To the Editor:
Essential thrombocytosis (ET) is a myeloproliferative clonal disease, of uncertain aetiology, which generates pathological expansion of megakaryocytes in the bone marrow, with the consequential persistent increase in platelet count. It is associated with an elevated risk of haemorrhaging, vasomotor symptoms and thrombosis, especially thrombus in the brain, peripheral and heart arteries; the incidence of acute coronary events is of 9.4%.1
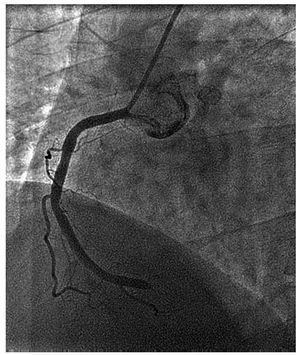
We present a case of a 52-year-old male with no known cardiovascular risk factors (CVRF) or family background of ischaemic heart disease. The sole background fact of interest is that he presented a diagnosis of ET in a haematology department study, without treatment at the time due to the low initial risk of complications. On the evening of his admission, he suffered a sudden loss of consciousness. He was attended at home by the emergency services; an electrocardiogram was carried out, showing ventricular fibrillation requiring electrical defibrillation on two occasions. Once rhythm was re-established, the electrocardiogram showed an atrial fibrillation with lateral ST segment elevation. He was admitted to the coronary service, and fibrinolysis was performed, which initially was effective, but 2 hours later experienced recurrent pain and re-elevation of the lateral ST segment, so a rescue angioplasty was carried out. The cardiac catheterization shows complete distal occlusion, with thrombotic material, in the right coronary artery; it is revascularised with a conventional stent (Coroflex®) of 3.5×13 mm (Figure). All other coronary arteries showed no significant signs of angiographic lesions.
Figure 1. Coronary catheterization with complete occlusion of the right coronary artery.
On admission, the patient presented a haemoglobin count of 11.6 g/dL and 569 000 platelets. A hypercoagulability study was performed, which shows an S protein (SP) deficiency and mutation of the JAK2 V617F tyrosine kinase (substitution of valine with phenylalanine in position 617).
Although the ET is a cause of thrombosis, association with myocardial infarction is infrequent and in this case, the patient presented no other CVRF, which would imply greater underlying risk of heart disease. The role of haemopathy stands out as a main cause of acute coronary episodes. For its diagnosis, a platelet count of >400 000/mL , bone marrow aspiration and biopsy that shows megakaryocytic hyperplasia is required; as well as excluding causes such as reactive thrombocytosis and other types of myeloproliferative disorders.2
As for treatment, thrombolitic treatment is a correct option since patients affected by this disease usually present acute thrombotic arterial occlusions, with absence of significative stenosis in the underlying coronary tree. It is important to keep the haemorrhagic risk of the underlying disease in mind when deciding the definitive therapeutic strategy; the use of drug eluting stents entails the need for double antiplatelet treatment over a longer period, with the ensuing risk of haemorrhaging. In the long-term, in those patients with high thrombotic risk (large platelet count, prior history of ischemic episode, age over 60), treatment with hydroxyurea, which has been related with reduction of thrombotic risk in a prospective controlled study, is recommended.1,2
The relationship of the disease with the JAK2 V617F mutation is prominent. This mutation is present in 50%-60% of ET cases, related with hypersensibility of the haematopoietic stem cell to thrombopoietin. In addition, the ET produces microvascular circulatory disorders and dysfunction of normal platelet activity. Said mutation could be directly related to the increased risk of thrombosis, although more studies are needed to confirm this.3
The association of the ET with an SP deficiency is infrequent so it has scarcely been documented. The SP concentration could be reduced in patients with acute thrombotic episodes, although series of patients with ET and reduction in the concentration of the natural anticoagulants such as the SP have been documented.4
To conclude, in young patients with no known CVRF who present an acute coronary syndrome, as well as the hypercoagulability study, the ET must be taken into account as a possible aetiology of the process.