Keywords
INTRODUCTION
Ischemic heart disease is the leading cause of death in most of the industrialized countries.1,2 It most typically manifests as chest pain, which is one of the main causes of hospital emergency department (ED) visits. In the USA, over 5 million patients visit the ED each year because of chest pain and a suspected diagnosis of acute coronary syndrome (ACS) produces about 2 million admissions annually.3 The tendency to admit patients is neither particularly efficient or safe. It is inefficient because it generates an annual cost of about 8000 million dollars and ACS is only confirmed in 25% of admissions.4 It is not very safe because 2%-10% of patients with ACS are wrongly sent home from the ED.5 The first chest pain units (CPU) appeared in the eighties with the aim of correcting these problems.6 Their cost-effectiveness7,8 meant they spread rapidly spread in the US.9 Such units may be either functional or structural in design. Units which are structurally designed have their own space and human resources.
On the basis of the evidence in the literature, some Spanish hospitals have incorporated CPUs within the ED.10-12 This study examines activity in one structural CPU and describes the prevalence, demographic and clinical characteristics, and final diagnosis of patients presenting with non-traumatic chest pain. The study also provides data on several care-related quality indicators, as well as providing an estimate of bed space requirements for CPUs.
METHODS
The present prospective study was performed in a tertiary level teaching hospital serving a reference population of 500 000 inhabitants. The emergency department deals with 125 000 emergencies annually between the trauma, surgery, psychiatry, and medicine units.
In June 2002, a CPU was opened within the existing area of the medical emergencies unit. It consisted of 5 cubicles: 3 one-bed cubicles for a first visit and 2 two-bed observation cubicles. A specialist in internal medicine was assigned as the unit's full-time head. A cardiologist was on-call 24 hours a day to attend patients in the CPU as required. Two nurses were assigned to the unit. One of these had previously been in charge of the same 7 cubicles and the other was newly contracted. There were no changes amongst the auxiliary staff.
From the moment the CPU opened, all patients over 18 years of age admitted with non-traumatic chest pain were attended there following the Spanish Society of Cardiology (SEC) guidelines.13 After a first clinical evaluation by the ED physician and ECG, patients are classified according to the initial diagnosis as:
1. ACS with ST-segment elevation (ACSSTE).
2. ACS without ST-segment elevation (ACSNSTE).
3. Possible ACS: patients with a normal ECG or without a diagnosis in whom an ACS cannot be completely ruled out. All of these patients remain in the CPU. Patients are reclassified as ACS, non-ACS, or are referred for further observation based on symptom recurrence, the appearance of new symptoms or changes in the ECG, and on troponin I values. Those in the first group are usually admitted to hospital. If patients in the last group can walk and have an interpretable ECG, an exercise stress test is performed following Bruce's protocol. If patients are unable to walk or if the ECG is inconclusive, an alternative ischemia induction test is scheduled, and the attending cardiologist decides whether to admit on the basis of the results. Patients with a negative stress test are discharged. If the result of the stress test is inconclusive, an alternative test is scheduled and the cardiologist decides whether to discharge or admit the patient.
4. Non-coronary chest pain: when the ED physician has established the final diagnosis, the patient may be discharged, admitted, or moved to the ED observation area.
On completion of the CPU protocol, patients are classified (final diagnosis) as:
1. ACSSTE.
2. Myocardial infarction without elevated ST- segment: those in groups 2 (ACSNSTE) and 3 (possible ACS) with positive troponin.
3. Unstable angina: patient with ACSNSTE and negative troponin, and those in group 3 with a positive stress test.
4. No ACS: patients in group 3 with negative stress test results, and all those in group 4.
5. No diagnosis: patients in group 3 without a stress test or with an indeterminate result.
The first 1000 patients attended in the CPU were included consecutively in the study, as were all other patients attended in the ED over the same period (June 24 to August 27, 2002). Data collected for each patient included age, sex, day, and time of visit, reason for visit, waiting time (time from arrival in the ED to when they were seen by the physician). In the case of patients who were discharged, time spent in the ED was also collected (time from arrival in the ED to discharge).
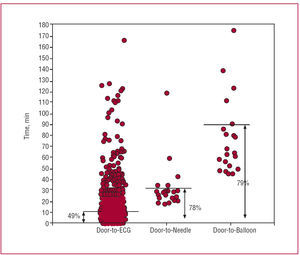
Data on SEC quality of care indicators13 were collected, including door-to-ECG time (time from arrival in ED to ECG) and, when applicable, door-to-needle time (time from arrival in ED to the administration of thrombolytic treatment), and door-to-balloon time (time from arrival in the ED to primary angioplasty). Door-to-stress test time was also collected (time from arrival in ED to performance of stress test).
To determine the appropriate number of beds for a CPU, two calculations were performed. The first took into account the total daily number of patients eventually admitted together with care time (time from arrival in the ED to the decision to admit), and time spent in the ED. The last of these corresponds to care time when a bed is immediately available. However, as beds are not usually immediately available, theoretical delays of 3, 6, and 12 hours over and above actual care time were included. The second estimate was based on the daily total number of patients discharged and time spent in the ED. The calculations were performed for the 75, 90 and 99 percentiles of the distribution of the mean of the variables involved, and for theoretical occupancy rates of 50%, 75%, and 90%. A maximally efficient system was arbitrarily defined as one in which 75% of cases were seen within 3 hours and there was a 90% occupancy rate. A system which could not collapse was defined as one in which 99% of cases were seen within 12 hours and the occupancy rate was 50%. The mean of both calculations was considered to indicate the ideal number of beds. Finally, the number of emergencies per year was divided by the number of beds obtained.
Quantitative and qualitative variables are expressed as mean (range), median (interquartile range), and percentages, respectively. Student's t test for unpaired data was used for between group comparisons using quantitative variables when the data was normally distributed according to the Kolmogorov-Smirnov test. The Kruskal-Wallis test was used when data was not normally distributed, and the χ2 test was used for qualitative variables. A P value less than .05 was considered significant.
RESULTS
A total of 22 468 patients were seen in the ED over the 65 day study period (8 386 of these were seen in the medical emergencies department, which gives a daily mean of 129 [96-161] patients). The mean daily number of patients with chest pain was 15.7 (9-29), giving a prevalence for the period of 4.4% of overall emergencies and 11.9% of medical emergencies.
The characteristics of patients seen for medical reasons are shown in Table 1. When compared with the other patients, those with chest pain were older (55 vs 51 years), included a higher proportion of males (55.6% vs 46.7%), and had higher rates of admission (28.6% vs 20.8%). There were no differences with regard to the time or day of the week on which the visit occurred. Waiting time for patients in the CPU was significantly less than for other patients (median of 10 min vs 34 min, respectively), although the time spent in the ED was similar (medians of 162 and 150 min, respectively).
The initial and final diagnosis and the final destination of patients in the CPU are shown in Figure 1. After the clinical history and first ECG, the initial diagnosis was definitive in almost two-thirds of patients: 48% were classified as non-ACS, 4.9% as ACSSTE and 10.2% as ACSNSTE. Of the 36.9% with a possible ACS, 57.7% (213 patients) were still without diagnosis after monitoring and serial troponin determination, and were candidates for a stress test. This was not performed or did not permit risk stratification in 69 patients (32.4%): this was due to significantly reduced quality of life in 21 patients, to lack of time in 13, and, in 35, an alternative test was required (15 with indeterminate ECG and 10 with functional limitations). On completion of the CPU protocol, 25.9% were diagnosed with ACS (4.9% with ACSSTE, 5% with non-ST-segment elevation myocardial infarction, and 16% with unstable angina), 64.7% without ACS, and 9.4% were still without a final diagnosis. Of those diagnosed with ACS, 12% (31 of 259) were discharged because of the existence of terminal heart disease or another disease which would be fatal in the short term. Overall, the percentage of patients admitted did not exceed 30%.
Figure 1. Distribution of patients with chest pain according to diagnosis. ACS, indicates acute coronary syndrome; ACSSTE, ACS with ST-segment elevation; ACSNSTE, ACS without ST-segment elevation.
No differences by gender were found between patients with and without ACS, although differences expected in terms of risk factors and pain characteristics were observed (Table 2).
In the group without ACS, an anxiety disorder was the most frequent diagnosis (36%). Other diagnoses are shown in Table 3. Seven per cent of these patients were admitted, which is much lower than in the ACS group.
Table 4 shows the results obtained for quality of care indicators based on the initial and final diagnoses. Door-to-ECG time was under 10 minutes for 49% of patients; door-to-needle time was less than 30 minutes in 78% of patients, and door-to-balloon time was under 90 minutes in 79% of cases (Figure 2). The mean door-to-stress test time was 15 hours and 40 minutes, and it was never less than 10 hours.
Figure 2. Distribution of patients attended in the chest pain unit according to different care times used as process quality indicators. The continuous line shows the standard accepted by the SEC and the percentage refers to the number of patients meeting that standard.
Based on these results, the number of beds for a CPU (Table 5) would depend on the point of equilibrium between a system which never became saturated (14 beds to cover 99% of cases, with a waiting time of 12 hours and a 50% occupancy rate) and a maximally efficient system (5.3 beds to cover 75% of cases, with a waiting time of 3 hours and a 90% occupancy rate). The mean was 9.65 beds, which means a requirement of one bed per 12 953 emergencies (125 000/9.65).
DISCUSSION
To date, most of the data used to justify the implementation of CPUs in Spain has come from studies performed in the US.3-9,14 Both economic arguments (reduction in unnecessary admission and avoidance of inappropriate discharges),6-8 and the magnitude of the problem,3 have been used to justify the creation of CPUs. Thus, chest pain has been considered to be one of the most frequent causes of visits to the hospital ED, with figures ranging from 5% to 20%.4 In the present study, using lax inclusion criteria for being seen in the CPU (presence of non-traumatic chest pain, and no other limitations), visits because of chest pain accounted for no more than 5% of all emergency room visits, or 12% of all medical emergencies. This prevalence rate, which had not been studied previously in Spain, is lower than that described previously for studies performed in the USA.3,4 This could be due to differences in the prevalence of heart disease in the 2 countries, to differences in the organization of health care, or to greater awareness in the US of the need to visit the ER when chest pain is present.1,2,9,15 Although the Spanish figures are lower than those for the US, they still represent a substantial number of visits and indicate a need for wider availability of CPUs. The levels of saturation in the majority of hospital EDs16 likewise does not facilitate the rapid identification and management of these patients and, when no CPU is available, they are usually scattered through different departments, and are seen by a range of personnel who are frequently both scarce and have a high workload.
After the clinical history and the first ECG, almost 50% of patients were classified as non-coronary, and had a final diagnosis which would not normally mean being seen by the cardiologist on call. This has been observed previously4,17 and, together with the need for an immediate interpretation of the ECG, make it essential that an experienced emergency doctor is present. In many hospitals in Spain, a cardiologist is not on call 24 hours a day. Even where this is the case they often have to divide their time between the ED and the cardiology department, which makes it impossible for them to be physically present in the ED at all times, or for them to be able to read patients' ECGs as soon as they are available. Thus, only close collaboration between departments will ensure reasonable patient care times.
One major contribution of CPUs in the care of these patients has been the introduction of ischemia induction.9 In Spain, the prognostic validity of conventional stress testing has been demonstrated in selected patients in the CPU.10-12 This type of stress testing is also the most economic, which is of relevance in a system of publicly financed health care with limited resources. However, it is not appropriate in all patients. In the present study, a number of patients had difficulty performing the test or had indeterminate results and therefore required an alternative test. This should be taken into account in future recommendations and protocols. Given increased rates of ischemic heart disease due to the ageing of the population,2 and a lower tolerance for exercise, the number of patients without a diagnosis and risk stratification is likely to increase in the near future. This will create the need for a change of focus. Some protocols already routinely incorporate alternative ischemia induction tests, such as perfusion scintigraphy during or immediately after chest pain18,19 or pharmacological stress echocardiography.19,20
The performance of the CPU as measured using established quality of treatment indicators deserves comment. In 50% of patients with chest pain, the consultation was initiated and an ECG available in under 10 minutes (door-to-ECG time), which is considerably lower than the mean waiting time of 34 minutes for the remaining patients. Nevertheless, as clinical guidelines recommend a time under 10 minutes,12 there is still room for improvement. Although inexperience may have played a part, even under ideal conditions (CPU with sufficient physical space and trained, and motivated staff), meeting the proposed standard constitutes a real challenge in the care of these patients.21 Obtaining an ECG is an essential first step in patients with ACSSTE to determine whether early revascularization is required. From this point of view, the results meet the required standard in almost 80% of cases and are in clear contrast to earlier experiences in which only 70% of these patients were revascularized (without taking into account whether the revascularization was performed within the stipulated time period or not).22 The door-to-needle time was notably lower than that observed previously in studies in Spain,23 though it is not possible to say whether this was due to a beneficial effect of the CPU or to the fibrinolytic treatment administered in the ED.
The SEC estimates that a CPU would require 1-2 beds per 50 000 emergencies attended annually in the ED.13 Our results, however, indicate a need for slightly over 3 beds per 50 000 emergencies attended annually. The main determinants of these needs are waiting time for a stress test and the time the patient has to spend in the ED after admission, due to lack of beds. These characteristics are center-specific and will influence any estimate of the number of beds needed. The American College of Cardiology guidelines on patient evaluation and treatment, aware of the inefficiency implied by the door-to-stress test time, contemplate the possibility that patients be discharged and return within the following 72 hours for a stress test.24 A recently published report described a positive experience with this type of initiative.25 The time patients spend in the ED once the decision to admit has been taken is one of the main reasons for the poor functioning of hospital emergency services26 and deterioration in the quality of care.27 Only a willingness to recognize the problem by all concerned and the adoption of appropriate measures will ease the problem.
Limitations
One limitation of the present study was its external validity. Although the way hospital EDs are organized in Spain is similar, there are differences between them. Nevertheless, regional similarities in the prevalence of risk factors and ischemic heart disease28 make it reasonable to believe that the results reported here be closer to the reality of the situation in Spain than those deriving from studies in countries such as the US, Canada or the UK. Secondly, the use of outcomes indicators such as mortality and the rate of cardiovascular events at 30 days would have been preferable to the process indicators adopted to measure CPU functioning. On the other hand, the true impact of setting up these units should become apparent within a short space of time. Finally, patient diagnoses in the CPU, and the expected distribution of patients with chest pain, was not confirmed by following-up patients. It was not, however, the aim of this study to estimate the validity and precision of the diagnostic protocol, but to establish the percentage of patients occupying each level of the protocol. Future studies should aim to clarify the proportion of patients admitted with ACS in whom the diagnosis is confirmed on discharge. They should also aim to determine the proportion of patients with non-coronary pain who go on to suffer a cardiovascular event.
CONCLUSIONS
This study has provided the first description of the characteristics of patients with non-traumatic chest pain attending a Spanish chest pain unit. Four aspects of the study are worthy of note. Firstly, the prevalence of non-traumatic chest pain in a hospital ED in Spain was found to be slightly less than 5%, and we were able to establish the distribution according to diagnosis using current instruments. Only the clinical history and first ECG were required to diagnose or discount ACS in 50% of patients. The other 50% presented other diagnoses, predominantly anxiety disorders. Up to 10% of patients who completed the CPU protocol did not have an etiological diagnosis due to limitations of using the stress test for risk stratification in the ED. Second, the study showed that care within the ACS process was faster than that for patients without chest pain. Third, in this cohort, males presented more frequently with chest pain than women, although the percentages of males and females diagnosed with ACS was similar. Fourth, using figures obtained in this study it was estimated that the CPU in Spain would require one bed per 13 000 emergencies dealt with annually in a given ED.
ABBREVIATIONS
ACS: acute coronary syndrome
ACSSTE: acute coronary syndrome with ST-segment elevation
ACSNSTE: acute coronary syndrome without ST-segment elevation
CPU: chest pain unit
ED: emergency department
SEC: Spanish Society of Cardiology
Correspondence: Dr. M. Sánchez.
Secció d'Urgències Medicina. Àrea d'Urgències. Hospital Clínic.
Villarroel, 170. 08036 Barcelona. España.
E-mail: msanchez@clinic.ub.es
Received May 8, 2006.
Accepted for publication December 14, 2006.