Disease progression in patients after a first hospitalization for heart failure (HF), in particular the interaction between survival and rehospitalizations, is not well established.
MethodsWe studied all patients with a first hospitalization and main diagnosis of HF from 2009 to 2013 by analyzing the Minimum Data Set of the Region of Murcia. Both incident and recurrent patients were studied, and the trend in hospitalization rates was calculated by joinpoint regression. Patients were followed-up through their health cards until the end of 2015. Mortality and readmissions, including causes and chronology in relation to the time of death, were assessed.
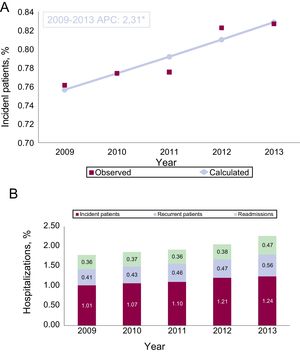
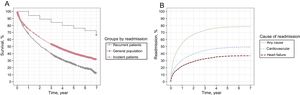
ResultsA total of 8258 incident patients were identified, with annual rates increasing (+2.3%, P <.05) up to 1.24 patients per 1000 inhabitants, representing 71% of hospitalized individuals and 57% of total discharges due to HF. In the first year, 22% were readmitted due to HF, 31% due to cardiovascular causes, and 54% due to any cause. Five-year survival was 40%, which was significantly lower than age- and sex-adjusted expected survival for the general population (76%) (P <.001). Among patients who died during follow-up, readmissions (1.5 per patient/y, 0.4 due to HF) showed a “J” pattern, with 48% of rehospitalizations being concentrated in the last 3 deciles of survival prior to death.
ConclusionsRates of first hospitalization due to HF continue to increase, with high mortality and rehospitalizations during follow-up, which are concentrated mainly in the period prior to death.
Keywords
Hospitalization due to heart failure (HF) is a major health problem of epidemic proportions due to progressive population aging and increasing comorbidities.1 The diagnosis of HF typically begins at the time of hospitalization, but HF progression also involves recurrent hospitalizations. The relevance of HF is shown by the fact that unscheduled admissions account for two-thirds of health care expenditure on HF (2%-5% of the annual health budget)2,3 and are associated with high hospital mortality (around 10%), urgent 30-day readmissions (around 20%),4 and high mid-term mortality rates that are comparable to those of the most prevalent cancers.5
Hospitalization for HF includes incident patients (first admission) and recurrent patients (those with previous admissions) because of the high rate of rehospitalization.6 This distinction is important, given that the action criteria differ. It has been suggested that after a first hospitalization, approximately 50% of patients with a first diagnosis of HF die within 5 years.2 The timeline of hospitalization and its association with mortality is also important because it affects the type of care and preventive measures that have to be implemented. However, data on this issue are scarce. A Canadian study found that rehospitalizations are mainly concentrated in the period prior to death.7
The objective of this work was to describe disease progression in incident patients after a first hospitalization for HF, as well as HF rates, trends, and characteristics, HF readmission profiles, and the interaction between readmission and mortality in the Spanish National Health System.
METHODSStudy PopulationThis study was an observational retrospective cohort study based on the Registry of the Minimum Data Set at Hospital Discharge of the Ministry of Health of the Region of Murcia. The registry is a clinical-administrative database that includes all hospitals (public and private) and more than 97% of hospital discharges with their diagnostic codes. We obtained all discharges with a main diagnosis of HF between 2003 and 2013 (residents in the Region of Murcia, financed by the National Health System in public hospitals of the Health Service of the Region of Murcia or in the contracted hospitals). HF was defined according to the codes in the International Classification of Diseases, Ninth Revision, Clinical Modification8 (398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93 and 428.XX). Elective admissions to public hospitals were excluded as well as mid- to long-term hospitalizations. Patients were identified by the code on their individual health card. During the study period, 91.5% of hospital discharges were assigned to single individuals after their verification via the PERSAN population database, which includes all users of the Murcian Health Service. This process allowed their follow-up in all the hospitals in the network during this period. Of the remaining 8.5%, the individual could not be identified due a missing health care card or an error in the card, and thus follow-up was conducted only by the initial admitting hospital.1 Single “health care episodes” for each individual were created (grouped discharges, transfers between hospitals). The study area was the Region of Murcia, which had a population of 1 472 049 inhabitants according to the official census of 2013.9 It has 9 public general hospitals with good physical access.
Incident Patients and First Hospitalization for Heart FailureIncident patients were defined as those with a first hospitalization for HF from 2009 to 2013 and no hospitalizations in the previous 6 years (2003-2008). This definition was established after assessment of the criteria applied in previous studies, which used periods of 5 years,10,11 4 years,12 and 2 years7 to define incident patients and their first hospitalization for HF. In addition, we used joinpoint regression (version 4.2.0.213) to determine the percentage of new patients vs the total number of patients attended each year. The percentage decreased until 2009, when the trend changed and the slope was no longer statistically significant (Figure of the supplementary material). Consequently, 2009 was considered to be the first year in which incident patients could be consistently identified as those without previous hospitalizations. Patients with previous hospitalizations between 2003 and 2008 and a new hospitalization between 2009 and 2013 were considered to be recurrent patients. Whether incident or recurrent, the first hospitalization between 2009 and 2013 was taken as the index episode. The information for 2009 to 2013 was grouped to make the calculation of survival and time until first readmission more robust.
Study VariablesThe HF index episodes in the period 2009 to 2013 were used to obtain all the demographic and clinical variables available: sex, age, length of stay, hospital mortality, and main diagnosis (reason for admission). Cardiovascular risk factors (diabetes mellitus, hypertension, and dyslipidemia) and those needed to calculate the Elixhauser comorbidity index14 were extracted from the secondary diagnoses.
Readmissions were studied within the entire geographical area, regardless of the hospital where the index episode occurred, and were classified with a main diagnosis of readmission for HF due to cardiovascular causes (diagnostic category >5; Diagnosis-Related Groups, v.2315) and readmission due to any cause. Follow-up was conducted until December 31, 2015. Information on mortality was obtained from the PERSAN registry, which includes discharges from health care due to death, and the National Death Index.16 All rehospitalizations were obtained from the Registry of the Minimum Data Set at Hospital Discharge of the Region of Murcia, which was consulted in March 2017. Information on the population of the Region of Murcia and its mortality rate was obtained from the Regional Center of Statistics of Murcia.9,17 Standardized rates were calculated using the standard European population.18
Statistical AnalysisTrends in hospitalization rates (2009-2013) were determined using joinpoint regression after standardizing the rates (direct method) to eliminate the effect of variations in the population structure (age and sex). An annual percentage change was considered statistically significant if it differed from 0 using a P value <.05. The survival rate of the general population (individuals of the same age and sex as the group of incident patients) was estimated according to observed mortality in the Region of Murcia in 2011.17 Survival was analyzed using Kaplan-Meier curves and Cox regression. Time until first readmission was estimated using the cumulative incidence function and the Fine-Gray regression, considering death as a competing risk. In both cases, patients were only included in the index episode if they were discharged alive. For each patient who died during the follow-up period, survival time from discharge from the index episode to death was divided into 10 equal intervals (deciles of survival). We also determined the decile in which each readmission occurred. This analysis allowed us to establish the timeline of readmissions in relation to survival time.7 All statistical analyses were performed using the SPSS (version 21.0) and R (version 3.4.3) software packages. Competing risks were analyzed using the cmprsk and riskRegression packages of the R software package. A P value of .05 was used as a cutoff for statistical significance.
RESULTSFirst Hospitalization for Heart FailureFrom 2009 to 2013, 9624 patients with hospitalization for HF were identified, of whom 8258 were new or incident patients without previous hospitalizations, and 1366 were recurrent patients, with admissions prior to 2009. The characteristics of the incident and recurrent patients in the index episode during the period 2009 to 2013 are shown in Table 1. Incident patients had lower comorbidity (a low Elixhauser index of < 4 points; 43% vs 29%, P <.001), and a lower prevalence of hypertension, diabetes mellitus, anemia, liver disease, and neurological disease.
Characteristics of the Cohort (Incident Patients and Patients With Previous Admissions)
| Patienta | Total | P | ||
|---|---|---|---|---|
| Recurrent | Incident | |||
| Total, no. | 1366 | 8258 | 9624 | |
| Men, % | 41.90 | 42.70 | 42.60 | NS |
| Women, % | 58.10 | 57.30 | 57.40 | |
| Annual rate/100 000 inhabitants | ||||
| Men | 15.50 | 95.44 | 110.94 | |
| Women | 21.79 | 129.99 | 151.79 | |
| Age group, % | ||||
| 0-44 y | 0.70 | 1.20 | 1.10 | .017 |
| 45-64 y | 8.80 | 9.50 | 9.40 | |
| 65-74 y | 20.50b | 17.40c | 17.80 | |
| 75-84 y | 45.70 | 45.10 | 45.20 | |
| ≥ 85 y | 24.30 | 26.80 | 26.50 | |
| Average age, y (median) | 77.69 (79) | 77.90 (80) | 77.87 (80) | .04 |
| Rates/100 000 inhabitants | ||||
| 0-44 y | 0.22 | 2.15 | 2.37 | |
| 45-64 y | 7.08 | 46.09 | 53.17 | |
| 65-74 y | 53.21 | 272.92 | 326.13 | |
| 75-84 y | 159.84 | 954.92 | 1114.76 | |
| ≥ 85 y | 270.36 | 1802.91 | 2073.26 | |
| Total | 18.62 | 112.58 | 131.2 | |
| Average stay, d (median) | 9.37 (7) | 9.07 (7) | 9.11 (7) | NS |
| Hospital mortality, % | 8.70 | 8.80 | 8.75 | NS |
| Elixhauser index, % | ||||
| 0-3 | 29.1c | 42.7b | 40.8 | .001 |
| 4-5 | 45.5b | 43.0c | 43.4 | |
| Rest | 25.4b | 14.2c | 15.9 | |
| Average | 4.44 | 3.87 | 3.95 | .001 |
| Comorbidities, % | ||||
| Hypertension | 72.60 | 69.80 | 70.20 | .05 |
| Cardiac arrhythmia | 61.90 | 50.70 | 52.30 | <.001 |
| Kidney failure | 32.00 | 22.40 | 23.80 | <.001 |
| Pulmonary vascular disease | 23.40 | 14.90 | 16.10 | <.001 |
| Obesity | 18.40 | 14.60 | 15.20 | <.001 |
| Chronic pulmonary disease | 18.70 | 14.20 | 14.80 | <.001 |
| Uncomplicated diabetes | 16.00 | 12.60 | 13.10 | .001 |
| Anemia due to other abnormalities | 13.60 | 10.70 | 11.10 | .002 |
| Neurological diseases | 5.90 | 7.50 | 7.20 | .043 |
| Peripheral vascular disease | 7.10 | 6.30 | 6.40 | NS |
| Depression | 5.40 | 6.10 | 6.00 | NS |
| Fluid and electrolyte abnormalities | 6.40 | 5.50 | 5.70 | NS |
| Complicated diabetes | 7.20 | 5.20 | 5.50 | .003 |
| Liver disease | 6.40 | 4.40 | 4.70 | .002 |
| Anemia due to blood loss | 3.60 | 2.30 | 2.50 | .005 |
NS, not significant.
The incident patient rate was 1.01/1000 inhabitants in 2009, which increased to 1.24/1000 in 2013. The joinpoint regression analysis of the standardized rates showed an increasing and statistically significant trend (P < .05), with an annual percentage change of 2.3% (Figure 1A). Each year, an average of 1.59 individuals per 1000 inhabitants were admitted for HF, of whom 1.13 were incident patients (71%). The analysis by sex showed that after the age of 74 years, there was a predominance of female incident patients (Table 1 of the supplementary material). Regarding hospitalizations, Figure 1B shows that the increase in hospitalizations in the study period was due to the rates of first admission of new or incident patients, the first admission of recurrent patients, and readmissions for HF in both groups. Each year, there was an average of 1.97 hospitalization episodes for HF per 1000 inhabitants, of which 57% were first hospitalizations of new or incident patients and 43% were rehospitalizations.
A: Standardized rates of incident patients with a first hospitalization for heart failure (per 1000 inhabitants). B: Crude hospitalization rates for heart failure based on the rate of first admission of incident patients and recurrent patients, and the rate of readmissions of both groups (per 1000 inhabitants). APC, annual percentage change (joinpoint regression). * Statistically significant (P < .05).
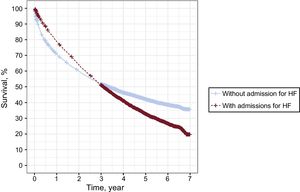
All patients were followed up for at least 2 years, with a maximum follow-up time of 7 years and a median follow-up time of 3.2 years (interquartile range, 1.0-4.8 years). Progress after first hospitalization for HF is shown in Figure 2. At 7 years, the cumulative survival of the incident patients was 33%, which was significantly lower than the expected 67% in the general population of the same age and sex, but was higher than the 14% of the recurrent patients (Figure 2A) (log-rank test, P < .001). Survival was 75%, 94%, and 68% at 1 year and was 40%, 76%, and 25% at 5 years, respectively. Considering death as a competing event, the cumulative probability of readmission at 7 years after the first hospitalization in incident patients (Figure 2B) was 37% for HF, 49% for cardiovascular causes, and 78% for any cause. By the end of the first year, these percentages were 22%, 31%, and 54%, respectively. The best Cox regression model to predict the risk of death included the variables sex, age, Elixhauser index, and mean stay (P < .005). Regarding the risk of readmission, the Fine-Gray regression included age and the Elixhauser index (Table 2 of the supplementary material and Table 3 of the supplementary material). Figure 3 shows that the incident patients who were not readmitted for HF had increased survival at the end of follow-up; however, in the initial period, mortality was higher in this group than in the group with readmissions. Subsequently, the trajectories crossed over. In fact, 58% of the deaths in the group without readmissions occurred in the first 6 months after discharge.
A total of 4368 incident patients died during the follow-up period, involving 7726 years of follow-up (average, 1.8 y/individual). The characteristics of this cohort by need for readmission is shown in Table 2. In total, 84% of the patients had 1 or more readmissions, involving a total of 11867 readmissions. There were an average of 3.2 readmissions per readmitted patient, an average of 1.5 readmissions per year of follow-up in the total group (0.4 for HF), and an average of 26.6 days of hospital stay per individual (15 days per year of follow-up, 4 days of which were for HF). In total, 29% of readmissions were for HF, 13% were due to other cardiovascular causes, and the remaining 58% were due to other causes (Table 4 of the supplementary material).
Characteristics of Patients With and Without Hospital Readmission Who Died During Follow-up After First Hospitalization for Heart Failure
| Readmissions | Total | P | ||
|---|---|---|---|---|
| No | Yes | |||
| Index episode | ||||
| Patients, no. (%) | 690 (15.8) | 3678 (84.2) | 4368 | |
| Women % | 58.3 | 57.3 | 57.4 | NS |
| Age groups, % | <.001 | |||
| 0-44 y | 0.3 | 0.3 | 0.3 | |
| 45-64 y | 3.9 | 5.4 | 5.1 | |
| 65-74 y | 9.1a | 14.0b | 13.2 | |
| 75-84 y | 40.4a | 49.4b | 48.0 | |
| ≥ 85 y | 46.2b | 30.9a | 33.3 | |
| Mean (median) | 82.6 (84) | 80.1 (82) | 80.5 (82) | |
| Hospital stay, d | <.001 | |||
| 0-5 | 28.1 | 31.0 | 30.6 | |
| 6-9 | 30.9a | 36.3b | 35.5 | |
| Rest | 41.0b | 32.6a | 34.0 | |
| Mean (median) | 10.3 (8) | 9.2 (7) | 9.4 (7) | |
| Elixhauser index, % | <.001 | |||
| 0-3 | 44.2b | 36.6a | 37.8 | |
| 4-5 | 42.8 | 45.4 | 45.0 | |
| Rest | 13.0a | 18.1b | 17.3 | |
| Mean (median) | 3.8 (4) | 4.1 (4) | 4.1 (4) | |
| Comorbidity,c% | ||||
| Cardiac arrhythmia | 49.7 | 54.1 | 53.4 | .041 |
| Diabetes without chronic complications | 10.3 | 15.0 | 14.2 | .001 |
| Diabetes with chronic complications | 4.3 | 6.4 | 6.1 | .042 |
| Obesity | 8.8 | 13.1 | 12.4 | .011 |
| Liver disease | 2.6 | 4.9 | 4.5 | .012 |
| Follow-up | ||||
| Total follow-up time, y | 622 | 7.104 | 7.726 | |
| Follow-up y/individual (median) | 0.9 (0.3) | 1.9 (1.6) | 1.8 (1.4) | |
| Follow-up time, no. | ||||
| ≤ 6 mo (27.9%) | 400 | 724 | 1.220 | |
| 7 mo - 1 y (14.3%) | 86 | 633 | 623 | |
| 2 y (20.1%) | 88 | 787 | 876 | |
| 3 y (19.4%) | 52 | 660 | 849 | |
| 4 y (7.5%) | 40 | 425 | 327 | |
| 5 y (6.4%) | 15 | 263 | 279 | |
| ≥ 6 y (4.4%) | 9 | 186 | 194 | |
| Number of readmissions | 11 867 | 11 867 | ||
| Readmissions/individual (interval) | 3.2 (1-38) | 2.7 (0-38) | ||
| Readmissions/y follow-up | 1.7 | 1.5 | ||
| Hospital stay, d | 116 056 | 116 056 | ||
| Hospital stay, d/individual (interval) | 31.6 (1-304) | 26.6 (1-304) | ||
| Hospital stay d/y follow-up | 16.3 | 15.0 | ||
NS, not significant.
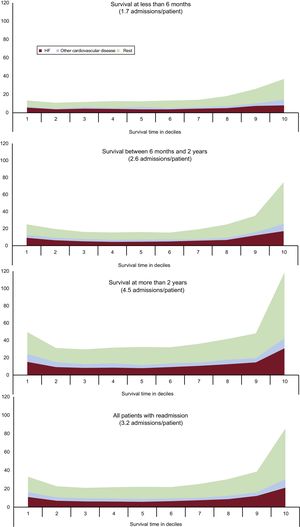
For each individual, survival time between discharge from first hospitalization and death was divided into 10 equal periods or deciles of survival. Figure 4 shows the timeline of readmissions by the decile of survival in which the readmission occurred. In patients with a survival of more than 6 months (20%, each decile represents a maximum of 18 days), 48% of readmissions were concentrated in the last 3 deciles before death.
In patients with a survival between 6 months and 2 years (38%, each decile represents a period of 19 days to 72 days), 51% of readmissions were concentrated in the last 3 deciles before death. In patients surviving more than 2 years (42%, each decile represents a period of 73 days to 255 days), 46% of readmissions were concentrated in the last 3 deciles before death. Overall, 48% of readmissions occurred in the last 3 deciles of survival before death. The respective rates for the first 2 deciles were 14.8%, 17.1%, and 17.9%. Overall, 17.4% of readmissions occurred in the first 2 deciles of survival. The pattern was similar for readmissions for HF and other cardiovascular causes, although the pattern was more difficult to discern due to the lower number of patients. Therefore, readmissions showed a J-shaped pattern in which rehospitalizations were concentrated in the period prior to death (Figure 4).
DISCUSSIONThis study, which focuses on a well-defined population, found an increasing trend in the standardized rate of incident patients with HF, who account for a large percentage of the total number of people admitted for HF (2/3), although their weight in total hospital discharges is lower (1/2). First hospitalization for HF predicts higher mortality during follow-up than in the general population. The pattern of readmissions is determined by survival time and shows a J-shaped pattern with most readmissions being concentrated in the period prior to death.
In most patients, the diagnosis of HF starts at the time of hospitalization, given that this is the most common setting of initial presentation of HF.19 In recent years, a series of studies have shown a decreasing trend in hospitalizations for HF.10,20,21 In this context, the present study provides new Spanish population data, focusing on patient progress after the first hospital admission for HF. To this end, it is better to analyze individuals rather than hospital admission, because the same individual can experience multiple hospitalizations.22
Until now, most studies have addressed hospitalizations without differentiating between incident and recurrent patients. The only population studies of trends in first hospitalizations were conducted in Scotland, Italy (Lombardy), and Denmark. All these studies reported decreasing rates from 1990 to 1996,23 1995 to 2003,12 2005 to 2012,24 and 1995 to 2012,11 respectively. These results are in contrast to those of the present study. The observed rate in our study was lower than published rates. Possible explanations could include socioeconomic differences in the supply and use of health services,24,25 and the inclusion of secondary diagnoses in addition to the principal diagnosis.10,23 The present study only included the principal diagnosis because this option is the most restrictive to avoid incurring misclassification problems that could mask the real trend. Incident and recurrent patients were assessed in the same period, allowing us to determine their relative contribution to total hospitalizations for HF. Only the Lombardy study10 provided data in this regard, showing that incident patients accounted for 59% of patients and 27% of hospitalizations. However, that study used a different methodology, which included patients with cardiomyopathies, without HF, and with secondary diagnoses. Our rates are higher (71% of the patients vs 57% of hospitalizations) because of methodological and socio-health differences, but this aspect should not alter the fact that the problems of both incident and recurrent hospitalizations in our setting have to be addressed. However, high patient mortality, particularly in recurrent patients, means that their relative contribution is maintained over time. Irrespective of these considerations, recurrent patients should be a health care objective, given that they account for approximately half of the entire hospitalization burden.
The other relevant aspect of this study was patient progress after first hospitalization for HF. Five-year survival was 40%, which was half the expected survival in the general population. This percentage shows that the first hospitalization for HF predicts poor prognosis, particularly considering that in-hospital mortality was already 8.8%. Although mortality was not exclusively due to HF, with age and other comorbidities undoubtedly also playing a role, this poor prognosis can be compared with some cancers (lung, colorectal, prostate, and breast), as has already been suggested.5,26
Numerous studies have shown that there is a high risk of readmission in these patients: 67% will be readmitted in the first year after discharge.7,27 In our study, when considering death as a competing risk, the readmission rate was also high (54% in the first year). However, as mentioned by some authors, rehospitalization should be interpreted from the perspective of the patient's survival trajectory in order to implement strategies to address this problem.28 In 2012, Chun et al.7 addressed patient progress after a first hospitalization, and showed that most hospital readmissions occur in 2 periods: the initial period after discharge, and the period immediately before the end-of-life. In an editorial referring to this study, Desai28 proposed a’bimodal’ curve in which readmissions have 3 phases: early readmissions, a plateau, and readmissions before death. We used a similar methodology and found that almost half of readmissions are concentrated in the period before death. As survival time increases beyond 2 years, and therefore severity decreases, the curve becomes J-shaped with readmissions being concentrated in the initial period after discharge and more densely concentrated in the period prior to death. This phenomenon was similar for all causes of readmission. On the other hand, when considering patients without readmission, more than half of the deaths are concentrated in the first 6 months after discharge, suggesting that among this group there is a population whose first admission is also predictive of the risk of early mortality after discharge. Taken together, these findings are relevant for the management of the disease because they highlight the importance of risk stratification at discharge and planning of continuity of care. After discharge, patients with more severe disease die early without the need for readmissions. However, most patients consume hospital resources due to readmission, both early readmission and particularly for end of life care, which entails the need to enhance both ambulatory and domiciliary care. Another aspect of interest is that, of the 15 days of readmission per individual per year, only 4 days were due to HF. Therefore, at a population level, most hospital stays (2/3) are due to causes not directly related to HF, which again supports the need for multidisciplinary care programs for this disease.
LimitationsThe limitations of the present study include those associated with the use of clinical-administrative databases, whose reliability depends on the quality of the clinical information collected and the correct assignment of the diagnostic code. The database used in this study is highly comprehensive, with more than 97% of discharges having diagnostic codes. Other studies have included patients with a secondary diagnosis in addition to a principal diagnosis of HF. However, to estimate the real admission rate for HF, we included only the major diagnoses rather than other less reliable secondary diagnoses. The determination of the period to define the incident patient is a critical decision. We used joinpoint regression to make this decision, whereas other studies decided by convenience and used shorter periods. Regarding the timeline of readmissions, it should be taken into account that not all the patients died during the 7-year follow-up. Thus, the results may be slightly overestimated because the survivors would have less severe disease and a lower risk of readmission.
CONCLUSIONSThe rates of first hospitalization for HF continue to increase and entail a high health care burden. During HF progression, the all-cause mortality rate in the HF population is double the age- and sex-adjusted all-cause mortality rate in the general population. However, after a first hospitalization for HF, these patients also require more hospitalizations, which are typically due to causes other than HF. These rehospitalizations are mainly concentrated in the period before death. This study confirms the need for ambulatory multidisciplinary care, including end-of-life care.
CONFLICTS OF INTERESTNone declared.
- –
Hospitalization for HF entails a high care and social health care burden, but the progress of incident patients with a first hospitalization due to HF has not been determined in the Spanish National Health System, particularly the interaction between survival and rehospitalizations.
- –
The rates of first hospitalization for HF continue to increase in the Spanish National Health System (1.24/1000 inhabitants) and entails a high care burden (71% of patients and 57% of hospitalizations).
- –
After a first hospitalization for HF, the survival rate (40% at 5 years) is half the age- and sex-adjusted rate in the general population, and entails a high need for rehospitalization (in the first year, 54% required readmission for any cause and 22% for HF).
- –
The pattern of readmissions in relation to survival time shows a J-shaped curve, with almost half of readmissions being clustered in the last 3 deciles of survival before death.
We would like to extend our thanks to the health professionals who, by virtue of their labor, made it possible to obtain the information used in the present study.