Marfan syndrome (MS) is a multisystem autosomal dominant genetic disorder affecting the connective tissue with the main manifestations involving the cardiovascular, skeletal, and ocular systems. Aortic involvement predisposes to aortic dissection and rupture and is the main cause of early mortality. The dissection risk rises with increasing aortic size, and prophylactic surgical replacement of the aorta is performed when the aorta is dilated. During pregnancy, women with MS are at further increased risk of aortic dissection and progressive dilation compared with the nonpregnant period.1,2 Overall, aortic dissection occurs in approximately 3% to 5% of MS pregnancies,2–5 with most events occurring during the last trimester of pregnancy or early postpartum.1,2,6 Both hemodynamic and hormonal factors have been implicated in the pathobiology of aortic dissection during pregnancy. The hypervolemic and hyperdynamic state of pregnancy increases aortic wall stress and intimal shear forces. At the same time, hormonal changes lead to fragmentation of the reticulum fibers, a reduction in acid mucopolysaccharides, and loss of the normal corrugation of elastic fibers. These changes explain the normal increase in the aortic wall of healthy pregnant women, but in women with MS there can be additional extracellular matrix degradation, less vessel support, further dilatation, and increased risk of aortic dissection.2,7–10 While the thoracic aorta is the most common vessel to dissect during pregnancy in women with MS, there have also been reports of dissection of other arterial vessels.6 There are a number of risk factors for arterial dissection in patients with MS, including genotype, older age, hypertension, and aortic dimension.1,2,5–7 During pregnancy, the risk of type A thoracic aortic dissection is related to the dimensions of the thoracic aorta, whereas type B dissection has not been shown to be related to aortic diameter. Some experts also speculate that lactation may be a risk factor for aortic dissection, as murine studies have shown that the risk of postpartum dissection was decreased by withholding lactation or through administration of an oxytocin receptor antagonist; however, studies in humans are lacking.9
While no pregnant woman with MS is totally risk free from the risk of aortic dissection, those with smaller aortic dimensions (less than 4.0cm) are generally considered at lower risk, with dissection occurring in approximately 1% of pregnancies.7 However, the aortic dimension associated with a “relatively safer” pregnancy and the threshold for elective aortic repair prior to pregnancy are still under debate, with thresholds for “high risk” ranging from 4.0cm to 4.5 cm. The 2010 American Heart Association Guidelines for the Diagnosis and Management of Patients with Thoracic Aortic Disease suggest that an aortic dimension of 4.0cm identifies women at highest risk during pregnancy, while the European Society of Cardiology Guidelines for the Management of Cardiovascular Disease during Pregnancy and the Canadian Cardiovascular Society: Clinical Practice Update on Cardiovascular Management of the Pregnant Patient recommend prophylactic surgery in patients with aortic root diameters above 4.5cm or above 4.0cm in the presence of high-risk features.11–13 However, data to support these recommendations have limitations and are based on studies with small numbers of aortic events and differences in surveillance and treatment strategies among study cohorts.3,5,14,15 Furthermore, in many studies, the women were not diagnosed prior to pregnancy and did not receive routine MS care during pregnancy. Lack of MS diagnosis prior to pregnancy is an important contributing factor to poor outcomes.4,14
In a recent research article published in Revista Española de Cardiología, Martín et al.15 report on a large retrospective multicenter cohort of 133 pregnancies in 89 women with MS seen between 2004 and 2020 and followed up in 2 dedicated Marfan units in Madrid (Hospital Universitario Puerta de Hierro) and Barcelona (Hospital Universitario Vall d’Hebron). The endpoint of interest was adverse aortic events during pregnancy and consisted of a composite of aortic dissection or rapid aortic root growth (≥ 3mm) requiring aortic surgery during pregnancy or in the postpartum period. In addition, late survival (median 8.6 years after pregnancy) and survival free from adverse aortic events in women with MS who had pregnancies were compared with 234 women with MS who had never been pregnant. In that study cohort, aortic events occurred in 3.7% of pregnancies and were secondary to 5 events (2 type A dissections, 1 type B dissection, and 2 patients with a rapid increase in root diameters) and the rate of aortic dissection was 2.2%. All events occurred in the third trimester or postpartum. There was no difference in long-term survival free of aortic events (dissection or elective aortic surgery) or death in women who had a pregnancy (without aortic complications) compared with those who were never pregnant.
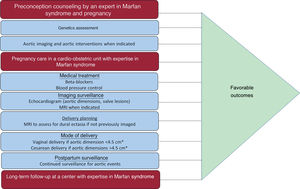
Favorable pregnancy outcomes in the study by Martín et al. were likely related to multiple factors, including the care provided to pregnant women in their MS units. The authors describe the management of patients in their MS clinics, including multidisciplinary team involvement, family screening, imaging surveillance, and access to medical and surgical MS therapies. Prophylactic aortic surgery is important to prevent complications during pregnancy and guidelines suggest that pregnancy should be avoided and prophylactic aortic replacement be performed prior to pregnancy in women with aortic dimensions> 4.5cm.12 In the study by Martín et al., 9% of the women had aortic surgery prior to pregnancy although the size of the aortic root at the time of prophylactic surgery is not reported. Beta-blockers during pregnancy are also advised to prevent aortic complications.12,16 Excellence in care in the MS units is highlighted by the fact that more than 80% of women were treated with beta-blockers during pregnancy. Additional guideline recommendations include frequent echocardiographic assessments, every 4 to 12 weeks (depending on the prepregnancy aortic diameter), during pregnancy, and up to 6 months postpartum, and a preference for vaginal deliveries in women with aortic dimensions less than 4.0cm.12 Vaginal deliveries occurred in more than 60% of the deliveries in the study by Martín et al. Data from MS units, such as these, provide helpful estimates of pregnancy risk when guideline-directed preconception interventions and pregnancy care are followed (figure 1).
Recommendations for the management of women of childbearing age with Marfan syndrome.* See Regitz-Zagrosek et al.12
The study by Martín et al. further adds to our understanding of the risks of aortic complications both during and after pregnancy. Four of the 5 women who experienced an aortic event had an aortic diameter less than 4.5cm and women with aortic diameters greater than 4.0cm had higher aortic event rates than those with smaller aortic diameters (18.7% vs 2.7%; P=.058). While the aortic threshold for intervention prior to pregnancy will likely continue to be debated, data from this study support a threshold for prophylactic aortic surgery of 4.0cm or more prior to pregnancy. Furthermore, this study reports the long-term impact of pregnancy on the MS aorta. Some prior studies have suggested that pregnancy had a small but significant influence on aortic growth, as well as rates of aortic complications in the long-term.1,2 However, Martín et al.15 found no significant differences in the incidence of aortic events or death in pregnant vs never-pregnant patients. Their study provides important additional data about MS outcomes during pregnancy in a large contemporary Spanish cohort followed up in experienced MS units. Despite excellent care, complications occurred during and after pregnancy, highlighting the importance of lifelong follow-up in this population.
FUNDINGC.K. Silversides is supported by the Miles Nadal Chair in Pregnancy and Heart Disease (Mount Sinai Hospital Foundation).
CONFLICTS OF INTERESTThe authors have no conflicts of interest.