To the Editor,
A 42-year-old male patient was admitted to the hospital with fever and chest pain complaints.
The patient had a history of human immunodeficiency virus (HIV) infection, which was diagnosed 15 years before the hospital admission. The CD4+ T cell count at admission was 874 cells/μL and viral load was undetectable (<50 copies/ mL). Nadir of CD4+ T cells was 414 cells/μL in 1996 and patient was in treatment with tenofovir + didanosine + atazanavir + ritonavir since 2003 with an undetectable level of viral load the last 6 years. He had no relevant prior cardiac history.
He began having fever, diarrhea, poor general condition and myalgia over the course of one week. In the last two days prior to admission he developed progressive intense stabbing chest pain at rest, with radiation to the back that worsened with recumbent position and deep breaths. Chest pain intensity diminished following intravenous analgesics but not sublingual nitroglycerin.
On physical examination the vital signs were normal, other than a body temperature of 38ºC. He did not have signs of systemic or pulmonary congestion, neither low output signs nor respiratory distress. The heart sounds were normal.
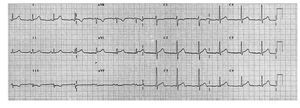
Laboratory data revealed leukocytosis with lymphocytosis, C-reactive protein was 19 mg/mL and peak cTnI reached 30 ng/mL. Chest radiography was unremarkable. ECG showed normal sinus rhythm with 1 mm ST-segment elevation in leads DI, aVL, and V4-V6 (Figure. 1). Nasal swab, blood, feces and urine were taken for culture and real-time reverse transcription polymerase chain reaction (RT-PCR) assays.
Figure 1. ECG at admission showing sinus rhythm with ST-segment elevation in leads V2 to V6, aVL and DI with ST-segment depression in inferior leads.
Despite the initial clinical suspicion of myocarditis a coronary angiography was performed that ruled out coronary artery disease.
The 2D echocardiography obtained in the emergency department showed a normal sized non-hypertrophic left ventricle with inferior wall hypokinesis and normal global systolic function, with no pericardial effusion.
The patient was admitted with a diagnosis of acute myocarditis. The RT-PCR was positive for Pandemic Influenza A (H1N1) infection.
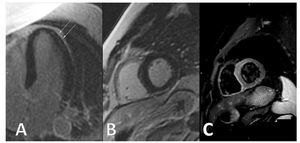
A conventional delayed-enhanced Cardiac Magnetic Resonance study conducted 3 days after admission shows typical intramyocardial latero-apical and epicardial inferior late enhancement, as well as high signal intensity at T2-weighted imaging, consistent with acute multifocal myocarditis (Figure 2).
Figure 2. Cardiac Magnetic Resonance. Panel A demonstrates intramyocardial late enhancement in the long axis view. Panel B shows a short axis view with epicardial late enhacement. Panel C depicts high T2 signal in the corresponding slide that is compatible with myocardial edema.
The patient was treated with oseltamivir with good clinical response. He did not develop any complications during the hospitalization. When treatment was completed, a second RT-PCR assay for H1N1 was negative. He was discharged with the diagnosis of acute viral myocarditis secondary to H1N1 infection.
As of April 14, 2010, more than 208 countries and overseas territories or communities have reported laboratory-confirmed cases of pandemic influenza H1N1 2009, including at least 17 700 deaths.1 Most deaths are related to respiratory complications in patients with underlying conditions conferring a high risk. Importantly, the clinical presentation, as well as the cardiac magnetic resonance findings, in our case were similar to those reported in other common etiologies of myocarditis, such as Parvovirus B19 infection.
HIV infection is a known etiology for myocarditis;2 however, the introduction of highly active antiretroviral therapy has reduced its incidence,3 and the temporal presentation of the disease together with the normalization of the RT-PCR makes H1N1 infection the most likely cause.
A series of cases of H1N1 myocarditis in a pediatric population has recently been published.4,5 Our case differs from those previously published because it is not a child and expands the population susceptible to this complication. Therefore, H1N1 influenza should now be considered in the differential diagnosis of viral myocarditis, since prompt initiation of oseltamivir may alter the clinical course of the disease. Whether current antiviral therapies may also limit cardiac involvement is largely unknown and deserves further investigation.