Keywords
INTRODUCTION
The increase of the life expectancy of our patients, as well as the extended indications and the greater sophistication of the devices employed in the treatment of bradiarrythmias and tachyarrythmias have motivated a progressive growth in the number of pacemakers and defibrillators that are implanted every year. Simultaneously, we have observed an increase in the number of systems that need to be explanted due to different causes: the infection of the generator casing or the electrodes, the presence of bacterial endocarditis, the dysfunction of these electrodes, the need to implant more complex systems and the presence of secondary tricuspid insufficiency. The retrieval of the endovenous electrodes is not always a simple procedure. Sometimes the progressive development of fibrous adhesions that are formed in time around the electrodes along their route in the vascular territory, as well as in the atrioventricular endocardium, leads to the extraction through open surgery and with the help of extracorporeal circulation a necessity.1,2 Due to this difficulty, in scientific literature there has been a certain degree of controversy about the indications for extraction of the electrodes implanted chronically. At first, the only cases considered as a necessary cause for extraction were those cases in which the severity of the disease justified the risk of its retrieval. The appearance of percutaneous systems of extraction with high rates of success and that definitively diminished the risk of the procedure for the patient, has lead to a progressive increase in the number of indications. In this sense, a group of experts of the North American Society of Pacing and Electrophysiology published in the year 2000, the first clinical guidelines in relation to this disease, in which the indications (Table 1), contraindications and the types of related adverse events3 seen with these techniques are defined. In 1989 we began to extract pacemaker and defibrillator electrode leads in our department, through percutaneous techniques. The objective of this study is to review the results obtained after the extraction of 314 endocavitary pacemaker and defibrillator electrodes, using different systems from extraction throughout the study period, and to also analyze the observed complications.
METHODS
Our study consists of a retrospective analysis of all the cases of pacemaker and defibrillator extraction through the percutaneous route in a period between April 1989 and June 2006. The cases were collected from a cardiac surgery cardiac database in our hospital and completed after a review of the Operating Room registry book. Histories of all the patients in which a pacemaker or defibrillator extraction had been carried out, independent of the technique employed, and in addition to this data the demographic and surgical variables were registered, as well as the incidence of complications.
Extraction Techniques
From the introduction of the first systems of percutaneous extraction (at the beginning of the study in April of 1989), we began to carry out this procedure in an initial form, in all the patients who required the extraction of electrodes; the average sternotomy was only done, with or without extracorporeal circulation, in those cases in which the percutaneous technique failed. Two surgeons of our department made the extractions.
Although changes have happened all along this period, the following techniques have been used:
1. Simple traction. It was attempted, prior to other procedures, in those cases in which the implant had taken place less than a year before. A cautious dissection of the site where the electrode is placed is done up to the subclavian insertion. At this point the procedure, without radioscopic control, can be to smoothly traction the electrode after the prior introduction of a pacemaker guide, until the tip of the electrode is reached.
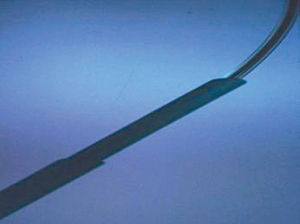
2. Contratraction sheath system (Cook Pacemaker Corporation®). From 1989 to 1997 we used this system, which consists of a guide that introduces itself along the electrode trying to reach the tip of it, fixing it by means of a counterclockwise turn. Next, 2 flexible sheaths are advanced, using the electrode as a guide. The external sheath, while being turned mechanically, liberates the electrode from the fibrous intravascular adhesions and allows the advance of the internal sheath up to 1-1,5 cm from the endocardium. Afterward, after fixing the external sheath to the endocardium, a traction mechanism of the electrode and the internal sheath is exerted (Figure 1).
Figure 1. Simple contratraction sheaths (Cook Pacemaker Corporation®) used for the smooth dissection of fibrotic zones produced by the passage of time in the vascular territory.
3. For free-floating electrodes in the vascular bed we used, during the early years, a biopsy clamp (straight Wilde clamp), which we introduced through the internal jugular vein to the right atrium under radiologic control, and with that we caught the electrode and proceeded to its traction (Figure 2).
Figure 2. Wilde clamp, employed in different surgical procedures as a biopsy clamp. The smooth tip does not damage vascular structures.
4. From 1998 onward, we began to use the radiofrequency sheaths (Cook Pacemaker Corporation®), whose mechanism is the same one than that of the simple sheaths, but connected to a bipolar radio frequency device that helps in the dissection of the endovascular adhesions. This system also has femoral lasso for electrodes that are left in the vascular system and are not accessible by superior access (Figure 3).
Figure 3. Contratraction sheath system with radiofrequency (Cook Pacemaker Corporation®).
Therapeutic Stance
1. The uncontaminated dysfunctioning electrodes were not extracted, but a new complete system was implanted in the same surgical event and on the same or contralateral side.
2. The patients with skin lesions due to prolonged bed rest were considered infected, and this was the reason why all of the system was extracted and a new one was implanted in the contralateral side.
3. In the case of infections of the generator casing or fistulas opened to the skin (even though they did not present bacteremia or endocarditis), if sepsis attributable to the device or endocarditis themselves was present, all of the system was extracted and a temporary pacemaker implanted if the patient needed it and a new, endocavitary system was later implanted.
Protocol Followed
In all the patients a standard preoperative protocol was followed. Blood cultures and wound cultures were obtained and a suitable antibiotic treatment was initiated before the surgery, as well as a transesophageal echocardiogram (TEE) in patients whose cause was related to an infectious process. A Doppler heart ultrasound of the venous vessels was carried out to plan the extraction and the new implant.
The electrodes were retrieved in the operating room under general anesthesia with arterial pressure, electrocardiogram and oximetry monitoring. We attempted to establish a surgical field that allowed us, at any time, to access not only by a subclavian route but also, in case of complications, by a femoral route or even to allow an average sternotomy. We have used an intrasurgical TEE in the past 2 years to control possible complications.
All of the patients, including those sent from other departments, in cases in which the indication of extraction was not of infectious origin, remained hospitalized until discharge. Patients that needed antibiotic treatment stayed in our hospital for 2 more weeks and were sent to their hospital of reference once the cultures were sterile to complete the antibiotic treatment, in those cases in which the patients asked to continue this treatment in their place of origin. All the patients were reviewed after a month since the hospital discharge, and the presence of complications was registered during this period.
Statistical Analysis
Data was analyzed by means of SPSS version 12.0 (Inc. SPSS Chicago, Illinois, USA) statistical software. The association between categorical variables was made with the test of c2 and Yachts correction or Fishers´ exact test. The comparison between parametric quantitative variables was done by means of a Student t test. The evaluation of prognostic factors was made with a logistic regression analysis and the results were expressed as odds ratio (OR) with the corresponding intervals of confidence of 95% (95% CI). For the tendencies analysis of linear proportions we used a linear tendency test (χLT). The statistical significance was established as P<.05.
RESULTS
Patients and Electrode Characteristics
From April 1989 to June 2006 we have extracted 314 endocavitary electrodes in 187 patients, whose mean age was of 69.60 years (range, 29.5-93.5 years; median, 71.5 years). The majority were male (68.4%; n=128). The average number of electrodes extracted per procedure was 1.57 (from 1 to 4 electrodes). A total of 196 ventricular catheters, 115 atrial and 3 from the coronary sinus were extracted, of which 11 were defibrillator electrodes and the rest, pacemaker electrodes. Altogether, 78 of these cables were left in the vascular space. The electrodes had been implanted an average of 69.16 months (mean period of time, 60.25; range, 0.11-234.6 months). In Figure 4 the percentage of electrodes implanted for less than a year can be seen, as opposed to which those that had been implanted between one and 4 years and those that were extracted after more than 4 years since implantation. During the study period a linear tendency was observed which turned out statistically significant (χLT; P=.011), with a progressive increase in the number of electrodes that we have extracted in every 3-year period, mainly due to the number of patients who we have received from other departments (Figure 5).
Figure 4. Time in months that electrodes had been implanted prior to their extraction.
Figure 5. Number of patients that were intervened for lead retrieval in our department during the study period. A significant linear tendency can be observed based on patients sent from other departments (χLT; P=.011).
Indications for Electrode Extraction
Altogether, 110 patients were sent from other departments (58.8% of our series). The clinical indications for the extraction of the electrodes are summarized in Table 2. Also, in Figure 6 we show the causes from extraction and can be observed to be different, according to whether the patients were from our department or had been sent of other centers. Fifty-one point four per cent of the electrodes were retrieved due to infection, bacteremia, endocarditis4 or embolisms (class I indication according to the North American Society of Pacing and Electrophysiology), and the 48.6% left corresponded to causes included in class II indications.
Figure 6. Causes for extraction according to the place of origin of the patients: the department of cardiovascular surgery of our hospital or other departments. Bars represent number of patients. TI indicates tricuspid insufficiency.
Extraction Techniques Employed
Altogether, 44 electrodes were extracted by means of simple traction. Contratraction, up until 1998, was used in 34 patients, and as of that date, contratraction with radio frequency was employed in 80 patients. In 8 patients it was necessary to use the Wilde clamp to reach the rest of left electrode. In 19 patients we used the femoral lasso to reach the electrodes that were free floating in the vascular system, 18 of them associated with radio frequency by means of a procedure that combined access by the subclavian and femoral veins. In 3 patients that presented bacterial endocarditis it was necessary to undertake a median sternotomy (in all of them because after the extraction there was a piece of the electrode left), in 2 using extracorporeal circulation additionally (Figure 7).
Figure 7. Methods for extraction employed. The simple contratraction techniques were employed up to 1998, when radiofrequency sheaths were introduced.
Results From the Electrode Extraction
Of the 314 electrodes, 304 were completely extracted (96.8%). The 10 remaining electrodes migrated to the pulmonary vein territory without clinical consequences. In 2 electrodes, the tip was in the superior vena cava and in the innominate vein, and in this last case it was necessary to undertake a median sternotomy 5 months later to extract the rest, since the patient was diagnosed with infectious endocarditis and presented a relapse after the suspension of the antibiotic treatment. The 7 others were lodged in the right ventricle, and in 2 patients, whose indication for the extraction was infectious endocarditis, it was necessary to make a second median sternotomy with extracorporeal circulation for its latter extraction. When we analyzed the cases of incomplete extractions we did not find variables that were associated to them in a significant form, although the average time since implantation of the 97.93 electrodes that could not be extracted completely was ±73.02 months, as opposed to the average time of implantation of the rest of the electrodes, 68.96±55.55 months, numbers that, however, did not reach statistical meaning. Either there was no correlation between the surgeons experience and the percentage of electrodes that were extracted completely, probably because during the study the percentage of cases was increased in a progressive way and, also, with increased complexity. In 3 of the 10 patients in whom the extraction was incomplete, its retrieval in other departments without optimal results had been previously attempted, this being the reason why they had been left in the vascular bed. All the electrodes that were incompletely retrieved were in the ventricle; of them, 8 were pacemaker and 2, defibrillator.
Complications
Table 3 shows the complications observed in our series. Altogether, 4 patients had mild complications that did not need an added intervention (2%), and 5 patients presented greater complications. A patient died of superior vena cava rupture during the procedure. There was another case of obstruction by a laceration in the right atrium that was solved by means of a median sternotomy in the same surgery. A patient presented abrupt hypotension with signs of sepsis after the retrieval of the electrodes, in spite of being treated with an effective antibiotic, and needed attention in the intensive care unit (ICU). A patient with a vegetation due to endocarditis by Staphylococcus aureus, measuring 6.7 cm presented a pulmonary embolism that required thromboendarterectomy. In this patient, a percutaneous extraction was considered due to the presence of adhesions secondary to a mitral valve substitution surgery done 3 months before. Lastly, we observed a case of serious tricuspid insufficiency secondary to the retrieval of the electrode that required surgery 3 months later. A univariate analysis was made in which we evaluated the age, gender, time since implantation of the electrodes, the presence of cable fragments left in the vascular territory, the experience of the surgical team during the study lapse, the number of electrodes that were extracted from each patient, the cause of the extraction of the cable and the location of the pacemaker (right side or left side). We observed a statistically significant relationship with the age of the patients, since the youngest were those in which complications were present (less than 60 years) (OR, 5.38; 95% CI, 1.07-27.23), and with endocarditis the likely cause for extraction (OR, 4.97; 95% CI, 1.04-23.70). We also verified that the risk of complications increased very significantly when the electrodes had been placed by via right subclavian vein (OR, 17.09; 95% CI, 2.15-135.70) (Table 4).
DISCUSSION
In light of our results, it is possible to emphasize the high rate of success with the combination of different retrieval methods (96.8%), with a percentage, although not elevated, of complications (>2.5%), which are not unimportant and that in our series have been related to endocarditis, the implantation of the device on the right side and to patients younger than 60 years of age. The increasing necessity of retrieving the pacemaker or defibrillator electrodes led us, at the end of the 1980s to carry these procedures in a less invasive manner, helped by the endovascular devices that began to be developed in those years.5-7 The first methods that were introduced replaced the technique of traction maintained after the introduction of some type of guide into the electrode by new systems that consisted of 2 sheaths, one internal and another external, made out of polyurethane, which were advanced through the vascular territory attempting to release the electrode of the surrounding fibrous structures and that, when arriving at the end of the electrode, carried out a contratraction mechanism, in an attempt to work against the movement of the myocardial wall to diminish in that way any complications.5 Although during the first years there was no a clear consensus with respect to the indications for electrode retrieval, the advances in the extraction techniques and the increase in the percentage of success gave rise to the appearance of the first published clinical guidelines in year 2003. In our series, 51.4% of the procedures included class I indications (50.3% of infectious origin) and the rest (48.6%) were class II indications. The infection of these devices, although not frequent, represents a potential source of serious complications. In the case of situations such as endocarditis related to the electrode, septicemias or infections of the same origin, there is no doubt that the extraction is the procedure of choice and that the complete retrieval of the system is the only method to eradicate this disease,5-7 since in the opposite cases the mortality figures can reach 25%.8 Similarly, in the cases in which there is a superficial infection of the pacemaker casing, or patients that present a skin lesion, though sometimes treated with antibiotics and local measures, extraction of all systems must still be the first option considered.9 In scientific literature, the incidence of infections related to endocavitary pacemakers or defibrillators published oscillate between 0.02 and 1.5%.1,10 The incidence of infection in our department during the study period was 0.84% in 2972 implantation procedures. It is important to emphasize the percentage of electrodes that we have retrieved due to an infectious cause. Although these cases reach 50.3%, this number increases considerably, to 75.3%, if we add the devices that are related with a lesion of the skin. The combination of different methods has allowed us to reach rates of success comparable to those of other authors. If we considered the percentage of electrodes that were officially completely retrieved, we had a 96.8% success rate, rising to 99.04% when we considered the percentage of clinical success, since only 3 electrodes later had to be retrieved through a median sternotomy. The percentage of electrodes that we were able to retrieve completely varies widely in the literature, with numbers that oscillate between 82.1% and 100% of electrodes, depending on the series read.11-14 It is, nevertheless, very difficult to standardize the results of different authors, since the average time of implantation of the electrodes also varies very widely, between 27 and 90 months.11-14 The incorporation of laser technology to percutaneous extraction techniques does not seem to offer greater advantages with respect to the rate of success obtained. Byrd et all4 published in May 2002 their experience in the United States in 2561 electrodes with this method and reached a percentage of success of 90%. In this manner, other authors obtain similar numbers that oscillate between 82.1% and 94%.10,12 The causes of incomplete extraction are related basically to the time of implantation5,14 (which increases fibrous reaction in the vascular bed), the surgeons experience making the extraction,5,14 implantation in the ventricle,14 the type of electrode (active fixation electrodes are more easily extracted)5 and the age of patients14 (they are more difficult to extract from younger patients). In our series, though we observed an important difference in the time since implantation of the electrodes that could not be extracted completely with respect to those that could (97.93 as opposed to 68.96 months), we did not find significant differences in this parameter. Also, we have not found significant differences during the period of study either, though the observed tendency points towards a reduction in function based on the experience of the surgical team. With respect to the type of electrode, some authors have shown a difference in the degree of difficulty for extraction of the electrodes according to their characteristics, such as the material they are manufactured with or the type of fixation (active fixation are easier to extract than the more complex defibrillator electrodes).5,14 Nevertheless, in our series, retrospectively, and considering that 58% of our patients were derived from other departments, it was impossible to register this data in a complete form. As for the defibrillator electrodes, only 11 were extracted and 2 of them could not be extracted completely. However, the relationship is not statistically significant due to the small sample size. Complications arising from electrode retrieval procedures are not unusual.12,15,16 Love et al3 defines a complication as a severe adverse event related to the procedure that needs some intervention to preserve the life of the patient or any complication related to the procedure that ends in the death of the patient or an irreversible damage of a function or structure. Also, they define mild complications as those related to the procedure that need some smaller intervention, that prolongs hospital stay or limits some function of the patient, but that in no case threatens the life or alters the function of an organ. The incidence of severe complications oscillates between 0.6% and 3.3% in the different series published,11,15,17,18 numbers similar to those observed by us. This incidence seems to be directly related with time since implantation, female gender, the number of electrodes per patient and the experience of the surgeon.14 In our series we have observed a significant relationship with the age of the patients, since the younger ones were those that presented complications, and with the presence of endocarditis. Also, we verified an important relationship to the placement of the device on the right side of the patient. Leacche et al18 published a case of superior vena cava in a patient with a pacemaker implanted on the right side during an electrode extraction with laser. Nonetheless, in other, larger series this incidence has not been evaluated. In our series, 2 of the 8 extracted pacemakers implanted on the right side (25%) displayed severe complications: one of the patients died due to rupture of the superior vena cava and another patient presented a cardiac obstruction that was solved in the operating room by means of an urgent sternotomy. One of the 8 patients had mild complications. It seems important to us to consider this data if we observed that the extraction on the right side can be more difficult, since the route to the right ventricle is more winding and the area where the subclavian vein and the superior vena cava meet as well as the right atrium can potentially be ruptured.
CONCLUSIONS
In conclusion, it seems clear there is an increase in the number of pacemaker and defibrillator electrode extractions. Percutaneous techniques are reducing the need for more aggressive surgeries, which in many cases are contraindicated due to the risk that they involve. However, it is important to consider that these techniques are not free of complications, making it advisable that an experienced surgical team carries them out, to diminish the number of complications and to increase the rate of success. Also, it seems essential to us that they be done in centers where it is possible to carry out an emergency surgical procedure in case a complication that can put in risk the life of the patient should arise.
ABBREVIATIONS
CI: confidence interval
OR: odds ratio
χLT: linear tendency test
Correspondence: Dra. T. Centella Hernández.
Servicio de Cirugía Cardiaca. Hospital Ramón y Cajal.
Ctra. de Colmenar, km 9,300. 28034 Madrid. España.
E-mail: centellato@telefonica.net
Received September 18, 2006.
Accepted for publication March 19, 2007.