To the Editor:
The percutaneous treatment of valve diseases in adults has long been limited to balloon valvuloplasty for rheumatic mitral stenosis and to the small number of aortic valvuloplasties performed as a bridge to surgery. The recent development of devices that can be implanted percutaneously for the treatment of aortic and pulmonary stenosis and mitral regurgitation have reawakened interest in this field of interventional cardiology.
Most of the effort is devoted to the treatment of degenerative aortic stenosis, as this is the most common valve disease in our general population. For this purpose, there are at least 8 percutaneous prostheses under development. The results of the initial experience with 2 of these prostheses (Edwards Sapien, Edwards Lifesciences, Inc.1,2 and the ReValving System, CoreValce3) in humans have been published in recent years, and ther publication of ongoing multicenter registries is expected to provide extensive information on their clinical utility.
Remarkably given the clearly established benefits of surgical valve replacement in patients with severe symptomatic aortic stenosis or with ventricular dysfunction have been clearly established, these studies are limiting inclusion to patients that have been rejected for surgery due to their estimated high surgical risk, based on the known poor prognosis in patients who have not been treated surgically upon reaching this point.
Echocardiographic studies confirm the good hemodynamic performance of the prostheses: in the series of Webb et al,2 the mean echocardiographic gradient decreased from 46 (±17) mm Hg to 11 (±5) mm Hg, and the aortic valve area (AVA) increased from 0.6 (±0.2) cm2 to 1.7 (±0.4) cm2. Moreover, over a mean follow-up period of 359 days, no relevant structural or functional abnormalities were observed in the prostheses. However, data concerning the anatomopathological features of the implanted prostheses have not been published. Thus, we present autopsy images of the first patient who died in our center following percutaneous implantation of an aortic prosthesis.
The patient was a 77-year-old man with severe degenerative aortic stenosis (AVA, 0.68 cm2; peak and mean transaortic gradients, 77 mm Hg and 49 mm Hg, respectively; ejection fraction, 66%; pulmonary artery systolic pressure within normal range). He had undergone thoracoplasty years earlier due to pulmonary tuberculosis and was diagnosed with severe chronic obstructive pulmonary disease (FEV1, 33%; FEV1/FVC, 0.64), requiring home oxygen therapy; these conditions produced dyspnea on minimal exertion. He had been formally rejected for surgery because of the high surgical risk and the decision was made to implant an Edwards Sapien biological aortic prosthesis via a transarterial route, according to the REVIVE protocol in which our center participated.
During the initial valvuloplasty, the patient developed respiratory distress and hemodynamic collapse, and the decision was made to intubate him and connect him to mechanical ventilation. A 26 mm prosthesis was implanted using a 24 Fr introducer, with good results obtained with a single inflation (area, 1.6 cm2; peak gradient, 20 mmHg; grade I/IV regurgitation on angiography and echocardiography). Despite the good function of the prosthesis during follow-up, the progress of the patient was slow, and he had repeated episodes of recrudescence of his bronchial disease with severe hypoxemia and/or hypercapnia, which required reconnection to the respirator (via a tracheostomy tube) after a few hours of spontaneous breathing. He died 3 months after implantation due to respiratory distress syndrome of noncardiac origin.
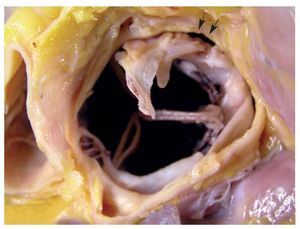
The autopsy showed that the prosthesis was well centered in the aortic annulus, with a slight anterior displacement and a small zone of agree with mala apposition to the annulus. The device covered the native valve almost completely, except for a small portion of the right leaflet, which was torn and part of which protruded into the aortic root above the metallic structure of the device (Figure 1). The latter did not interfere with the coronary ostia, which were on a higher level, and there were no impediments to the opening and closure of the prosthesis. The base of the stent was impacted in the basal segment of the interventricular septum, without affecting the functionality of the anterior mitral leaflet. Calcium deposits were observed in the mitro-aortic continuity (Figure 2). The injection of saline solution from the aortic portion demonstrated good coaptation of the prosthetic leaflets, without significant regurgitation.
Figure 1. Prosthesis (aortic aspect). The anterior aortic leaflet protrudes into the aortic root. Moreover, a small zone of malapposition of the stent is observed (arrow).
Figure 2. Prosthesis (ventricular aspect).
Thus, pathological techniques enable an accurate study of the relationship between the prosthesis and the adjacent structures, and help to confirm its satisfactory function.