To the Editor,
Stenosis or obstruction of the superior vena cava (SVC) is a rare complication of surgery to correct sinus venosus (SV) atrial septal defect (ASD) with partial anomalous pulmonary venous drainage (PAPVD). We report 2 cases of adult patients that demonstrate the utility of percutaneous treatment of SVC stenosis after said surgical procedure.
The patients were an 18-year-old man and a 39-year-old woman who underwent surgical correction with tunneling of right superior pulmonary vein in the left atrium by means of pericardial patch, without enlargement of the SVC, 1 year and 11 years ago, respectively. In addition, the woman required implantation of a DDD pacemaker due to symptomatic sinus node dysfunction one year after the surgery. The patients had vascular spiders at the pectoral level, with congestion of the face and neck. Echocardiography and magnetic resonance verified the stenosis of the SVC.
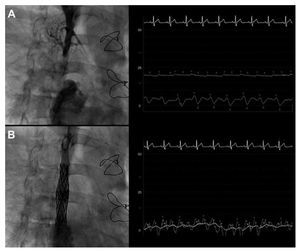
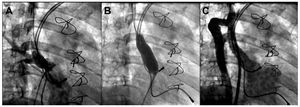
In the case of the 18-year-old man, the cardiac catheterization was carried out by femoral and right jugular venous access, and revealed complete and lengthy obstruction (5 cm) at the level of the SVC where it emptied into the right atrium (Figure 1A). He had a baseline gradient of 15 mm Hg with pressure in the portion proximal to the SVC of 22 mm Hg. For the intervention, a multipurpose guide-wire catheter was introduced via the right jugular vein. A 0.014 Miracle 6 g wire (Abbott Vascular) was passed through the entire obstruction and dilatation was achieved with 2-mm and 4-mm diameter balloons. Right femoral access was employed for dilatation using an 8 mm ´ 40 mm balloon and, finally, 2 overlapping 39-mm CP stents (Numed Inc.) mounted on a 12 mm ´ 40 mm Opta-Pro balloon (Cordis) were implanted. The angiographic results were good, with no residual gradient (Figure 1B). In the case of the woman, who had a DDD pacemaker, stenosis with a minimum diameter of 3 mm (Figure 2A) and a residual gradient of 14 mm Hg were observed. Right femoral access made it possible to pass through the stenosis, and successive dilatations were carried out with 12 mm ´ 40 mm and 18 mm ´ 45 mm balloons (Figure 2B). This resulted in a minimal luminal diameter of 12 mm (Figure 2C) and a residual gradient of 4 mm Hg. To avoid the possibility of a stent trapping the pacemaker leads, no stent was implanted. Both patients were asymptomatic 6 months after their interventions, with no echocardiographic evidence of restenosis.
Figure 1. A: venogram at the level of superior vena cava (SVC) showing a lengthy complete occlusion. On the right, a pressure gradient of 15 mm Hg between SVC and right atrium is observed. B: final angiographic result following implantation of two overlapping stents. The image on the right shows that the gradient has disappeared.
Figure 2. A: venogram at the level of superior vena cava showing severe stenosis at the entrance to right atrium. B: balloon dilatation. C: final angriographic result following dilatation.
The most common etiology of SVC syndrome was classically tumor-related, although in recent years, with the increase in the implantation of pacemakers, defibrillators, etc., iatrogenesis secondary to these devices is the major cause.1 Stenosis of the SV is an infrequent complication of surgical repair of a SV type ASD with PAPVD. It can occur immediately after surgery because of the space occupied by the patch that redirects the pulmonary veins to the left atrium, especially in the case of a small-caliber vena cava, such as that of the man we describe here and who, moreover, had a persistent left superior vena cava. In the case of the woman, the pacemaker leads may have played a role in the development of the stenosis.
Tzifa et al1 published a series of 63 patients with SVC obstruction of differing etiology in which the initial hemodynamic results were satisfactory in 100% of the cases treated with stent and in 78% of those treated by means of balloon angioplasty, although, over the long term there were no differences between the 2 modalities of percutaneous treatment. Nicolae et al2 reported a case of an adult patient with SVC stenosis after surgery for SV type ASD and PAPVD treated successfully by means of stent implantation.
In conclusion, these two cases demonstrated that percutaneous treatment can be a valid alternative to surgery in cases of SVC obstruction following surgery for SV type ASD and PAPVD.