The Geriatric Cardiology Section was created as part of the Spanish Society of Cardiology (SEC) in 1995 and focuses on understanding the diagnostic and therapeutic characteristics of elderly patients with heart disease. Although the section is small, its efforts have been admirable, particularly in the areas of scientific expertise and knowledge dissemination. In this editorial, we would like to highlight the section's main scientific contributions to the field of heart disease in elderly patients seen in daily clinical practice, a topic that usually receives minimal attention (table 1).
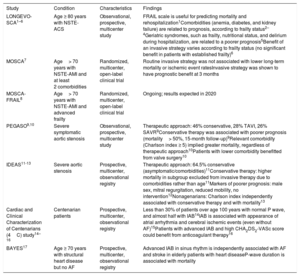
Most relevant characteristics and findings from some studies undertaken by the Section on Geriatric Cardiology of the Spanish Society of Cardiology
| Study | Condition | Characteristics | Findings |
|---|---|---|---|
| LONGEVO-SCA1–6 | Age ≥ 80 years with NSTE-ACS | Observational, prospective, multicenter study | FRAIL scale is useful for predicting mortality and rehospitalization1Comorbidities (anemia, diabetes, and kidney failure) are related to prognosis, according to frailty status2–4Geriatric syndromes, such as frailty, nutritional status, and delirium during hospitalization, are related to a poorer prognosis5Benefit of an invasive strategy varies according to frailty status (no significant benefit in patients with established frailty)6 |
| MOSCA7 | Age> 70 years with NSTE-AMI and at least 2 comorbidities | Randomized, multicenter, open-label clinical trial | Routine invasive strategy was not associated with lower long-term mortality or ischemic event ratesInvasive strategy was shown to have prognostic benefit at 3 months |
| MOSCA-FRAIL8 | Age> 70 years with NSTE-AMI and advanced frailty | Randomized, multicenter, open-label clinical trial | Ongoing; results expected in 2020 |
| PEGASO9,10 | Severe symptomatic aortic stenosis | Observational, prospective, multicenter study | Therapeutic approach: 46% conservative, 28% TAVI, 26% SAVR9Conservative therapy was associated with poorer prognosis (mortality> 50%, 15-month follow-up)9Relevant comorbidity (Charlson index ≥ 5) implied greater mortality, regardless of therapeutic approach10Patients with lower comorbidity benefitted from valve surgery10 |
| IDEAS11-13 | Severe aortic stenosis | Prospective, multicenter, observational registry | Therapeutic approach: 64.5% conservative (asymptomatic/comorbidities)11Conservative therapy: higher mortality in subgroup excluded from invasive therapy due to comorbidities rather than age11Markers of poorer prognosis: male sex, mitral regurgitation, reduced mobility, no intervention12Nonagenarians: Charlson index independently associated with conservative therapy and with mortality13 |
| Cardiac and Clinical Characterization of Centenarians (4C) study14–16 | Centenarian patients | Prospective, multicenter, observational registry | Less than 30% of patients over age 100 years with normal P wave, and almost half with IAB14IAB is associated with appearance of atrial arrhythmia and cerebral ischemic events (even without AF)15Patients with advanced IAB and high CHA2DS2-VASc score could benefit from anticoagulant therapy16 |
| BAYES17 | Age ≥ 70 years with structural heart disease but no AF | Prospective, multicenter, observational registry | Advanced IAB in sinus rhythm is independently associated with AF and stroke in elderly patients with heart diseaseP-wave duration is associated with mortality |
AF, atrial fibrillation; IAB, interatrial block; NSTE-ACS, non–ST-segment elevation acute coronary syndrome; NSTE-AMI, non–ST-segment elevation acute myocardial infarction; SAVR, surgical aortic valve replacement; TAVI, transcatheter aortic valve implantation.
Population aging is a concern, both at present and in the future. By 2050, octogenarians will account for over 30% of the world population, and Spain is expected to have the oldest population in the world.18 Ischemic heart disease (IHD) is closely linked to age, and non–ST-segment elevation acute coronary syndrome (NSTE-ACS) is one of the most common reasons for hospitalization among elderly people. Despite this, the elderly population is underrepresented in clinical trials and, therefore, little information is available on the best approach for these patients. Clinical practice guidelines do not offer clear guidance, and decision-making is a challenge for cardiologists managing these patients. To further complicate the matter, age cannot be deemed a sufficient or single criterion for denying treatments and interventions. However, apart from age, what other criteria should be considered? Although this issue may seem simple for geriatricians, it is less straightforward for cardiologists.
The LONGEVO-SCA registry1 (Impact of Frailty and Other Geriatric Syndromes on Clinical Management and Outcomes in Elderly Patients With Non–ST-segment Elevation Acute Coronary Syndrome) aimed to analyze the impact of a comprehensive geriatric assessment (CGA) during hospitalization to provide tools and knowledge that will help to optimize therapeutic decisions in these patients. This registry enrolled 532 patients aged ≥ 80 years at 44 hospitals in Spain and confirmed the prognostic impact of frailty on NSTE-ACS beyond the classic prognostic factors listed in manuals and guidelines. It is particularly enlightening that frailty was assessed using the FRAIL scale, an instrument that is quick, simple to use, and readily applicable in a setting in which limited patient mobility and staff time constraints often hinder CGA use in cardiology departments. Additional analyses have provided useful data on the relationship between comorbidities and frailty, both highly prevalent in elderly patients with heart disease. For instance, anemia, diabetes, and kidney function appear to have a differential prognostic impact, according to the presence or absence of frailty.2–4 Other substudies of the registry addressed additional relevant aspects, such as malnutrition and the appearance of delirium during hospitalization, that identify patients with a poorer geriatric and prognostic profile but are not usually included in routine assessments, despite being potentially preventable and treatable situations.5
What strategy should be used with elderly patients who have NSTE-ACS? There are conflicting data on the benefit of a routine invasive strategy for these patients, and there is even less evidence on whether frailty, comorbidity, and other components of the CGA could help identify subgroups in whom the strategy is clearly favorable in terms of risk-benefit. Although a LONGEVO-ACS substudy6 observed a lower short-term incidence of cardiovascular events in the invasive strategy subgroup, this benefit was apparently not observed in the frailest patients.
The MOSCA trial7 was conducted to shed light on this issue and included patients with significant comorbidity, finding that the routine invasive strategy was not associated with lower long-term mortality or the appearance of ischemic events. Additionally, the MOSCA-FRAIL trial,8 currently in the enrollment phase, was designed to address this uncertainty, but this time in elderly patients with NSTE-AMI and severe frailty. A major hurdle for this type of clinical trial in very elderly patients with heart disease, comorbidities, and geriatric syndromes is that enrollment itself is sometimes a dilemma for the treating cardiologist, and in other cases, the patient or family are themselves reluctant to participate. This illustrates that decisions in this field are often based on subjective impressions, and precisely for that reason it is essential to encourage and promote specific research in this area to obtain more solid evidence.
When treating elderly patients with geriatric syndromes, another major issue is bleeding risk, an unavoidable concern when prescribing antithrombotic and anticoagulant agents or indicating an invasive strategy. This is further complicated by the fact that bleeding risk scales are not adequately validated among elderly persons. For example, in the LONGEVO-SCA registry,19 the CRUSADE scale had a slight predictive value in elderly patients and, among the many age-related variables, only comorbidity was associated with the appearance of hemorrhagic events. In addition, the PRECISE-DAPT scale classifies the vast majority of elderly patients as high risk, indicating the need to review the cutoff points of this scale or to validate new scales adapted to elderly patients.20
For IHD in elderly patients, the most solid evidence includes the benefits of urgent reperfusion, particularly by primary angioplasty, as recommended in current clinical practice guidelines. However, this strategy is offered less often as age increases and as patients are presumed to be more vulnerable. Once again, this is often based on a subjective impression, and not on an objective, rigorous assessment. The IFFANIAM registry21 included more than 400 elderly patients older than 75 years hospitalized due to ST-segment elevation acute coronary syndrome treated with primary angioplasty and focused on the impact of frailty in this context, observing a 1-year mortality that was 5-fold higher among frail patients with a lower body mass index. So, should clinicians include frailty and nutritional status (among other conditions seen in geriatric patients) when making decisions about ST-segment elevation acute myocardial infarction?
AORTIC STENOSISWe would like to raise a question: how many apparently vulnerable elderly (or not so elderly) patients with severe aortic stenosis (AS) are treated in our daily practice? In young patients, there are no disputes about the indications of valve replacement. However, although in recent years we have seen widespread use of transcatheter aortic valve implantation for valve replacements, further efforts are still needed. In fact, in the PEGASO registry9 of severe symptomatic AS in octogenarians (mean age, 84 years), nearly half were treated conservatively, and transcatheter aortic valve implantations and surgical aortic valve replacements were performed at similar proportions. The conservative approach was associated with> 50% 1-year mortality, and severe comorbidity had an impact on mortality, regardless of the strategy used.
The conservative approach taken with these patients has been confirmed in other studies, such as the IDEAS registry,11 which found that a large percentage of patients (64.5%), particularly those with greater comorbidity, continued to be treated conservatively and 1-year survival was again higher in patients who had undergone valve replacement. In nonagenarians with AS, a growing patient subgroup, comorbidity is clearly a determining factor for both conservative therapy and mortality, regardless of the strategy chosen.13 Greater evidence to support this has led us to consider these issues and to implement the use of CGA as a clinical tool for screening patients with severe AS.
INTERATRIAL BLOCKThe Cardiac and Clinical Characterization of Centenarians (4C)14 study showed that less than a third of centenarians had a normal P wave, and almost half had interatrial block (IAB), a condition more prevalent among elderly patients with cardiovascular disease and related to the appearance of atrial fibrillation (AF) and even related to the appearance of cerebral ischemic events with no evidence of AF. Consequently, in recent years, several studies have found that patients with advanced IAB and a high CHADS2-VASc2 score could benefit from anticoagulant therapy.15,16
Data from the BAYES registry,17 which included patients aged ≥ 70 years with structural heart disease and no known AF, showed that advanced IAB was independently associated with the development of AF and stroke during the follow-up period. Specifically designed future studies could guide treatment choices for these patients.
HEART FAILURESeveral recent studies around the world have highlighted the need to implement CGA for outpatients with heart failure. For instance, the FRAGIC study,22 with 500 patients aged ≥ 75 years, will clarify the relevance of the CGA and frailty in the prognosis of elderly patients with chronic heart failure, and will likely enhance its use as a support tool and marker of health care quality in heart failure units and cardiology outpatient clinics.
CONSENSUS DOCUMENTSAlong with research supported by the Geriatric Cardiology Section of the Spanish Society of Cardiology, work has been done on documents and manuals to collect and summarize the available evidence and to make it accessible, thus encouraging use in clinical practice. Several documents have been prepared to underscore the importance of the frailty assessment and to offer tools to measure it in each cardiovascular disease situation,23 as well as to establish guidelines on supportive care for elderly patients with heart failure24 (often unfamiliar to cardiologists). In recent times, the pandemic caused by the SARS-CoV-2 (COVID-19) disease has emerged as a top-level geriatric emergency, leading to new concerns about the approach taken with elderly patients in general, and those with cardiovascular disease in particular, including extraordinary measures in social and health residences and facilities at the peak of the pandemic and during the “new normal” as the lockdown is gradually lifted. In this context, a document has been prepared together with the Spanish Society of Geriatrics and Gerontology to collect available evidence on COVID-19 in elderly patients.25
CONCLUSIONS: PAST, PRESENT, AND FUTUREOver these years, many milestones have been reached in the field of geriatric cardiology, and not all of them can be mentioned in this document. Unquestionably, this small but growing section has helped to gain further knowledge and develop a comprehensive view focused on elderly patients with cardiovascular disease in various clinical situations. Additionally, the section has produced scientific evidence and practical documents that will aid the management of these patients.
The section looks to the future with enthusiasm, and new projects will look at issues such as AF in nonagenarians as well as concomitant AF and IHD in very elderly patients. Another challenge we aim to address is to analyze whether the benefits of recently introduced drugs with evidence for cardiovascular diseases in the general population are the same for this population group, which is usually underrepresented (or even excluded, when frailty, geriatric syndromes, and/or comorbidity are combined) in the main clinical trials. Therefore, our endeavors are ongoing, and we are certain they will be undertaken with effort, eagerness, and determination in upcoming years.
CONFLICTS OF INTERESTNo conflicts of interests related to this article.
We would like to express our sincere appreciation for everyone who made our accomplishments possible: to Dr José Manuel Ribera Casado for founding the section and to Dr Manuel Martínez-Sellés, Dr Albert Ariza Solé, and Dr Pablo Díez-Villanueva for their involvement in its efforts.