To the Editor,
Percutaneous aortic valve replacement is now an alternative for the treatment of severe degenerative symptomatic aortic stenosis (SAS) in selected patients with high surgical risk or contraindication for surgery. According to various reports, there is great variability in the presence of coronary artery disease (CAD) in patients with SAS, which can range from 7%1 to 66%.2 In our centre, percutaneous coronary interventions (PCI) are performed following a protocol in patients with concomitant SAS and CAD who will undergo percutaneous aortic valve implantation, attempting a revascularisation as complete as possible one month before aortic valve replacement. In our historical series of 39 CoreValve® aortic valve implantations, prior coronary revascularisation was performed in 8 patients (20.5%). The CAD in these patients may evolve and present as effort angina or may lead to complications in the form of acute coronary syndrome, and require a new PCI once the valve has been implanted. There is only one case in the literature of PCI after implantation of this type of valve, as a consequence of the natural evolution of CAD,3 perhaps because the average follow-up for this type of patient is still very short.
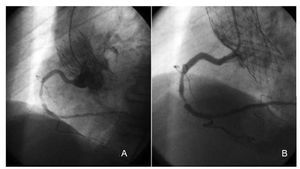
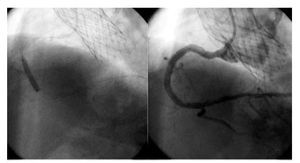
We report the case of an 85-year-old woman with SAS and a history of hypertension, dyslipidaemia and pulmonary arterial hypertension. Due to her high surgical risk (logistic EuroSCORE, 21.81%), we performed aortic valve replacement using CoreValve® prosthesis implantation. A coronary angiography was performed prior to the implant, which showed significant CAD in the anterior descending medial and proximal circumflex arteries, which were treated by PCI with conventional stents. The CT angiography also showed a lesion <0% in the middle segment of the right coronary artery, which was not operated. Four months after hospital discharge, the patient was admitted for acute coronary syndrome with no ST elevation and with high-risk criteria (troponin I at 1.43 ng/mL and electrocardiograms indicating acute ischaemia), which is why we decided to perform a coronary angiography. The procedure was performed via the left femoral route with a 6 Fr Avanti® introducer (Cordis). Prior to the coronary angiography, an aortography was performed that confirmed the correct positioning and functioning of the prosthesis and excluded the occlusion of the coronary ostia. For the study of the left coronary tree, we used a JL4 Super Torque Plus® diagnostic catheter (Cordis), which showed the permeability of the previously implanted stents with no evidence of progression in the coronary artery disease. For the right coronary artery, we used a JR4 Super Torque Plus® diagnostic catheter (Cordis) and a complex and subocclusive plaque was documented in the middle third (Figure 1A). We should note that for proper channelling of both coronary ostia it is necessary to lead the catheter tip through the rhomboid-shaped frames of the prosthesis. Furthermore, at the sinus of Valsalva level, the prosthesis takes the form of a calix so as not to compromise the flow of the coronary arteries. That way, the catheter is supported by the prosthesis and not by the aortic wall, which enables the coronary ostia to remain separated. It is essential to use a catheter with a large distance between the tip and the primary curvature to achieve a proper selective channelling of the coronary vessels. For this reason, we used a 6 Fr Vista Brite Tip® AR1 guiding catheter (Cordis) (Figure 1B) to perform the PCI, which enabled us to perform a proper channelling of the right coronary ostium. It also provided us with good support since it is more curved than the JR4 used for diagnosis and therefore adapts better to the curvature required by the prosthesis frames. We then advanced the 0.014" Pilot 50® angioplasty guidewire with hydrophilic coating (Abbott) and performed dilation with a 2.5 (15) mm Voyager balloon (Abbott). Finally, we implanted two conventional Driver Sprint Rx® stents (Medtronic) measuring 3.5´18 mm and 4´14 mm. The procedure finished without complications (Figure 2).
Figure 1. Coronary angiography A: JR4 Curve. B: AR1 curve.
Figure 2. Stent implantation and final result.
In the future, the need for performing PCI through a CoreValve® prosthesis will increase given the generalisation of this treatment in SAS and the longer follow-up time for these patients. We believe that this is a feasible and safe technique if proper precautions are taken.