Keywords
INTRODUCTION
Cardiovascular disease is the main cause of death and disease in persons with diabetes mellitus.1,2 The prevalence of ischemic heart disease in patients with type 2 diabetes mellitus ranges from 10%-25%.3 Moreover, the presence of diabetes mellitus causes the protective effect of female sex to disappear in ischemic heart disease, as shown in the Rancho Bernardo study.4
Type 2 diabetes mellitus is a complex disease, with disorders in the lipid profile, blood pressure and clotting factors. However, traditional risk factors explain just 25% of the excess cardiovascular risk in patients with diabetes.5 The presence of insulin resistance might also partly explain this excess risk.6
The metabolic syndrome, or insulin resistance syndrome, consists of a combination of impaired glucose metabolism, abdominal obesity, dyslipidemia, and hypertension. The metabolic syndrome contributes to the onset of cardiovascular disease.7 The World Health Organization (WHO) has published a definition of the metabolic syndrome for operational purposes.8
Few studies have undertaken a prospective analysis of the association between insulin resistance and cardiovascular death and disease in patients with type 2 diabetes mellitus.6 The 2 aims of our study were to assess the incidence of cardiovascular disease in a cohort of patients with type 2 diabetes mellitus without proteinuria, and to determine the contribution of different components of the metabolic syndrome to the onset of cardiovascular events.
MATERIAL AND METHODS
Design
A prospective cohort study.
Study Population
From 1 June 1994 to 1 June 1998 we enrolled all patients with type 2 diabetes mellitus from the endocrinology outpatient service of the Hospital Comarcal in Alcañiz, Spain, which has a referral population of 70 000 persons, who fulfilled the following criteria: the presence of diabetes diagnosed according to WHO criteria in force at the time,9 age above 35 years at the time of diagnosis, and insulin independence for at least one year after diagnosis of the disease (n=463). Patients were excluded if they had proteinuria (n=27) or lacked data for any of the defining variables of the metabolic syndrome (n=118). The final number of participants available for follow-up was 318.
Baseline Variables
The following data were collected for each patient:
Clinical variables: age, sex, known disease duration, weight in kilos (measured in light clothing without shoes, with a precision of 500 g), height (precision of 1 cm), body mass index (BMI) defined as the weight in kg/square of the height in meters, waist diameter at the level of the umbilicus, hip diameter at the widest part of the gluteal region, calculation of the waist to hip ratio (WHR), and systolic and diastolic blood pressure (average of 3 measurements taken after 10 min seated rest, with a cuff suitable for the arm circumference and with a precision of 5 mm Hg). The patients were classified according to their smoking habits as active smokers, ex-smokers, or nonsmokers, and according to their antidiabetic therapy as being treated with diet alone, with oral anti-diabetic agents, or with insulin.
Biochemical variables: venous blood was drawn after a 10 h overnight fast and before the administration of any antidiabetic medication. A 24 h urine sample was taken and, after excluding any urinary infection, the rate of albumin excretion was measured. The samples were classified as normal albuminuria (<30 mg), microalbuminuria (30-300 mg), and macroalbuminuria or proteinuria (>300 mg).
Definition of the Metabolic Syndrome
According to the WHO,8 a person with diabetes has the metabolic syndrome if he or she fulfills 2 or more of the following criteria: hypertension (systolic pressure >160 mm Hg and diastolic pressure >90 mm Hg, or receiving blood pressure lowering therapy), dyslipidemia (triglycerides >150 mg/dL and high density lipoprotein [HDL] cholesterol <35 mg/dL in men or <40 mg/dL in women), obesity (BMI>30 and WHR>0.9 in men or >0.85 in women), and microalbuminuria (24 h urinary albumin excretion rate >30 mg).
Biochemical Methods
Measurements of total cholesterol, triglycerides, HDL cholesterol and glucose were made with a Shimadzu CL 7200 autoanalyzer. Glycosylated hemoglobin was measured in a Cobas Mira Plus automated analyzer, with a normal range of 4.5%-5.7%. Microalbuminuria was measured by immunoturbidimetry. Low density lipoprotein (LDL) cholesterol was calculated from the Friedewald equation when the triglyceride level was lower than 400 mg/dL.
Cohort Follow-up
The patients were followed up prospectively until their death (n=21; 6.6%) or until the close of the study on 31 October, 2001. New-onset angina was defined as the new onset of coronary-type pain confirmed by an ischemia induction test and coronary angiography. Myocardial infarction was defined as the presence in the clinical history on admission of chest pain with typical electrocardiographic changes and the characteristic rise and progressive fall in the levels of the creatinine kinase MB fraction and troponin I (the latter available at our hospital since February 2000). A stroke was defined as a neurologic deficit lasting longer than 24 h and a transient ischemic attack as a neurologic deficit resolving completely within 24 h. The cause of death, obtained from the hospital charts or by contacting the primary care physician who signed the death certificate, was coded according to the ICD-9. In 1 patient (0.3%) the date of death was obtained from the civil registry but the cause of death could not be determined. Two patients (0.6%) whose vital status could not be determined were considered as being lost to follow-up.
Statistical Methods
Quantitative variables were described as the mean ± standard deviation (SD) or the median and interquartile range (triglycerides). Qualitative variables were reported by their frequency distribution. The comparison of quantitative variables was made with Student t test for independent samples and comparison of qualitative variables by the chi square test, with the linear trend test when appropriate. Triglyceride levels were transformed logarithmically to normalize their distribution.
The rates of total cardiovascular events, coronary events and cerebrovascular events were expressed as the number of events per 1000 persons per year. The comparison of event-free survival between patients with and without the metabolic syndrome was made by Kaplan-Meier survival analysis and the logarithmic range test. The patients were withdrawn from the study after their first vascular event.
To assess the independent contribution of the presence or absence of the metabolic syndrome and of the number of its components to the appearance of cardiovascular events we undertook a multivariate analysis with Cox proportional hazards regression. The relative risk (RR), with its 95% confidence interval (CI), was calculated as an approximation to the hazards ratio. The main dependent variable was a combination of new-onset angina, fatal or nonfatal acute myocardial infarction (AMI), transient ischemic attack (TIA), fatal or nonfatal stroke, or lower limb amputation. Secondary dependent variables consisted of coronary events (combination of new-onset angina and fatal or nonfatal AMI) and cerebrovascular events (combination of TIA and fatal or nonfatal stroke). The main independent variable was coded binarily (0-1 component of the metabolic syndrome versus 2 or more) or in four categories (0-1/2/3/4 components) with coding according to the reference category. The models were adjusted for the variables which gave a significant prediction of events in the univariate analysis or for their clinical importance. Associations with a P<.05 were considered significant.
RESULTS
Of the 463 patients initially enrolled, 318 were finally selected. The only difference between those patients included in the study and those who were excluded was a lower initial systolic blood pressure (143 vs 149 mm Hg; P=.012). Table 1 shows the initial characteristics of the patients and the distribution of the risk factors for the metabolic syndrome in the whole group and according to whether the patients did or did not have any cardiovascular events during the follow-up. The initial prevalence of the metabolic syndrome was 77%. Those patients who had a cardiovascular event were older, had lower HDL cholesterol concentrations and a greater initial prevalence of microalbuminuria and the metabolic syndrome.
The mean duration of the follow-up was 4.6±1.5 years. There were 11 (3.5%) new-onset anginas, 8 (2.5%) nonfatal AMI, 6 (1.9%) fatal AMI, 6 (1.9%) TIA, 9 (2.8%) nonfatal strokes, 1 (0.3%) fatal stroke, and 1 (0.3%) amputation above the knee. The overall rate of cardiovascular disease was 28.6/1000 patients per year. There were 13 (4.1%) nonvascular deaths and 1 (0.3%) death from an unknown cause. The overall mortality rate was 14.3/1000 patients per year.
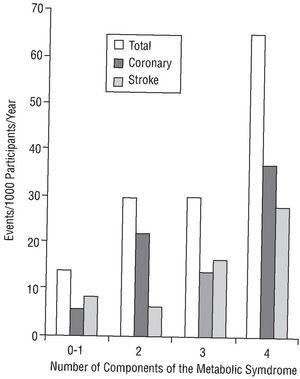
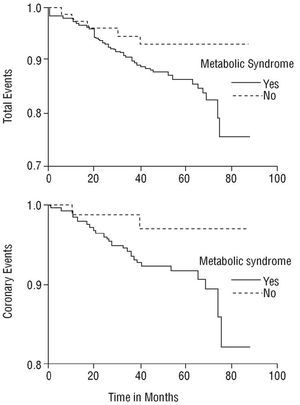
The rates of total cardiovascular disease, coronary disease and cerebrovascular disease increased as the number of components of the metabolic syndrome increased (P=.022 in the linear trend for total events; Figure 1). The respective rates of total cardiovascular disease, coronary disease and cerebrovascular disease, expressed per 1000 patients per year, were 14.0, 5.6, and 8.4 in patients without the metabolic syndrome, and 33.3, 20.7 and 11.7 in patients with the metabolic syndrome. The difference in the survival curves between patients with and without the metabolic syndrome for the main variable (total cardiovascular disease) bordered statistical significance (P=.058; Figure 2). Coronary disease-free survival was significantly different (P=.05; Figure 2), but not cerebrovascular disease-free survival (P=.63).
Fig. 1. Rate, according to the number of components of the metabolic syndrome, of total events (14.0, 29.7, 30.0, and 65.0), coronary events (5.6, 22.0, 14.0, and 37.0) and cerebrovascular events (8.4, 6.2, 16.6, and 27.8) for each 1000 patients per year. The linear trend for the increase in the risk of events as the number of components of the metabolic syndrome increased was significant for total events (P=.022), but not for coronary or cerebrovascular events individually.
Fig. 2. Total event-free survival curve (RR=2.4; P=.06, Mantel-Cox) and coronary event-free survival (RR=3.8; P=.06, Mantel-Cox) in patients with (n=245) and without (n=73) defining criteria of the metabolic syndrome.
In the Mantel-Cox univariate analysis, the presence of the metabolic syndrome increased the risk for overall vascular disease (RR=2.4; 95% CI, 0.9-6.1; P=.06) and for coronary disease (RR=3.8; 95% CI, 0.9-16.3; P=.06) to the limit of statistical significance, but the risk for cerebrovascular disease did not increase (RR=1.3; 95% CI, 0.4-4.7; P=NS). After introducing the components of the metabolic syndrome coded into four categories, the presence of four components significantly increased the overall risk for disease (RR=4.7; 95% CI, 1.5-14.9; P=.008) and the risk for coronary disease (RR=7.0; 95% CI, 1.3-38.0; P=.025), but not the risk for cerebrovascular disease (RR=3.2; 95% CI, 0.6-16.0; P=NS). Other predictors of overall vascular disease, coronary disease and cerebrovascular disease with a P<.1 in the univariate analysis are shown in Table 2.
Adjustment in the multivariate analysis was made for age, smoking, and glycosylated hemoglobin. No adjustment was made for HDL cholesterol or microalbuminuria because they already formed part of the metabolic syndrome. This adjustment resulted in no clinically important modification in risk conferred by the presence of the metabolic syndrome for total events (RR=2.3; 95% CI, 0.9-5.9; P=.08) or coronary events (RR=3.7; 95% CI, 0.9-15.7; P=.08), nor did it modify the risk conferred by the simultaneous presence of all four components for overall disease (RR=5.0; 95% CI, 1.6-15.9; P=.006) or coronary disease (RR=7.4; 95% CI, 1.3-41.1; P=.02).
DISCUSSION
The main finding of this study was the increased total cardiovascular and coronary risk in those patients with type 2 diabetes mellitus who had a greater number of defining signs of the metabolic syndrome. The prevalence of the metabolic syndrome depends on the definition of its components. A recent study using the WHO criteria showed the prevalence of the metabolic syndrome in patients with type 2 diabetes mellitus to be similar to that our population, around 80%.10 Obesity was also the most prevalent component in our patients. These data agree with those obtained by quantification of insulin resistance: thus, in the study by Bruneck,11 the prevalence of insulin resistance using the HOMA model was 84% in patients with type 2 diabetes mellitus.
The clinical importance of the metabolic syndrome concerns its potential impact on cardiovascular death and disease in patients both with and without diabetes. In the study by Lakka et al,12 which excluded diabetic patients, the presence of the metabolic syndrome tripled the risk of cardiovascular death. Likewise, in the study by Lehto et al13 of patients with type 2 diabetes mellitus, the association of a high BMI, hypertriglyceridemia, decreased HDL cholesterol and hyperinsulinemia predicted cardiovascular death. The presence of the metabolic syndrome, as defined by the WHO, was associated with coronary disease in patients with type 2 diabetes mellitus in 2 studies by Isomaa et al, with a relative risk of 3.8414 and 2.23,10 respectively. In our study, the metabolic syndrome was associated with an adjusted RR of 2.3 for overall cardiovascular disease and 3.7 for coronary disease, which is in agreement with the studies mentioned above. The prediction of vascular risk due to the presence of the metabolic syndrome is hardly surprising, as its components have all been individually associated with cardiovascular death and disease in many studies and have been the subject of attention of different scientific societies.15-18
The most characteristic form of dyslipidemia in patients with type 2 diabetes mellitus is an increase in triglycerides and a decrease in HDL cholesterol.19 A large study published in 1997,20 which included data on 1059 patients with type 2 diabetes mellitus and a follow-up of seven years, showed that coronary death was associated, after multivariate adjustment, with an increase in triglycerides, a decrease in HDL cholesterol, the non HDL cholesterol concentration and the ratio of HDL cholesterol to total cholesterol. This reflects the importance of dyslipidemia in the definition of the metabolic syndrome.
In the Multiple Risk Factor Intervention Trial21 the annual death rate in the subgroup of diabetic patients rose from 0.5 in those with a systolic blood pressure below 120 mm Hg to 2.4% in those with a systolic blood pressure above 200 mm Hg.
Excess abdominal fat in patients with type 2 diabetes mellitus has been associated with poor metabolic control, dyslipidemia and cardiovascular complications.22 However, no prospective studies have analyzed the specific contribution to mortality of the WHR in patients with type 2 diabetes mellitus, probably because of the high prevalence of increases in this ratio in this particular group of patients, as reflected in our study.
A metaanalysis23 showed that the odds ratio conferred by the presence of microalbuminuria to the onset of fatal and nonfatal cardiovascular events was 2. Two explanations have been proposed for the increase in cardiovascular death and disease in patients with microalbuminuria. Microalbuminuria itself could be an indicator of the metabolic syndrome or it could be a complication resulting from the hyperglycemia and hypertension, leading to a state of generalized endothelial dysfunction.24
The data resulting from this study confirm the etiologic importance of the various components of the metabolic syndrome in the cardiovascular risk of patients with type 2 diabetes mellitus in our area. The simultaneous presence of 4 components of the metabolic syndrome was significantly associated with cardiovascular and coronary disease. This association was seen after adjusting for other potentially confounding factors, for the temporal sequence of the study, evidenced by its prospective nature, and for the increase in the risk of cardiovascular events with the increase in the number of defining components of the metabolic syndrome. The study also showed the dose-response curve which supports the concept of causality. The presence of the metabolic syndrome according to the WHO definition (2 or more components) was at the limit of statistical significance, probably because of the reduced number of patients.
One limitation of the study is the fact that patients with proteinuria were excluded because microalbuminuria was a defining sign of the metabolic syndrome, as were patients with incomplete data. This exclusion of patients whose data were incomplete reduced the statistical power of the study, but it is unlikely to have resulted in a selection bias, because the only difference between the patients included and those excluded was their initial systolic blood pressure. Another limitation was the failure to include any direct or indirect measurement of insulin resistance, as both the HOMA model6 and insulin dose25 are considered independent vascular risk factors in patients with type 2 diabetes mellitus. Neither is it possible to rule out the fact that the National Cholesterol Education Program (ATP-III) definition of the metabolic syndrome26 might have produced different results, as this definition does not include the presence of microalbuminuria. Finally, the patients all came from a specialized outpatient clinic, and may not therefore be representative of all patients with type 2 diabetes mellitus.
Given that type 2 diabetes mellitus is a heterogeneous disease, with a variable proportion of insulin resistance and secretion defects, and that the vascular risk is greater in patients with marked insulin resistance,27 it is important to detect these patients clinically in order to apply suitable preventive measures. Furthermore, the prognosis after a coronary event is worse in patients with diabetes than in nondiabetic patients.28
CONCLUSIONS
In a group of patients with type 2 diabetes mellitus we saw that the simultaneous presence of all four components of the metabolic syndrome, as defined by the WHO, is associated with an increase in overall cardiovascular risk and in coronary risk. The data from our study support the use of the WHO definition of the components of the metabolic syndrome for predicting risk. We therefore consider this definition useful for detecting the subgroup of patients with type 2 diabetes mellitus with a greater degree of insulin resistance and a higher risk of cardiovascular events.
ABBREVIATIONS
RR: relative risk.
WHO: World Health Organization.
BMI: body mass index.
WHR: waist to hip ratio.
AMI: acute myocardial infarction.
TIA: transient ischemic attack.
HDL: high density lipoprotein.
LDL: low density lipoprotein.
Correspondence: Dr. J.A. Gimeno Orna.
Balbino Orensanz, 19, 2.o B. 50014 Zaragoza. España.
E-mail: mjpnosti@eresmas.com