To the Editor:
Percutaneous coronary intervention (PCI) in calcified lesions is a challenge for the interventional cardiologist and quite often devices for plaque modification, such as rotational atherectomy (RA) are needed to achieve appropriate expansion and apposition of stents.1 The optical coherence tomography (OCT) is a new high resolution intracoronary diagnostic technique that has proven its ability for characterization of atherosclerotic lesions2 as well as during PCI3,4 and in the evaluation of neointimal stent coverage.5 We describe OCT findings in a patient with a calcified lesion treated with RA and drug eluting stents.
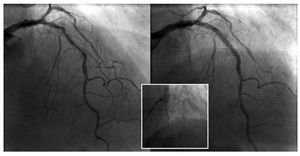
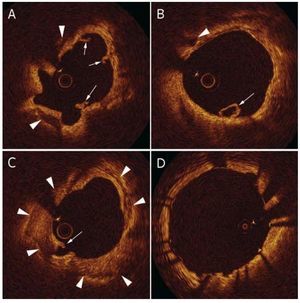
A 79 year-old male with history of hypertension and previous smoker, suffered an acute coronary syndrome with ST segment depression in leads V3-V6 and troponin I of 1.6. The echocardiogram showed preserved systolic function with apical hypokinesis. Coronary catheterization showed highly calcified long stenosis in the lef anterior descending artery (LAD) in the proximal and mid segments (Figure 1, left) and non significant lesions in the circumflex and right coronary arteries. PCI was performed, using RA (Rotablator, Boston Scientific) with a 1.75 mm burr. Then the OCT system was introduced (ImageWire, LightLab Imaging) to the mid LAD and images were obtained during pull back at 2 mm/s with simultaneous injection of contrast through the guiding catheter ("non-occlusive" technique6). The OCT (Figure 2) revealed large calcification (arrowheads), with areas of circumferential calcium (Figure 2C). The vessel lumen showed a uniform area with minimum diameter of 1.9 mm and multiple intimal microdissections (Figures 2A and B, arrows) produced by the Rotablator olive shaped burr. Two overlapping drug eluting stents (2.75x18 and 3x18 mm Xience V, Abbott Vascular) were implanted, with good angiographic result. The segment was studied again with OCT, showing good expansion and apposition of the stents (Figure 2D), with no plaque prolapse towards vessel lumen or edge dissections.
Figure 1. Angiographic image of the calcified lesion on the descending anterior (left) artery and of the result after the intervention (right).
Figure 2. Optical coherence tomography following rotational atherectomy. A and B: calcified lesion (arrowheads) and multiple intimal microdissections (arrows). C: circumferential calcification area. D: result after stent implantation.
High resolution (10-20 µm) of the OCT images allow for accurate characterization of atherosclerotic lesions, which are classified as fibrous (hyperintense), lipidic (hypointense, with undefined edges), and calcified (hypointense, with well-defined borders).1 In addition, in the context of PCI, it allows the identification of dissections, plaque prolapse through the stent struts, malapposition and neointimal tissue with an elevated sensibility,3,4 better than intracoronary ultrasound. The main limitation is the need to displace the blood from inside the vessel during the acquisition of images. An "occlusive" technique is usually used, with a proximal occlusion balloon and an injection of saline through its lumen,7 which results technically complex and causes transitory ischaemia. The alternative "non-occlusive" technique used in this case simplifies the procedure considerably.6
In the case in question, the OCT allowed evaluation of the effect of the rotational atherectomy in the calcified plaque: a uniform arterial lumen and multiple microdissections on the arterial wall. In addition, it was helpful to check the appropriate expansion and apposition of the stents, which can be problematic in heavily calcified lesions8 and are prioritary for the prevention of stent thrombosis.