INTRODUCTION
Non-bacterial thrombotic endocarditis (NBTE) is characterized by endocardial vegetations made up of accumulations of sterile blood platelets and fibrin which do not usually involve inflammatory responses.1 Incidence ranges between 0.3% and 9.3% in autopsy series and usually affects patients aged between 40 and 80 years, although people of any age can be affected.2
Nonbacterial thrombotic endocarditis is usually associated with neoplasms and other chronic debilitating diseases, but may also be associated with acute processes such as sepsis, infections (such as pneumonia or pyelonephritis) or large burns.2,3 Although neoplasms are the underlying disease entities most frequently encountered in serial autopsies3-6 (specifically, mucinous adenocarcinoma), surgical series7 have shown that NBTE is more frequent in patients with connective tissue and autoimmune diseases and rheumatic heart disease.
Nonbacterial thrombotic endocarditis is characterized by the high incidence of accompanying embolic events, approximately 42% (range, 14.1%-90.9%), the most frequent ones being cerebral.2
Diagnosis is not easy, since the index of suspicion is low and imaging tests are not reliable. Controlling the underlying disease is the most important factor in the treatment of NBTE. Nevertheless, anticoagulant therapy with heparin appears to prevent embolic events,8 and is a treatment that should be established based on similar pathogenesis and the association of this entity with Trousseau's syndrome and disseminated intravascular coagulation.9
Several autopsy series have been published in Spain, including those by Pujol et al,4 Maté del Tío et al5 and Villar et al.6 The aim of the current study is to expand the information available on this pathological process with special focus on underlying diseases.
The aims of this study were: to identify the main diseases underlying NBTE and, if these varied from the published series, to study previous valve lesions and the type of underlying valvular heart disease, analyze the performance of the diagnostic methods used, and group together the clinical characteristics these patients present, thereby establishing the clinical patterns that should lead us to suspect the presence of this disease.
METHODS
The study was conducted in the Hospital Universitario 12 de Octubre in Madrid. It was a cross-sectional study reviewing all the autopsies performed over 29 years (1974-1977 and 1980-2004) in the anatomical pathology department. The years 1978-1979 were not included due to technical problems encountered when recovering all the clinical-pathological information. All the autopsy studies included systematic study of the heart (opening all four chambers via longitudinal section of the atrial and ventricular walls, gross and microscopic examination of the valves, and dissection of the coronary arteries) and, thus, it is unlikely that any case of NBTE was missed. Information on the patients who fulfilled the selection criteria was obtained by inspecting clinical histories and histological preparations (when possible) by a clinical physician and an anatomical pathologist, respectively.
All patients who had an anatomicopathological diagnosis of nonbacterial thrombotic endocarditis, noninfective thrombotic endocarditis, verrucous endocarditis, marasmic endocarditis, or marantic endocarditis were included.
Patients were excluded when histological findings demonstrated the presence of an acute or chronic inflammatory infiltrate or culture-positive endocardial tissue. The presence of sepsis or infection in another location was not an exclusion criterion, unless valve colonization was demonstrated.
Nonbacterial thrombotic endocarditis was diagnosed on the basis of one or more vegetations on one or more cardiac valves without destruction, abscess or perforation. It was defined histologically by the presence of a fibrin thrombus and blood platelets without polymorphonuclear leukocytes or microorganisms.
Statistical Analysis
Data were collected and analyzed using the SPSS statistical package 12.0; descriptive statistics were determined. Given the size of the sample, the Kolmogorov-Smirnov test was used to test the model for normality and whether parametric tests could be used; the test was negative and thus nonparametric tests were finally used. To test whether there was an association between the variables, the χ2 test was used (with the Fisher exact test when necessary) for qualitative variables and the Mann-Whitney U test for quantitative ones.
RESULTS
In the periods 1974-1977 and 1980-2004, 2041 autopsies of adults were performed in the Hospital Universitario 12 de Octubre de Madrid in the anatomical pathology department. This yielded 22 cases of NBTE which translates into an incidence of 1.08%.
Distribution by Age and Sex
Of the 22 cases, 11 (50%) were men and 11 were women (Table 1 and Figure 1). The mean (standard deviation [SD]) for age was 63.0 (15.1) years (range, 24-84 years).
Figure 1. Distribution by age and sex..
Associated Diseases
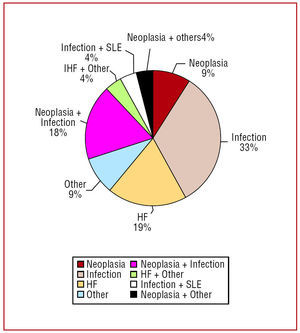
Table 1 and Figure 2 underline neoplasm, infection and heart failure as associated diseases.
Figure 2. Associated diseases. HF indicates heart failure; SLE, systemic lupus erythematosus.
Neoplasm As the Main Associated Disease
Of the 7 patients where NBTE was associated with a neoplasm, 1 patient presented 2 concurrent neoplasms: renal carcinoma and prostatic adenocarcinoma. Of the 8 existing neoplasms, 5 (62.5%) were adenocarcinomas 2 pancreatic, 1 esophageal, 1 gastric, and 1 prostatic whereas 3 (27.3%) were carcinomas (2 renal and 1 bronchogenic). Of the 7 patients with neoplasms, 6 had progressed to metastasis (85.7%).
The average age of these patients was 60.4 years and 85.7% were men. A statistically significant association was demonstrated between the type of underlying disease (neoplasm) and sex (male) via the Fisher exact test (P=.022).
Infections As the Main Associated Disease
In 12 cases NBTE was associated with infectious disease. These included 6 cases of sepsis (50%; 27.3% of total cases), 3 cases of tuberculosis (25%; 13.6% of the total), 2 cases of pneumonia (16.6%; 9.1% of the total) and 1 case of chronic pyelonephritis (8.3%; 4.5% of the total). One patient with tuberculosis also had systemic lupus erythematosus. Some 66.6% of the patients with infection were women with an average age of 69.5 years.
Heart Failure As the Main Associated Disease
In 5 (22.7%) patients, NBTE was associated with heart failure, one of whom also had chronic kidney failure (CKF). There were also previous valve lesions in 3 patients. Their average age was 64 years and 60% were men.
Other Disorders As the Main Associated Disease
The only clinical association established in 1 patient was alcoholism, whereas 1 patient with previous valvular heart disease also had acute hemorrhagic pancreatitis. There was one case of toxic oil syndrome in a patient who also presented a neoplasm.
Valvular Heart Disease As a Predisposing Factor
There was previous valvular heart disease in 45.4% of the patients. Of the 10 cases associated with valvular heart disease, 6 were rheumatic (60%; 27.3% of the total cases), 3 were degenerative (associated with age or hypertension) (30%; 13.6% of the total), and 1 involved congenital bicuspid aortic valve (10%; 4.5% of the total). Of the 10 cases of valvular heart disease, 6 (60%) occurred in women with an average age of 62.2 years. The types of valvular disease are shown in Figure 3.
Figure 3. Types of valvular heart disease.
Cause of Death
In most cases, death (Table 1) occurred as a consequence of the main associated disease. The cause of death was directly related to NBTE in 2 (9.1%) patients (cerebral herniation after embolism in the central nervous system and pulmonary thromboembolism).
Valvular Disease
In 8 (36.5%) patients, only the mitral valve was affected, whereas in 5 (22.7%) the aortic valve was affected and the tricuspid valve in 1 (4.5%). Six patients had both mitral and aortic valve disease (27.3%), whereas in 1 patient (4.5%) both the aortic and tricuspid valves were diseased. In 1 patient (4.5%), the autopsy report did not specify which valve was affected. There were no cases of three-valve or four-valve endocarditis. There was no statistically significant association between the diseased valve and sex, age, associated disease, or the presence of murmurs at auscultation.
Clinical Findings
There was no ante mortem clinical suspicion of NBTE in any patient. Heart murmur was detected in 6 (27.3%) patients at auscultation. Admission was due to an episode of acute heart failure in 22.7% of the patients.
Electrocardiographic data for each patient were collected, if available, demonstrating that 12 (54.5%) patients were in sinus rhythm. Atrial fibrillation was the most frequent pathological ECG alteration (6 cases, 27.3%), followed by conduction alterations.
Histopathological Findings
Fourteen of the 22 cases included in the study underwent histological examination (Table 2). Ten had 1 valve lesion, 2 had 2 lesions, 1 had 3 lesions, and 1 had 4 lesions. The examined vegetations were between 0.2 and 2.5 cm (mean, 0.4 cm) and all were macroscopically visible. Six of the patients had lesions located on the free margin of the valve, 2 on the ventricular surface and 6 on the atrial surface.
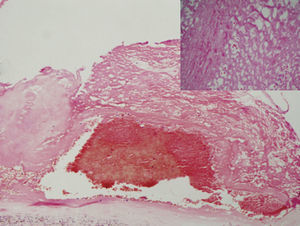
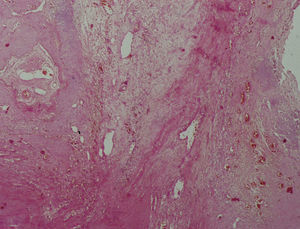
All the lesions were predominantly made up of fibrin and blood platelets, and substantial amounts of red blood cells were found in 3 patients (Figure 4). Granulation tissue was found with neovascularization and active enlarged fibroblasts in 3 patients (Figure 5). In 2 of these 3 cases, a total of 11 fibrotic foci were observed. There were calcium deposits in 5 of these cases of sclerosis. The use of specialized techniques did not identify polymorphonuclear leukocytes or microorganisms.
Figure. 4. The image shows (HE, 340) a vegetation made up of a web-like mesh of fibrin and blood platelets (see detail; HE, 3200), with numerous red blood cells trapped within it (patient 7).
Figure 5. The image shows (HE,3100) granulation tissue with neovascularization within loose myxoid tissue (patient 19).
Peripheral Embolisms
Peripheral embolisms were found in 9 patients (40.9% of total cases) during autopsy (Table 3). The organs more often involved were the spleen in 5 patients (22.7%) and the kidney and central nervous system, each in 4 (18.2%) patients. In 1 patient, the small intestine and legs (4.5%) were affected, in addition to the kidney and spleen, and in another patient the lung was affected, in addition to the kidney and central nervous system. In 4 patients, the embolisms involved 2 or more organs. There were no cases of coronary embolism.
The average age of patients with embolic events was 66 years (range, 31-84 years) and 55.5% were men. The main associated disease was neoplasm, in 11.1% of patients; infection, 33.3%; heart failure, 22.2%; neoplasm-associated infection, also 22.2%; and a neoplasm- associated with toxic oil syndrome, 11.1%.
There was no statistically significant association between the presence of peripheral embolisms and age, sex, associated disease, or the affected valve. Nor was there any association between the fact of having a peripheral embolism and receiving an echocardiogram or anticoagulant therapy.
Echocardiogram
Transthoracic echocardiography was performed in only 4 (18.2%) patients. The echocardiogram was not diagnostic in 2 patients, whereas in the other 2 patients the finding of endocarditis was doubtful. Transesophageal echocardiography was not performed in any patient.
Anticoagulant Therapy
Of the total of 22 patients, 7 (31.8%) received anticoagulation therapy, 4 (18.2%) with sodium heparin and 3 (13.6%) with acenocoumarol. The main indication for anticoagulant therapy was atrial fibrillation.
DISCUSSION
As in other studies,3,4,7 we have used a broad definition of NBTE that includes every noninfected thrombotic valvular vegetation, regardless of size, previous state of the valve or the presence of an autoimmune connective tissue disorder.
In our study, frequency, average age and distribution by sex was similar to that described in other works.2-6,10
In our study, NBTE was associated with underlying neoplasms and infections, as well as heart failure, as found in classic series.3 The high incidence of infection was noteworthy as being the main underlying disease, rather than neoplasm.
Furthermore, valvular heart disease was identified as a predisposing factor in a high percentage of the patients (45%), indicating that previous valve lesions are a significant factor in the pathogenesis of NBTE,1,2 as already reported by Gross and Friedberg in 1936. Given the prevalence of rheumatic heart disease in Spain, it is reasonable to assume that most valve lesions are of rheumatic origin, although it is probable that the frequency of degenerative valvular heart disease will increase in the future. Valvular heart disease was considered a predisposing factor only in those cases where the valve affected by NBTE and the valve affected by valvular heart disease were the same.
Adenocarcinoma was the most frequently associated neoplasm, both in our series and as reported in the literature.2-5,10 The location and type of tumor reported in other series depended on the incidence of each tumor in the given geographical area. However, the lack of association with hematological malignancies was noteworthy, as described in previous series.2,4,5,8,10
On the other hand, we would like to highlight the high percentage of cases associated with tuberculosis (13.6% of the total), which was similar to that found by Pujol et al4 in Spain, although this has rarely been described in the international literature.
In one case, the patient presented systemic lupus erythematosus, but also had tuberculosis. The histological findings were not characteristic of Libman-Sacks endocarditis, thus the infection should probably be regarded as the main underlying disease. Furthermore, 1 patient presented toxic oil syndrome, but also had a neoplasm, making it difficult to estimate the real significance of the syndrome in the etiology of this case of NBTE, since this association has not been previously described, whereas neoplasms have been considered the main underlying disease in many series.
The mitral valve was more frequently affected than the aortic valve, which is in line with the literature.2-5,10 This seems to be due to these valves experiencing increased blood flow turbulence, which may promote endothelial damage and, together with hypercoagulability, can lead to the formation of thrombotic vegetations. This hypothesis has been verified in animal studies, where the creation of arteriovenous shunts led to verrucous endocarditis.11
In the present study, the incidence of peripheral embolism was similar to previous studies.2,10 Nonbacterial thrombotic endocarditis was involved in the pathogenesis of embolism, as well as heart failure and atrial fibrillation which appear in a high percentage of cases. However, the absence of coronary embolism and the presence of a single case of pulmonary embolism is noteworthy compared to other studies.
There was no clinical suspicion of this entity in any patient. The diagnosis may have been hindered by the characteristics of the underlying disease, the low amount of cardiac murmurs (27.3% in our series) and the rapid clinical course. Furthermore, the reliability of transthoracic echocardiography tends to be low, given the small size of the vegetations. In our series, this was performed in 4 patients and was not diagnostic in any of them. One study12 reported on 6 patients diagnosed with NBTE post mortem, who had all undergone echocardiography within 45 days of death. Two-dimensional echocardiography demonstrated vegetations in 4 of 6 patients and in 5 of 11 affected valves. However, this technique may not be able to detect vegetations less than 4 mm, thus, if clinical suspicion is high, transesophageal echocardiography should be considered.13
We should raise our level of awareness of this condition so that we can make a diagnosis while the patient is still alive and thus initiate anticoagulant treatment. Although no prospective studies have confirmed this, it may prevent embolic events, thereby improving patient prognosis.
CONCLUSIONS
Nonbacterial thrombotic endocarditis is particularly associated with infections and neoplasms, although it is also associated with other debilitating diseases. In our series, the most frequent neoplasms were pancreatic adenocarcinoma and renal carcinoma, whereas sepsis and tuberculosis were the most frequent infections. Diagnosing the latter gains in importance, since they are potentially curable diseases.
Nonbacterial thrombotic endocarditis should be suspected in every patient presenting signs or symptoms of peripheral embolism with an associated debilitating disease and transthoracic echocardiography should be performed to attempt to confirm the diagnosis. If clinical suspicion is high or the transthoracic window inadequate, transesophageal echocardiography should be strongly considered. In conclusion, the presence of NBTE should be actively investigated, and if confirmed, anticoagulant treatment should be initiated to attempt to improve patient prognosis.
ABBREVIATIONS
NBTE: non-bacterial thrombotic endocarditis
Correspondence: Dra. J. Llenas García.
Servicio de Medicina Interna. Hospital 12 de Octubre.
Avda. de Córdoba, s/n. Planta 15 derecha. 28040 Madrid. España.
E-mail: jarallenas@hotmail.com
Received July 4, 2006.
Accepted for publication January 31, 2007