To the Editor:
Percutaneous stent implantation has become the treatment of choice for coarctation of the aorta (CoA) and recoarctation in adults, given the good short to medium-term results and the decrease in the rate of complications as compared with surgical repair and balloon angioplasty. We present the cases of two patients, referred to our center for heart transplantation after being diagnosed as having idiopathic dilated cardiomyopathy (IDC), the possible etiological cause of which was found to be CoA. Both patients were successfully treated with percutaneous stent implantation, despite the presence of severe left ventricular dysfunction and pulmonary hypertension (PH).
The first case was that of a 46-year-old man with hypertension, IDC with severe left ventricular dysfunction and severe mitral insufficiency (Table), PH, normal coronary arteries and implanted defibrillator. He was in New York Heart Association functional class III upon admission to be evaluated for the indication for heart transplantation. He had normal sinus rhythm and complete left bundle branch block. Doppler ultrasound of the lower extremities led to the suspicion of CoA, which was confirmed by means of transesophageal echocardiography. Cardiac catheterization revealed the presence of CoA distal to left subclavian artery, relative hypoplasia of the aortic arch and descending thoracic aorta, a peak pressure gradient across the coarctation of 46 mm Hg (Table) and pulmonary artery pressure of 57/26 mm Hg (mean: 37 mm Hg).
The second case was that of a 44-year-old hypertensive woman with a diagnosis of postpartum IDC. She was admitted to the hospital in February 2003 to undergo assessment for heart transplantation, during which she had a vertebrobasilar transient ischemic attack. The results of Doppler ultrasound of the supraaortic arteries led to the suspicion of CoA. Transthoracic echocardiography revealed severe left ventricular dilation, severe systolic dysfunction and moderate-to-severe PH. Catheterization confirmed the presence of CoA distal to subclavian artery with a peak pressure gradient in the coarctation of 23 mm Hg (Table) and a pulmonary artery pressure of 47/23 mm Hg (mean: 34 mm Hg).
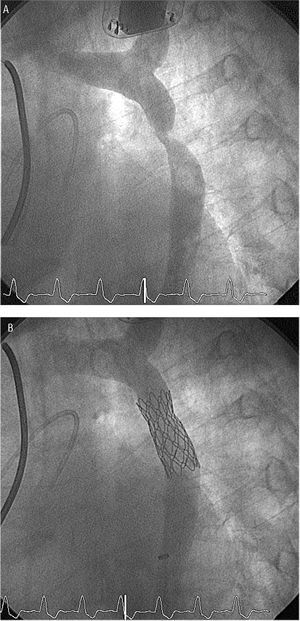
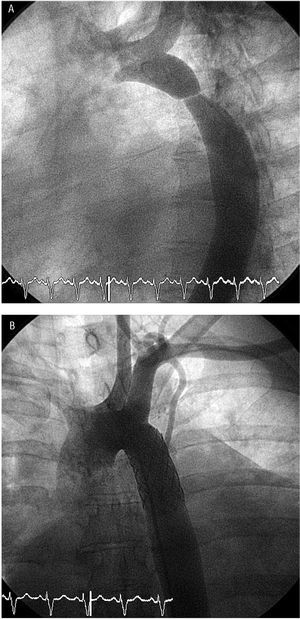
As the patients were considered to be at high risk for surgery, the decision was made to perform a percutaneous intervention in both cases. The procedures were carried out with sedation and analgesia. Bilateral femoral arterial access was employed in the first patient and right femoral and right radial arterial access in the second. A direct 16x40-mm stent mounted on a 16x40-mm BIB balloon (NuMED, Inc.) was implanted in the first case, whereas, the second patient underwent predilatation with a 16x40-mm balloon, and a 40-mm-long Palmaz-Schatz stent manually mounted on a 20x40-mm balloon was implanted. Both procedures were performed without complications, with excellent angiographic results (Figures 1 and 2) and a significant decrease in, or the disappearance of, the pressure gradient across the coarctation. The resulting clinical improvement made it possible to postpone transplantation for four years in the first case, whereas the second patient still has not had to be included in the waiting list.
Figure 1. Case 1: Severe aortic coarctation. Aortogram (A) before (left anterior oblique projection, 60o) and B) after implantation of a 16x40-mm Cheatham Platinum stent.
Figure 2. Case 2: Severe aortic coarctation. Aortogram (A) before (left anterior oblique projection, 60o) and B) after (frontal projection) implantation of a 40-mm-long Palmaz-Schatz stent mounted on a 20x40-mm balloon.
Aortic coarctation represents from 8% to 10% of all congenital heart disease. The patients remain asymptomatic or nearly asymptomatic for a long period of time, and it is often diagnosed in a young person undergoing a study for hypertension. Without treatment, most of the patients die before the fourth or fifth decade of life due to complications related to hypertension, such as coronary artery disease, stroke, rupture of the aorta or cerebral vessels, or heart failure.1 Moreover, despite surgical or percutaneous correction, there is a high risk of complications involving the aortic wall, which increases with age and in patients with a bicuspid aortic valve (25% to 50%).2 Heart failure has a bimodal distribution in the natural history of CoA, with an initial peak in children, generally related to associated congenital defects, and a second peak after the age of 40 years related to aortic stenosis, coronary artery disease or IDC.3
The surgical results are satisfactory and the indication for surgical treatment during the first year of life is little questioned. However, the risk associated with surgery in adults is significantly higher.4,5 Balloon angioplasty is considered to be the treatment of choice in native CoA after the first year of life, until adolescence, and also in postoperative recoarctation.6,7 Its limitations include a high rate of recoarctation, a risk of acute aortic dissection of 1% to 4% and a risk of aneurysm formation of 4% to 11.5%.8,9 Stent implantation prevents elastic recoil and reinforces weak portions of the wall, reducing the probability of recoarctation and the development of aneurysms or dissections. A review of the scientific literature demonstrates that the medium-term results with stent implantation are similar to those currently obtained with surgery and better than those obtained with balloon angioplasty. For this reason, this option, which is less aggressive for the patient, is becoming the treatment of choice for native or postoperative CoA in the adult.10-16 Its use in children is limited by the size of the release devices, the need for subsequent redilations in relation to somatic growth and the possibility of restenosis due to intrastent proliferation. Another case of successful stent implantation in an adult with CoA in the presence of severe left ventricular dysfunction and acute pulmonary edema has been reported in the scientific literature.17 However, despite the excellent immediate and short to medium-term results, the follow-up period for this technique is only 10 to 12 years, and future studies on the possible vascular complications and the long-term outcome in patients with stents implanted in aorta will be required.