After hospitalization, patients are in a transient state of generalized risk for adverse health events, a condition that has been termed post hospital syndrome.1 Almost 1 in 6 patients hospitalized for acute myocardial infarction and 1 in 5 of those admitted for heart failure are readmitted within 30 days of discharge.2 Notably, only 10% and 35% are readmitted for the same diagnosis as that of the original hospitalization, respectively.3 The transience of this period of high vulnerability is reflected by readmission risk that stabilizes around 7 weeks after discharge.4 The challenge is to explain these observations.
Could we be causing indirect harm to patients during hospitalization that contributes to this subsequent syndrome? In the hospital, health professionals try to offer optimal treatment based on their patients’ acute health concerns. However, during this process, patients suddenly find themselves in an environment that can become stressful and perhaps even toxic. In this article, we discuss the possible causes of post hospital syndrome and propose strategies to mitigate this risk.
STRESS FROM DIFFERENT FRONTS: THE ALLOSTATIC OVERLOAD HYPOTHESISAlthough post hospital syndrome, the transient period of generalized risk after hospitalization, is well documented, its etiology is less clear. The hypothesis that it is caused by stress during hospitalization is plausible. Adaptation to and recovery from a stressful situation is known as allostasis, with the main mediators being the hypothalamic-pituitary-adrenal axis and the autonomic nervous system. When a person is faced with a threat, this mechanism modifies hemodynamic and metabolic parameters to induce a “fight or flight” reaction and thus enhances the individual's abilities to face challenges. However, constant and repeated exposure to stress disrupts these allostatic mechanisms, compromising the response capacity of the hypothalamic-pituitary-adrenal axis and the autonomic nervous system when faced with a new threat. This state of inadequate adaptation is known as allostatic overload, and its well documented consequences include deterioration of functional and cognitive capacity and dysfunction of multiple physiologic systems.5
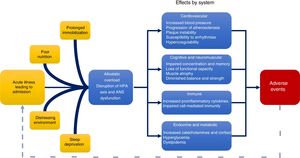
In the context of a hospitalization, patients simultaneously face the physical and mental stress generated by their own illness and the hospital environment. Although the need for hospitalization per se can represent an emotional burden for patients, other potentially modifiable aspects, such as limited mobility, constant sleep disruption, loss of privacy and autonomy, inadequate nutrition, and alarming and unpredictable sounds, are factors that can further contribute to this stress overload and a greater subsequent risk of adverse events (Figure 1).6
Plausible pathophysiology of post hospital syndrome. In addition to the physical and mental stress caused by their underlying disease, hospitalized patients are exposed to environmental stressors such as sleep deprivation, loud and unpredictable noises, poor nutrition, and prolonged periods of limited mobility. These may lead to allostatic overload, with subsequent changes in various physiologic systems. This physiologic dysfunction contributes to the acquired transient risk of adverse events after hospital discharge, including readmission, known as post hospital syndrome. ANS, autonomic nervous system; HPA, hypothalamic-pituitary-adrenal.
The functioning of hospitals may make it difficult to protect patients from stressful experiences. For example, sharing a room with an unknown person may put the patient in a highly stressful situation. Private and sensitive conversations with physicians or nurses may be overheard, and witnessing another person's suffering, worsening condition, or even death can be perceived by patients as ominous and discouraging for their own recovery. Furthermore, shared rooms are associated with a higher risk of health care-associated colonization and infections.7 In addition, a continuously open door with physicians, nurses, or students entering several times daily without properly announcing and identifying themselves can be an affront to privacy at a time of high vulnerability. Moreover, independent individuals may feel stressed by the loss of autonomy over their daily decisions including what to wear and when to eat, bathe, and have visitors.
Insufficient restSleep deprivation during hospitalization may be a major contributor to allostatic overload and disruption of recovery. Falling asleep can be a challenge for hospitalized patients when there are loud and unpredictable noises produced by intravenous infusion pumps, vital signs monitors, health personnel, and other patients. Moreover, it can be even more difficult to maintain a prolonged and restful sleep because of vital signs rounds or blood tests at night or in the early morning. It is thus not surprising that patients report both shorter duration and poorer quality of sleep during hospitalization.8 Taking into account that sleep deprivation causes cardiometabolic alterations (such as worse glycemic control or blood pressure) and cognitive alterations (such as fatigue, daytime hypersomnolence, or delirium), among other physiologic disruptions, this situation can lead to adverse outcomes.9 For example, if lack of sleep is not correctly identified as the triggering factor for disturbance in awareness or worsened blood pressure control, clinicians may decide to adjust treatment or order new tests that ultimately lead to longer hospital stays, a higher risk of adverse drug effects, and greater loss of functional capacity at discharge.
Mobility restrictionsThe design of hospital rooms and treatments (including prolonged intravenous infusions or a Foley catheter) can discourage physical activity. Patients may feel forced to stay in their beds or rooms to avoid missing a physician's visit or diagnostic test, as well as to avoid interfering with the work of the hospital staff. The risks of this restricted physical activity go beyond deep vein thrombosis: it is especially harmful for those susceptible to rapid deterioration of mental and physical function, such as the elderly, causing rapid functional decline with every day of immobility and an increased risk of falls or other adverse events during and after hospitalization.10
Inadequate nutritionSimultaneously, patients face other conditions that generate stress, including poor nutrition during hospitalization. It is not uncommon for patients to have food restrictions while waiting for procedures, even when their scheduling is uncertain, resulting in unnecessarily long fasts. Moreover, a diet that differs from the patient's usual preference (for example, low salt) or unappetizing food presentations can exacerbate the loss of appetite during hospitalization caused by the acute illness or other stressors. All these factors can cause stress and depletion of the metabolic reserves necessary for an adequate hospital and ambulatory recovery, which is reflected by the finding that both malnutrition and poor nutrition during hospitalization are associated with longer stay and mortality.11
STRATEGIES TO IMPROVE PATIENTS’ HOSPITAL EXPERIENCEAfter recognition of the different sources of hospital-related stress, the opportunity arises to design and implement strategies that mitigate this adverse exposure. In this perspective, improving patients’ experience during hospitalization could lead to less stress overload—which may be beneficial in itself—and may also lead to a better and faster recovery. Given that this seems to be a systemic rather than a hospital-specific issue, we propose some strategies to reduce patients’ stress burden while providing the best care possible.
Reduce uncertainty and surprisesEven in the busiest environment, we should be able to take active measures to shield patients from stressful situations and create an environment that is geared to healing. The stress that patients may feel during hospitalization due to the loss of control over, and uncertainty about, their day-to-day situation can be the target of interventions seeking to safeguard each patient's autonomy and privacy. One strategy is to make a daily plan available to patients where they could find a brief but precise description of their clinical status and trajectory during their hospitalization, a schedule with the rounds and procedures planned for the day, and the milestones that need to be met before discharge. This would allow patients to understand their illness, have clear expectations about their recovery, and regain control over their daily activities. In this way, for example, they could plan physical activities outside their rooms without fear of missing physicians’ visits and ensure that family members are present to ask questions when the physician does arrive. Likewise, the simple act of allowing patients to wear their personal clothing instead of hospital gowns allows greater expression of identity and personality, reaffirming that they are being treated as individuals.
Similarly, it is important for patients to know—or find out with ease—the name and function of clinicians in charge of their treatment and every person who enters their room. Simple interventions could be implemented to support this objective, such as displaying the information of the attending physician in a visible place in the room and requiring any staff who enter the room to announce their name and profession with a corresponding record that is available to the patient. As far as possible, individual rooms should be provided to prevent strangers from hearing discussions about private issues and to reduce the risk of transmission of infections.12
Guarantee appropriate conditions for rest and recoverySufficient rest should be considered an essential part of in-hospital treatment. To help patients maintain circadian rhythm and support their cognition, it is important for rooms to have natural light and a clock on which the date is also clearly displayed. Sleep interruptions could be reduced by adopting currently available technologies such as small and comfortable telemetry devices that interfere minimally with sleep and movement, allowing the patient to rest without compromising monitoring needs. Likewise, during the night, efforts should be made to keep noise to the minimum necessary level and avoid taking blood samples or performing other nonurgent interventions. In a nonrandomized study, Milani et al.13 found similar interventions to be associated with a lower risk of rehospitalization at 30 and 90 days after discharge.
Promote physical activity and sufficient caloric intakeA suitable and safe room with a stretcher at the correct height, with steps and support surfaces to aid transfer, is an open invitation for the patient to spontaneously ambulate and maintain independence instead of relying on staff assistance. A safe and effective way to incentivize in-hospital physical activity is to develop an individualized plan by a physical therapy specialist that could extend to outpatient follow-up. It is important for this to be synchronized with adequate caloric intake, considering the catabolic state induced by patients’ acute illness. Early detection of malnutrition or risk of malnutrition in hospitalized patients is essential to design a personalized plan that prevents worsening nutritional status and favors recovery, and there are strategies designed to do this with the assistance of experts in nutrition.14 In addition, it is critical that the presentation, temperature, and taste of hospital food are appealing to the patient. In the elderly, other strategies, such as monitoring food intake and nutritional counseling after discharge, have been associated with a lower risk of rehospitalization.15
Create an individualized plan for outpatient follow-upAnother time of high stress for patients and their families is the transition from hospital to home. New concerns often arise during this period, including lack of adequate knowledge and skills to optimally support the patient in the absence of hospital staff. Therefore, from hospital admission, the family should be invited and encouraged to actively participate in the patient's treatment and decision making. This would imply being flexible with visiting hours and allowing permanent companions, with comfortable spaces available for them. In this respect, the outpatient plan should be discussed in detail before discharge, allowing to ask questions, and creating realistic expectations. The success or failure of a patient's recovery depends on both the follow-up plan and the effectiveness with which this plan has been communicated and codeveloped.
CONCLUSIONThere is evidence suggesting the possibility that we have inadvertently been causing harm to patients through the stress derived from different environmental and social factors during hospitalization. While virtually all medical interventions involve a potential risk of harm, some of this additional stress could be prevented, remedied, and its effects mitigated. We need to see hospitalization through patients’ eyes and employ patient-centered design principles to the way we are organized, conduct our work, and set up the built environment. Therefore, the implementation of interdisciplinary strategies to improve patients’ experience during their hospital stay may help to improve their outcomes. All these efforts would ultimately be aligned with the medical maxim: Primum non nocere.
CONFLICTS OF INTERESTC. Caraballo has no potential conflicts to report. K. Dharmarajan is chief scientific officer at Clover Health, a Medicare Advantage company. H.M. Krumholz was a recipient of a research grant, through Yale, from Medtronic and the US Food and Drug Administration to develop methods for postmarket surveillance of medical devices; is a recipient of research agreements with Medtronic and Johnson & Johnson (Janssen), through Yale, to develop methods of clinical trial data sharing; works under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures that are publicly reported; received payment from the Arnold & Porter Law Firm for work related to the Sanofi clopidogrel litigation and from the Ben C. Martin Law Firm for work related to the Cook IVC filter litigation; chairs a Cardiac Scientific Advisory Board for UnitedHealth; is a participant/participant representative of the IBM Watson Health Life Sciences Board; is a member of the Advisory Boards for Element Science and for Facebook, and the Physician Advisory Board for Aetna; and is the founder of Hugo, a personal health information platform.