Differences between European countries in coronary heart disease mortality were initially described in the 20th century, and albeit less dramatic than first reported, these differences remain substantial. Three main hypotheses have been proposed to explain the so-called “Mediterranean paradox”: a) underestimation of coronary heart disease mortality due to methodological flaws; b) the “lag time” hypothesis, and c) the traditional Mediterranean diet and lifestyle. In this manuscript we present and discuss another possible explanation for the Mediterranean paradox related to the higher prevalence and incidence of stable atheromatous plaques in this area.
Keywords
.
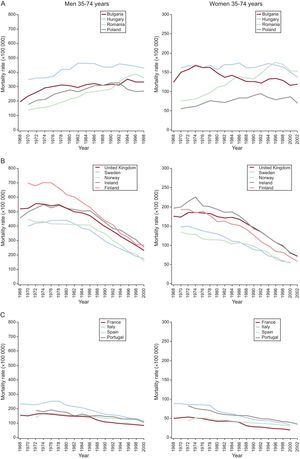
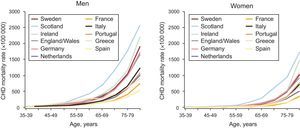
The Southern European ParadoxDifferences between European countries in coronary heart disease (CHD) mortality were initially described in the 20th century. In a comparison of official mortality statistics, it was evident that mortality rates were much lower in Southern European countries than in Northern Europe. At present, the countries in the European region with the highest CHD mortality are Russia and most of the former Soviet Union (Fig. 1A).1 In addition, Northern, Central, and Western European countries have experienced a large decrease in CHD mortality in the last few decades (Fig. 1B).1 However, a substantial difference between the Southern and the Northern and Central European countries is still unexplained, including CHD mortality among the elderly (Figs. 1B, 1C and Fig. 2)2–12.
Coronary heart disease mortality in a selection of European countries: specific rates by 5-year age group (2007). CHD, coronary heart disease. Graph data was obtained from the corresponding National Statistical Institute.2–12.
In 1980, French epidemiologists generated the concept of the “French paradox,” ie, the paradoxical situation in France of a low CHD mortality rate despite a high intake of dietary saturated fat.13 The French paradox was later extended to other European Mediterranean countries such as Spain, Italy, parts of the former Yugoslavia, and Greece, where differences existed in both cardiovascular mortality and the incidence of myocardial infarction (MI) compared to Northern European regions.14,15 These observations have stimulated research during recent years on the role of saturated fat intake in particular, and the Mediterranean diet in general, in the development of CHD.
The Seven Countries Study has provided several relevant observations regarding this apparent paradox. Results for high cholesterol and blood pressure indicated that, although the 25-year relative risk for coronary mortality was similar across different countries, these risk factors were associated with a different absolute risk in Southern Europe compared to the United States and Central or Northern Europe.16,17 Thus, the fundamental difference appears to be in absolute CHD risk, which can differ markedly between countries for a given level of risk factor exposure. These data are consistent with the validity of the recalibration techniques when adapting the Framingham risk function to different regions and countries, supporting the notion that, while the relative risk associated with classical risk factors is similar between these regions, the absolute risk for the same exposure level may differ considerably between countries.18
Three main hypotheses have been proposed to explain the Mediterranean paradox:
- 1.
Underestimation of CHD mortality due to methodological flaws, ie, an excessive proportion of deaths in France attributed to “unspecified causes” could underestimate CHD mortality. However, even after correcting for this potential bias, CHD mortality in France was, in 1992, approximately one-third that of Britain, indicating that undercertification cannot completely explain the observed differences.19
- 2.
The “lag time” hypothesis. It has been proposed that the differences in CHD mortality between Northern and Southern European populations may be due to a late start in the consumption of animal fat and the delayed appearance of raised serum cholesterol concentrations in Southern regions. However, despite increased exposure to animal fat for the last three decades, no CHD epidemic has occurred in Southern European countries. Moreover, some studies indicate that high cholesterol concentrations, smoking, and hypertension are,20 and have been for as long as 40 years now, highly prevalent in Spain without resulting in the predicted increase in CHD events.21
- 3.
The “Mediterranean diet and lifestyle” hypothesis. In the 1950s, Ancel and Margaret Keys published “How to Eat Well and Stay Well the Mediterranean Way,” which encompasses dietary and sociocultural habits common to Mediterranean–specifically Southern European–countries that have been postulated to play a role in this context.22 Initially, the French paradox was attributed at least in part to the consumption of wine (high in polyphenols). However, the Mediterranean diet in general might provide a more comprehensive explanation. Although it varies in different regions, in general it is characterized by high olive oil consumption and low saturated fat intake. Olive oil is rich in oleic acid (55%-80% of total fat), monounsaturated fatty acid and linoleic acid (5%-20% of total fat), polyunsaturated omega-6 fatty acid, and several antioxidants such as polyphenols that could explain the cardiovascular benefits associated with its consumption.
In fact, the PREDIMED controlled clinical trial has already shown that a Mediterranean diet supplemented with virgin olive oil or nuts has a positive effect on cardiovascular risk factors in a high cardiovascular risk population. Compared to the nonintervention low-fat control group, subjects who followed any supplemented Mediterranean diet experienced a decrease in blood pressure,23 insulin resistance, and inflammatory biomarkers23, improved their lipid profile23,24 and increased plasma total antioxidant capacity. In addition, an atherosclerotic lesion regression was observed in the PREDIMED participants with the highest carotid intima-media thickness, measured in the far wall of bilateral common carotid arteries after 1 year.25 The PREDIMED results of the 7-year follow-up for clinical cardiovascular events are expected during 2012. Pointing in the same direction, the Lyon Heart Diet Study showed a decrease in the coronary recurrence rate after a first MI in subjects following a Mediterranean diet, compared to controls.26 Moreover, nonadherence to a Mediterranean diet may lead to high cardiovascular mortality rates even in countries located in the Mediterranean basin.27
Is the lower mortality in Southern Europe due to an increased prevalence of stable atheromatous plaques?A possible explanation for the Southern Mediterranean paradox could be that the population prevalence of coronary artery atherosclerotic lesions would be similar all over Europe but the number of unstable plaques per individual would be higher in Northern and Central European countries, which would result in an increased incidence of acute coronary syndromes in the latter populations.28
Progression beyond the fatty streak stage into advanced atherosclerotic lesions is characterized by subendothelial accumulation of oxidized low-density lipoprotein cholesterol. Oxidized low-density lipoproteins act as a chemotactic factor for circulating monocytes and also as an antigen capable of activating the cellular immune response, leading to the different stages of chronic inflammatory response in CHD.29
Atherosclerotic plaques can be stable, with little predisposition to disruption and hence not commonly leading to acute CHD events, or unstable, which are associated with acute coronary events. Stable plaques are characterized by a dense fibrous cap, a small lipid core, and low-grade inflammation. Unstable or “vulnerable” plaques, on the contrary, have a thin fibrous cap, high lipid content, and high levels of local inflammatory activity. This local inflammation contributes to the degradation of the fibrous layer, facilitating plaque rupture and acute intracoronary thrombosis that can in turn lead to acute coronary occlusion, with subsequent myocardial ischemia and acute myocardial damage.
It could be speculated that despite a comparable atherosclerosis burden in Southern and Northern European populations, atheromatous plaques in subjects in the South could be more stable and therefore less susceptible to fissure or rupture. Some preliminary and indirect evidences suggest that this could be the case:
- 1.
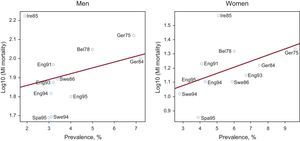
A recent systematic review and meta-analysis using data from 31 countries reported a significant ecological correlation between study-level angina prevalence and country-level MI mortality rates in men and women.30 Thus, it would be expected that countries with higher MI mortality rates would have higher angina prevalence. However, a comparison of European studies with participants of a similar age showed that angina prevalence in Spain is similar to that reported in some Northern European countries with a higher CHD mortality, such as England or Sweden (Fig. 3). This observation suggests that in Mediterranean subjects atherosclerotic lesions may be more stable, yielding the expected number of stable angina cases but a much lower number of major events such as MI.
Figure 3.Association between angina prevalence and myocardial infarction mortality in a selection of European studies with a similar age distribution. Bel78, Belgium 1978; Eng91, England 1991; Eng93, England 1993; Eng94, England 1994; Eng95, England 1995; Ger75, Germany 1975; Ger84, Germany 1984; Ire85, Ireland 1985; MI, myocardial infarction; Spa95, Spain 1995, Swe86, Sweden 1986; Swe94, Sweden 1994. Adapted from Hemingway et al.30
(0.14MB). - 2.
Differences in plasma concentrations of circulating oxidized low-density lipoprotein particles have also been described in Europe. Plasma oxidized low-density lipoproteins levels are a marker of oxidative stress directly implicated in atherosclerotic plaque formation. This marker has been associated with plaque instability and the development of CHD events.31,32 A South-North gradient in plasma concentrations of oxidized low-density lipoproteins has been observed in patients with stable CHD that parallels the incidence and mortality rates of CHD in Europe.33 This finding concurs with the more prolonged postprandial lipidemic state that leads to the higher oxidative status observed in Northern European populations.34 The oxidized low-density lipoprotein gradient does not correlate with a differential level of total cholesterol1 or different use of lipid-lowering therapy in either primary or secondary prevention in Northern and Southern European countries.35,36 However, in CHD patients, higher low-density lipoprotein cholesterol levels and a higher percentage of hyperlipidemia was detected in Southern Europe than in the North.33,36,37
- 3.
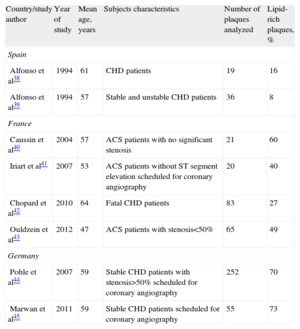
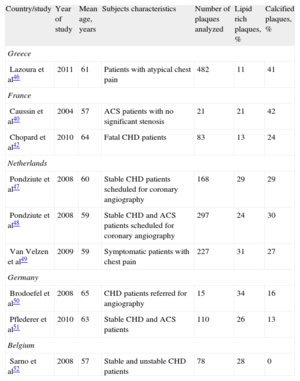
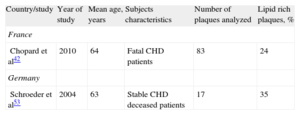
Composition differences in atherosclerotic plaques between European populations have recently been revealed by invasive and noninvasive techniques. Intravascular ultrasound studies in patients with stable and unstable CHD have shown a striking increase in the percentage of lipid-rich plaques from South (8%-16%) to Central (70%-73%) Europe (Table 1).38-45 Computed tomography studies in similar patients point to the same conclusion: an increase in the percentage of lipid-rich plaques from Southern (11%) to Central (34%) European countries (Table 2).40,42,46-52 In addition, two comparable histologic analyses of autopsy plaque samples from CHD patients showed a higher lipid-rich percentage in Germany than in France (Table 3).42,53 Interestingly, while an increasing number of lipid-rich plaques is detected from Southern to Central Europe, an inverse gradient of calcified plaques is found (Table 2). Taking into account that one of the major criteria to classify a plaque as vulnerable is the existence of a thin fibrous cap with a large lipid core, there is preliminary evidence to support a plaque stability gradient in European countries.
Table 1.Percentage of Lipid-rich Atherosclerotic Coronary Plaques in European Countries. Studies Based on Intravascular Ultrasound
Country/study author Year of study Mean age, years Subjects characteristics Number of plaques analyzed Lipid-rich plaques, % Spain Alfonso et al38 1994 61 CHD patients 19 16 Alfonso et al39 1994 57 Stable and unstable CHD patients 36 8 France Caussin et al40 2004 57 ACS patients with no significant stenosis 21 60 Iriart et al41 2007 53 ACS patients without ST segment elevationscheduled for coronary angiography 20 40 Chopard et al42 2010 64 Fatal CHD patients 83 27 Ouldzein et al43 2012 47 ACS patients with stenosis<50% 65 49 Germany Pohle et al44 2007 59 Stable CHD patients with stenosis>50% scheduled for coronary angiography 252 70 Marwan et al45 2011 59 Stable CHD patients scheduled for coronary angiography 55 73 ACS, acute coronary syndrome; CHD, coronary heart disease.
Study selection was based on similarity of subject characteristics and on the plaque classification used (only those studies with the same or a comparable plaque classification were selected).
Table 2.Percentage of Lipid-rich Atherosclerotic Coronary Plaques in European Countries. Studies Based on Coronary Computed Tomography
Country/study Year of study Mean age, years Subjects characteristics Number of plaques analyzed Lipid rich plaques, % Calcified plaques, % Greece Lazoura et al46 2011 61 Patients with atypical chest pain 482 11 41 France Caussin et al40 2004 57 ACS patients with no significant stenosis 21 21 42 Chopard et al42 2010 64 Fatal CHD patients 83 13 24 Netherlands Pondziute et al47 2008 60 Stable CHD patients scheduledfor coronary angiography 168 29 29 Pondziute et al48 2008 59 Stable CHD and ACS patients scheduled for coronary angiography 297 24 30 Van Velzen et al49 2009 59 Symptomatic patients with chest pain 227 31 27 Germany Brodoefel et al50 2008 65 CHD patients referred for angiography 15 34 16 Pflederer et al51 2010 63 Stable CHD and ACS patients 110 26 13 Belgium Sarno et al52 2008 57 Stable and unstable CHD patients 78 28 0 ACS, acute coronary syndrome; CHD, coronary heart disease.
Study selection was based on similarity of subject characteristics and on the plaque classification used (only those studies with the same or a comparable plaque classification were selected).
Table 3.Percentage of Lipid-rich Atherosclerotic Coronary Plaques in European Countries. Studies Based on Histology
Country/study Year of study Mean age, years Subjects characteristics Number of plaques analyzed Lipid rich plaques, % France Chopard et al42 2010 64 Fatal CHD patients 83 24 Germany Schroeder et al53 2004 63 Stable CHD deceased patients 17 35 CHD, coronary heart disease.
Study selection was based on similarity of subject characteristics and on the plaque classification used (only those studies with the same or a comparable plaque classification were selected).
The relatively scanty objective information regarding the reasons for the observed differences in nonfatal and fatal acute MI and coronary death in European countries suggests that CHD in Mediterranean subjects appears to follow a less aggressive course that could be related to the presence of more stable atheromatous plaques. This putative plaque type that would be more common in Southern Europe could be at least in part due to environmental, pharmacologic, and/or genetic factors. Environmental factors would include diet and physical activity, among others. Pharmacologic factors could be related to a different use or response to drugs aimed at stabilizing atheromatous plaques, such as statins. On the other hand, genetic variation among European countries could also explain the increased plaque stability in Southern Europe. Although low genetic differentiation has been described among Europeans, there is a correspondence between genetic and geographic distances within Europe.54 This genetic variation could affect the efficacy of statins to decrease low-density lipoprotein cholesterol and also to stabilize the atheromatous plaque.55
Nevertheless, independently of the cause, atherosclerotic plaque composition needs to be analyzed in well-designed multinational studies that include the countries showing the highest and the lowest CHD death rates in Europe. A multinational study would allow a more realistic comparison of plaque composition characteristics between European countries. The challenge is, however, to study the characteristics of atherosclerotic plaques in large groups of asymptomatic individuals across Europe.56 New advances in imaging techniques such as multidetector computed tomography, which allows a complete plaque characterization with extremely high specificity, might make it possible to study asymptomatic individuals. Multidetector computed tomography rules out atherosclerotic lesions safely, at low radiation exposure (0.88-1.0 mSv).57 Intravascular imaging techniques such as virtual histology, intravascular ultrasound, integrated backscatter intravascular ultrasound, and optical coherence tomography also enable us to observe certain plaque characteristics. However, although optical coherence tomography has much more resolution than intravascular ultrasound and can yield information on inflammation parameters it has not been fully validated to analyze coronary plaques in humans and has important limitations in differentiating lipid-rich and calcified tissue.58,59 But more importantly, intravascular ultrasound and optical coherence tomography are invasive techniques and thus are not suitable to analyze atheromatous plaque characteristics in nonsymptomatic individuals.
Confirmation of the hypothesis proposed here would have a huge impact in primary prevention and management of CHD, as knowing the atherosclerotic plaque composition in each region's population would improve patient treatment and decrease its associated cost.
FundingThis work was supported by the Spanish Ministry of Economy and Innovation through the Carlos III Health Institute and the European Regional Development Found (Red HERACLES RD06/0009, CIBER Epidemiología y Salud Pública), and by the Catalan Research and Technology Innovation Interdepartmental Commission (SGR 1195).
Conflicts of interestNone declared.