the targets for TC and LDLc, but also achieving the right levels of TG and HDLc to reduce the risk as much as possible.
FundingThis study received funding from Merck & Co. Inc.
Conflicts of interestDr Gustavo Vitale is employed by Merck, Sharp and Dohme in Spain, and the authors of this article have collaborated with this company as scientific advisers.
Received 18 May 2010
Accepted 22 October 2010
Corresponding author: Servicio de Cardiología y UCC, Hospital Clínico Universitario, Travesía de A Choupana s/n, 15706 Santiago de Compostela, A Coruña, Spain. Jose.ramon.gonzalez.juanatey@sergas.es