Only a few studies have reported nationwide population-based data on the magnitude and control of hypercholesterolemia. This work examines the prevalence and management of hypercholesterolemia in Spain.
MethodsCross-sectional study conducted from June 2008 to October 2010 on 11 554 individuals representative of the population aged ≥18 years in Spain. Study participants provided 12-h fasting blood samples, which were analyzed in a central laboratory with standardized methods.
ResultsIn the whole population, 50.5% had hypercholesterolemia (total cholesterol ≥200mg/dL or drug treatment) and 44.9% high levels of low-density lipoprotein cholesterol (≥130mg/dL or drug treatment), with no substantial sex-related differences. Moreover, 25.5% of men showed high-density lipoprotein cholesterol <40mg/dL and 26.4% of women high-density lipoprotein cholesterol <50mg/dL. Also, 23.2% of men and 11.7% of women had triglycerides ≥150mg/dL. Frequency of dyslipidemia increased up to 65 years, except for low high-density lipoprotein cholesterol which did not vary with age. Among those with high low-density lipoprotein cholesterol, 53.6% knew of it and 44.1% of them received lipid-lowering treatment; among the latter, 55.7% had a controlled level (13.2% of all hypercholesterolemics). Control of high low-density lipoprotein cholesterol increased with age and with the number of visits to the specialist physician, but was lower among diabetics (odds ratio = 0.38; 95% confidence interval, 0.28-0.53) and patients with cardiovascular disease (odds ratio = 0.55; 95% confidence interval, 0.33-0.92).
ConclusionsAbout half of the Spanish population has elevated serum cholesterol; moreover, cholesterol control is poor, particularly among those with highest cardiovascular risk, such as diabetics or patients with cardiovascular disease.
Keywords
.
IntroductionTotal serum cholesterol (TC) and low density lipoprotein (LDL) cholesterol are independently associated with a high, continuous risk of ischemic heart disease,1, 2 even in young people3 and populations with a low risk of coronary heart disease.4 Nevertheless, effective, safe, and inexpensive treatments are available to control high cholesterol and the associated cardiovascular risk.5
Knowing more about the extent of the problem and the way blood lipids are managed can lead to a better understanding of how coronary risk varies between populations,6, 7 or within the same population over time.8 Most importantly, it can help identify opportunities for reducing cardiovascular risk and establish which individuals can most benefit.9 National population-based studies on the distribution and management of blood cholesterol have only been carried out in a few countries.10, 11, 12, 13, 14, 15 Similarly, information on LDL and triglycerides (TGC), ie, the lipid fraction on which treatment targets are based,5, 16 appears to be available only for the United States11, 13, 14 and China.10
Only two population-based nationwide studies on cholesterol distribution have been conducted in Spain. The first was performed in individuals aged 35 to 64 years in 199017; however, cholesterol was assessed using dry chemistry techniques, which underestimate serum cholesterol. The second study was conducted in individuals aged between 5 and 59 years in 1992-1994.18 More recent data have come from combinations of local and regional studies.19, 20 This paper therefore reports on the prevalence and management of serum cholesterol and its fractions in the current adult population of Spain.
Methods Study Design and ParticipantsData were collected in the Nutrition and Cardiovascular Risk in Spain Study (ENRICA); ENRICA study methods have been described previously.21 Briefly, ENRICA was a cross-sectional study conducted from June 2008 to October 2010 in 12 948 individuals who were representative of the noninstitutionalized Spanish population aged 18 years and older. Participants were selected using multistage, stratified cluster sampling. The sample was first stratified by province and size of municipality. In each stratum, clusters were randomly selected in 2 stages, using municipalities and census tracts. In the next stage, households in each section were selected by random telephone dialing, using the telephone landline directory as the sampling frame. Finally, subjects in households were selected in proportion to the distribution of the Spanish population by sex and age group. Data socio-demographic characteristics, lifestyle, and use of health services was collected by telephone interview and 2 home visits. In the first home visit, blood and urine samples were obtained, and in the second a physical examination was performed and data on food consumption were collected. The overall response rate was 51%, which is among the highest seen in population health surveys including a physical examination conducted in Europe.22
All study participants provided written consent and the study was approved by the clinical research ethics committees of the Hospital Universitario La Paz in Madrid and Hospital Clínic in Barcelona.
Determination of Blood LipidsParticipants provided 12-h fasting blood samples. Total cholesterol was measured by enzymatic methods using cholesterol esterase and cholesterol oxidase. High density lipoprotein (HDL) cholesterol was measured by the direct method using elimination / catalase and LDL cholesterol was calculated using the Friedewald formula.23 Triglycerides were measured with glucose oxidase using the glycerol phosphate oxidase and glucose method. All determinations were made with the ADVIA 2400 Clinical Chemistry System (Siemens) in the Center for Biological Diagnosis at the Hospital Clínic in Barcelona; standardized procedures were followed and appropriate quality controls applied.
Definition of Hypercholesterolemia, Knowledge, and ControlParticipants were considered to have hypercholesterolemia if their TC was ≥200mg/dL or they were receiving pharmacological treatment. They were considered to have high LDL cholesterol at values of ≥130mg/dL or if they were being treated with lipid-lowering drugs.1 Since cholesterol is a continuous variable, thresholds were also analysed for TC of ≥190 and ≥240mg/dL and for LDL cholesterol of ≥115 and ≥160mg/dL to take into account criteria applied in different clinical guidelines.1, 24, 25 A TC≥310mg/dL was also considered because it is associated with cardiovascular risk independently of other risk factors.5 Low HDL cholesterol was defined as <40mg/dL in men and <50mg/dL in women,1, 24 and hypertriglyceridemia was considered to be present when TGL was ≥150mg/dL.16
Participants were considered to be aware they were hypercholesterolemic if they responded in the affirmative to the question “Have you ever been told by your doctor that you have high cholesterol?” The question “Did your doctor prescribe treatment with pills?” was used to identify participants being treated with drugs; those who answered “Yes, and I’m currently following the treatment” were selected. As recommended in the guidelines, LDL cholesterol levels were used to define cholesterol control. Cholesterol was considered controlled when LDL cholesterol was <130mg/dL, or <100mg/dL in patients with diabetes or cardiovascular disease (CVD).1, 25 Thresholds in the European guidelines (LDL cholesterol <115mg/dL, or <100mg/dL in diabetic patients or those with CVD24, 26) and in the ATP III and Spanish primary care guidelines (LDL cholesterol <100mg/dL in patients with diabetes or CVD; <160mg/dL in subjects with low cardiovascular risk, ie, no more than one classic risk factor; and <130mg/dL for other subjects) were also used.1, 25
Diet and Exercise to Manage HypercholesterolemiaThe following questions were used to assess advice on diet and exercise in subjects who were aware they were hypercholesterolemic: “Did your doctor or nurse advise you to reduce your consumption of high-fat foods or foods which are high in cholesterol?”, “Did your doctor or nurse advise you to do any physical activity, in particular, did they advise you to walk for at least 30min several days a week?“, and in overweight patients, “Has your doctor or nurse ever advised you to lose weight?”. Possible answers were: “Yes, and I am currently following their advice”, “Yes, but I’m not currently following their advice”, and “No”. In addition, all study participants were asked: “During the past year, have you had your blood cholesterol tested?” (Yes/No).
Other VariablesIn addition to sociodemographic variables, we measured weight and height in standard conditions using electronic scales and height boards.27 Body mass index (BMI) was calculated as weight (kg) divided by the square of height (in m), and categorized as BMI <25.0, overweight (BMI 25.0 to 29.9), and obese (BMI≥30). Waist circumference was measured with an extensible, flexible tape at the midpoint between the last rib and the iliac crest, at the end of normal expiration.27 Abdominal obesity was defined as waist circumference >102cm for men and >88cm for women. Blood pressure was determined under standardized conditions with validated, automatic sphygmomanometers (OMRON model M6). Patients were defined as hypertensive if they had systolic pressure of ≥140mmHg, diastolic pressure of ≥90mmHg, or if they were taking antihypertensive medication.25, 28 Diabetes was defined as fasting blood glucose >126mg/dL or treatment with oral agents or insulin.29
Subjects were asked if their doctor had ever diagnosed any CVD, including infarct or heart attack, thrombosis or stroke, and heart failure. Finally, they were asked how often they saw a primary care physician or a specialist (the 6 possible answers were grouped into three categories: <1 time/year, 1-2 times/year, and >2 times/year).
Statistical AnalysisOf the 12 948 ENRICA study participants, 140 subjects with TGC>400mg/dL were excluded as the Friedewald formula is not recommended to calculate LDL cholesterol in those individuals. We also excluded subjects without information on the following variables: hyperlipidemia (n = 84), educational level (n = 47), BMI (n = 881), waist circumference (n = 26), blood pressure (n = 88), glucose (n = 94), and other variables (n = 34). Analyses were therefore conducted using data from 11 554 individuals.
Associations between sociodemographic, lifestyle, and clinical variables and knowledge, treatment, and control of high LDL cholesterol were summarized using odds ratios (OR) and 95% confidence intervals (95%CI) derived from logistic regression models. Independent variables included in the models were sex, age, educational level, BMI, abdominal obesity, hypertension, diabetes, CVD, visits to a primary care physician, and visits to a specialist. All variables were modeled categorically using dummies. Dose-response was also tested by modeling quantitative variables as continuous variables.
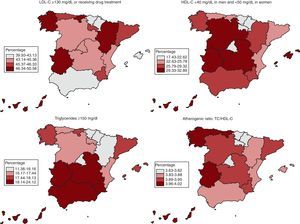
Finally, prevalence rates of high LDL cholesterol, low HDL cholesterol, and high TGC, as well as the atherogenic ratio (TC/HDL cholesterol), were calculated for each of Spain's 17 autonomous communities. For comparisons between regions, estimates were adjusted for age and sex using the direct method.
P values of <.05 were considered statistically significant. Analyses were performed using Stata survey procedure v.11 to take into account the study's complex sampling design. Observations were weighted and CI corrected based on the stratified cluster sampling design.
ResultsMean values for TC and LDL cholesterol were 195.9mg/dL and 121.2mg/dL, respectively (Table 1). Values for TC and LDL cholesterol were similar in men and women but, as expected, HDL cholesterol was higher and TGC lower in women than in men. The frequency of dyslipidemia increased up to 65 years, except for low HDL cholesterol which did not vary with age (Table 1).
Table 1. Serum Lipids in the Spanish Population Aged 18 and Over in 2008-2010, by Sex and Age
| Patients, n | Total cholesterol, mg/dL | LDL-C, mg/dL | HDL-C, mg/dL | Triglycerides, mg/dL | |
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | ||
| Total | 11 554 | 195.9 (0.5) | 121.2 (0.4) | 53.1 (0.2) | 107.6 (0.7) |
| Men | 5699 | 192.9 (0.7) | 122 (0.6) | 47 (0.2) | 120 (1.2) |
| Age, years | |||||
| 18-29 | 1164 | 165.4 (1.3) | 100.1 (1) | 46.2 (0.3) | 95.5 (2.3) |
| 30-44 | 1828 | 198.2 (1) | 127.1 (0.8) | 46.1 (0.3) | 124.9 (2.3) |
| 45-64 | 1700 | 206.5 (1) | 132.2 (0.9) | 47.5 (0.3) | 134.3 (1.9) |
| ≥65 | 1007 | 192.2 (1.4) | 120.7 (1.2) | 48.8 (0.4) | 113.5 (1.9) |
| Women | 5855 | 198.8 (0.6) | 120.5 (0.5) | 59.1 (0.2) | 95.9 (0.8) |
| Age, years | |||||
| 18-29 | 1049 | 174.3 (1.3) | 99.2 (1) | 58.9 (0.4) | 81.3 (1.5) |
| 30-44 | 1741 | 188.7 (0.9) | 113.9 (0.8) | 58.5 (0.4) | 81.6 (1.2) |
| 45-64 | 1736 | 213.9 (1) | 133.0 (0.8) | 60.1 (0.4) | 104.7 (1.4) |
| ≥65 | 1329 | 211.3 (1.1) | 129.6 (0.9) | 58.9 (0.5) | 114.4 (1.8) |
HDL-C, high-density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; SE, standard error.
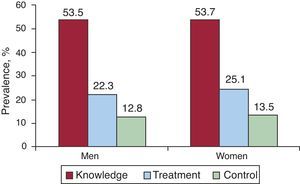
A total of 50.5% of the adult population was hypercholesterolemic (TC ≥200mg/dL or on drug treatment) and 44.9% had high LDL cholesterol (LDL cholesterol ≥130mg/dL or on drug treatment). There were no significant differences between sexes. When thresholds for TC and LDL cholesterol were reduced to ≥190mg/dL and ≥115mg/dL, the prevalence of hypercholesterolemia increased to about 60%, whereas when thresholds of ≥240mg/dL and ≥160mg/dL were used prevalence decreased to 22% (Table 2). Notably, 0.5% of the population had TC ≥310mg/dL. We found that 25.5% of men had low HDL cholesterol compared to 26.4% of women, and 23.2% and 11.7%, respectively, had hypertriglyceridemia. As with the mean lipid values, the frequency of dyslipidemia increased up to 65 years, except for low HDL cholesterol which did not vary with age (Table 2). Applying these prevalence rates to the Spanish population aged 18 years and over in 2009 would give figures of approximately 19.5 million individuals with high TC, 17.3 million with high LDL cholesterol, 10 million with low HDL cholesterol, and 6.7 million with hypertriglyceridemia. Of the individuals with high LDL cholesterol, 53.6% were aware that they were hypercholesterolemic and, of those, 44.1% were receiving lipid-lowering drugs; 55.7% were controlled. Therefore, 23.7% of all subjects with high LDL cholesterol in the population were treated and 13.2% were controlled. There were no substantial differences between sexes in the management of high LDL cholesterol (Figure 1).
Table 2. Prevalence of Dyslipidemia in the Spanish Population Aged 18 and Over in 2008-2010, by Sex and Age
| Patients, n | Total cholesterol, % (SE) | LDL-C, % (SE) | HDL-C, % (SE) | Triglycerides, % (SE) | |||||
| ≥190 mg/dL * | ≥200 mg/dL * | ≥240 mg/dL * | ≥115 mg/dL * | ≥130 mg/dL * | ≥160 mg/dL * | <50 mg/dL in men and <40 mg/dL in women | ≥ 150 mg/dL | ||
| Total | 11 554 | 59.3 (0.6) | 50.5 (0.6) | 21.9 (0.4) | 61.4 (0.6) | 44.9 (0.6) | 21.4 (0.5) | 26 (0.5) | 17.4 (0.4) |
| Men | 5699 | 57.1 (0.9) | 48.4 (0.8) | 20.6 (0.7) | 63 (0.9) | 46.1 (0.9) | 21.8 (0.7) | 25.5 (0.8) | 23.2 (0.7) |
| Age, years | |||||||||
| 18-29 | 1164 | 20.8 (1.7) | 15.3 (1.6) | 1.9 (0.5) | 28.1 (1.7) | 13.5 (1.5) | 2.1 (0.5) | 23.8 (1.9) | 11.8 (1.3) |
| 30-44 | 1828 | 57.6 (1.4) | 46.9 (1.4) | 15.2 (0.9) | 66 (1.3) | 44.9 (1.4) | 16.9 (1.2) | 29.5 (1.5) | 26.3 (1.5) |
| 45-64 | 1700 | 75.5 (1.3) | 67.2 (1.3) | 32.9 (1.3) | 78.6 (1.3) | 63.8 (1.4) | 34.9 (1.3) | 25.2 (1.3) | 30.4 (1.3) |
| ≥65 | 1007 | 67.1 (1.8) | 57.5 (2) | 31.1 (1.8) | 71.7 (1.7) | 56.3 (1.9) | 31.3 (1.8) | 21.1 (1.5) | 18.6 (1.4) |
| Women | 5855 | 61.5 (0.8) | 52.5 (0.8) | 23.1 (0.7) | 59.7 (0.8) | 43.6 (0.8) | 21 (0.7) | 26.4 (0.7) | 11.7 (0.5) |
| Age, years | |||||||||
| 18-29 | 1049 | 31.3 (1.8) | 22.7 (1.7) | 3.8 (0.7) | 25.1 (1.8) | 12 (1.3) | 2 (0.5) | 26.2 (1.4) | 6 (0.8) |
| 30-44 | 1741 | 46.1 (1.4) | 33.7 (1.3) | 7.3 (0.7) | 46.7 (1.5) | 27 (1.2) | 6.3 (0.6) | 26.9 (1.2) | 7.3 (0.7) |
| 45-64 | 1736 | 78 (1) | 70.2 (1.1) | 33.3 (1.1) | 76.5 (1.1) | 59.8 (1.3) | 29.9 (1.1) | 24.8 (1.3) | 14.5 (0.9) |
| ≥65 | 1329 | 83.8 (1.2) | 77.6 (1.3) | 45.8 (1.7) | 82.2 (1.2) | 69.2 (1.5) | 43.5 (1.7) | 28.1 (1.6) | 18.2 (1.4) |
HDL-C, high-density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; SE, standard errors.
* Or being treated with lipid-lowering drugs.
Figure 1. Knowledge, drug treatment, and control of hypercholesterolemia in the Spanish population aged 18 and over in 2008-2010. Cholesterol control: low density lipoprotein cholesterol (LDL-C) <130mg/dL (<100mg/dL in patients with diabetes or cardiovascular disease). Percentages are calculated for all subjects with high LDL-C (≥130mg/dL or receiving lipid-lowering drugs).
Using the thresholds in the European guidelines (LDL cholesterol <115mg/dL and <100mg/dL in diabetics or those with CVD),24 high LDL cholesterol was controlled in only 40.2% of subjects receiving lipid-lowering drugs. Using more rigorous thresholds (LDL cholesterol <115mg/dL and <70mg/dL in diabetics or individuals with CVD),5 only 31.3% were controlled. O the other hand, using the less stringent ATP III1 and Spanish primary care guidelines,25 66.4% were controlled.
Notably, of individuals with high LDL cholesterol treated with lipid-lowering drugs who had diabetes or CVD, only 40.5% and 43.6%, respectively, had LDL cholesterol <100mg/dL and only 7.0% and 5.2% had LDL cholesterol <70mg/dL.
Both patient awareness and drug treatment of cholesterol increased with age, and were more frequent in diabetics, those with CVD, and those who visited their doctor more often, especially primary care doctors (Table 3). Drug treatment was less frequent in women but more common among all patients with high blood pressure. Control over cholesterol levels increased with age and was more frequent in hypertensive patients and those making more frequent visits to a doctor, particularly a specialist; control was less frequent in diabetics and those with CVD (Table 3).
Table 3. Variables Associated With Knowledge, Treatment, and Control of Hypercholesterolemia in the Spanish Population Aged 18 and Over in 2008-2010
| Knowledge (n=5182) | Treatment in subjects with high cholesterol (n=2778) | Control in treated subjects (n=1226) | |
| Sex | |||
| Men | 1 | 1 | 1 |
| Women | 0.88 (0.76-1.03) | 0.75 (0.60-0.94) a | 0.79 (0.58-1.06) |
| Age, years | |||
| 18-29 | 1 | 1 | 1 |
| 30-44 | 1.17 (0.82-1.67) | 1.92 (0.77-4.79) | 4.82 (0.81-26.75) |
| 45-64 | 1.86 (1.32-2.64) b | 6.82 (2.80-16.63) b | 4.93 (0.86-28.15) |
| ≥65 | 1.94 (1.34-2.80) b | 13.89 (5.56-34.69) b | 6.21 (1.09-35.44) a |
| Linear trend, P | <.001 | <.001 | .036 |
| Educational level | |||
| Primary or under | 1 | 1 | 1 |
| Secondary | 1.06 (0.90-1.25) | 0.81 (0.63-1.004) | 0.91 (0.64-1.29) |
| University | 1.00 (0.83-1.21) | 0.77 (0.58-1.002) | 1.19 (0.81-1.76) |
| Linear trend, P | .812 | .055 | .529 |
| BMI (Kg/m2) | |||
| <25 | 1 | 1 | 1 |
| 25.0-29.9 | 1.19 (0.99-1.42) | 1.15 (0.87-1.53) | 1.43 (0.94-2.19) |
| ≥30 | 1.23 (0.96-1.56) | 1.22 (0.85-1.74) | 1.49 (0.90-2.49) |
| Linear trend, P | .073 | .289 | .165 |
| Abdominal obesity | |||
| No | 1 | 1 | 1 |
| Yes | 1.05 (0.88-1.27) | 1.14 (0.88-1.48) | 1.07 (0.75-1.54) |
| High blood pressure | |||
| No | 1 | 1 | 1 |
| Yes | 1.09 (0.94-1.27) | 1.45 (1.16-1.81) b | 1.35 (1.01-1.81) a |
| Diabetes | |||
| No | 1 | 1 | 1 |
| Yes | 1.90 (1.44-2.50) b | 3.01 (2.03-4.46) b | 0.38 (0.28-0.53) b |
| Cardiovascular disease | |||
| No | 1 | 1 | 1 |
| Yes | 2.18 (1.31-3.62) c | 2.05 (1.02-4.13) a | 0.55 (0.33-0.92) a |
| Primary care visits | |||
| <1 per year | 1 | 1 | 1 |
| 1-2 per year | 1.38 (1.15-1.66) b | 2.36 (1.70-3.27) b | 1.24 (0.72-2.17) |
| >2 per year | 1.64 (1.35-2.00) b | 4.01 (2.87-5.60) b | 1.35 (0.79-2.31) |
| Linear trend, P | <.001 | <.001 | .331 |
| Visits to specialist | |||
| <1 per year | 1 | 1 | 1 |
| 1-2 per year | 1.18 (1.01-1.37) c | 1.33 (1.05-1.69) a | 1.19 (0.87-1.63) |
| >2 per year | 1.19 (0.93-1.53) | 1.41 (0.96-2.07) | 1.65 (1.03-2.64) a |
| Linear trend, P | .027 | .016 | .042 |
95%CI, 95% confidence interval; BMI, body mass index; LDL-C, low density lipoprotein cholesterol;
OR, odds ratio.
Data are shown as OR (95% CI) adjusted for all variables in the table.
Cholesterol: LDL-C ≥130mg/dL or receiving lipid-lowering drugs. Control of cholesterol: LDL-C <130mg/dL (<100mg/dL for patients with diabetes or cardiovascular disease).
a P≤.05.
b P≤.001.
c P≤.01.
Among those who were aware they were hypercholesterolemic, 76.1% received and acted on advice to follow a diet low in fat and cholesterol, while 48.0% received and followed advice on performing physical activity. Among those with hypercholesterolemia who were overweight, 26.5% were advised to lose weight and said that they were doing so (Table 4). On the other hand, 85.6% of patients with high cholesterol who knew they were hypercholesterolemic and 64.0% of those who were unaware they had high cholesterol had had their cholesterol levels tested in the previous year.
Table 4. Medical or Nursing Advice on Lifestyle in Adults With Hypercholesterolemia in Spain, 2008-2010
| Patients, n | 2778 |
| Advice on a low fat and low cholesterol diet | |
| Received and followed advice | 2115 (76.1) |
| Received advice but did not follow it | 380 (13.7) |
| Did not receive advice | 283 (10.2) |
| Advice on physical activity | |
| Received and followed advice | 1333 (48) |
| Received advice but did not follow it | 556 (20) |
| Did not receive advice | 889 (32) |
| Advice on weight loss * | |
| Received and followed advice | 340 (26.5) |
| Received advice but did not follow it | 234 (18.2) |
| Did not receive advice | 712 (55.4) |
Data are shown as n (%).
* Calculated on 1,286 participants with BMI ≥25.
Figure 2 shows that the Basque Country, Chartered Community of Navarre, Community of Madrid, and Valencian Community had prevalence rates for high LDL cholesterol, low HDL cholesterol, and high TGC which were below the median, while Galicia, Canary Islands, Extremadura, and Region of Murcia had rates above the median. The atherogenic ratio was lower in the Basque Country, Chartered Community of Navarre, Community of Madrid, and La Rioja, and higher in Galicia, Canary Islands, Extremadura, and Principality of Asturias. Geographic variations were significant for low HDL cholesterol and high TGC, but were small for the atherogenic ratio.
Figure 2. Geographical distribution of hypercholesterolemia in the Spanish population aged 18 and over in 2008-2010 (LDL-C ≥130mg/dL or drug treatment, HDL-C <40mg/dL in men and <50mg/dL in women, triglycerides ≥150mg/dL, and atherogenic ratio: TC/HDL-C). Data adjusted for age and sex. HDL-C, high-density lipoprotein cholesterol, LDL-C, low density lipoprotein cholesterol; TC, total serum cholesterol.
DiscussionThis study has shown that half of the Spanish adult population has high cholesterol and that it is, in general, poorly controlled. Control is particularly poor in people with diabetes or CVD.
The prevalence of hypercholesterolemia in Spain is similar to that of the United States in 2006 and England in 2003.12, 30 Interestingly, although high cholesterol is the single most important coronary risk factor, mortality from ischemic heart disease is much lower in Spain than in the United States31 and England.32 This may be because cardiovascular risk depends on several risk factors, not just one. An earlier study using regional data showed that the lower coronary risk in Spain compared to the United States cannot be explained by traditional cardiovascular risk factors alone.33
Cholesterol control is rather poor in Spain. This study has shown that there is room for improvement regarding identification, lifestyle advice, and drug treatment in people with hypercholesterolemia. It is striking that 46.4% of hypercholesterolemic individuals are not aware that they have high cholesterol, even though 64% of them reported having their cholesterol tested in the previous year. This lack of awareness could be due to several factors. First, some doctors may only inform their patients that they have high cholesterol when their levels exceed thresholds (TC and LDL cholesterol ≥240 and ≥160mg/dL) which might be considered more appropriate for a country such as Spain, with low coronary risk. On the other hand, the finding may also reflect problems in doctor-patient communication which lead to patients having a poor understanding of the results of the analyses.
There is also room for improvement in the management of cholesterol through diet and physical activity, as only 76% of hypercholesterolemic subjects reported receiving and following dietary advice, while fewer than half reported receiving and following advice on physical activity and weight control. Diet and physical activity can help normalize cholesterol levels or reduce the need for drugs.5, 24 All patients should receive structured advice and, above all, training on how to modify their lifestyle in a changing society where the traditional Mediterranean diet is less frequently followed34 and levels of physical inactivity are increasing.35
Treatment with lipid-lowering drugs was less common in women than in men. This may be due to lower cardiovascular risk in women and the fact that clinical guidelines recommend treatment with drugs primarily in higher risk hypercholesterolemic patients. Unfortunately, we could not calculate the frequency of treatment according to baseline cardiovascular risk because we had no data on pre-treatment cholesterol and blood pressure values.
Finally, even when receiving treatment, only 55.7% of subjects manage to control their cholesterol, a surprisingly low proportion given that available drugs are effective and safe. Cholesterol control is particularly low in people with diabetes or CVD (40.5% and 43.6%, respectively). This is partly because these patients have more stringent treatment goals (<100 or <70mg/dL in guidelines); with goals of <130mg/dL, 75.2% of diabetics and 73.6% of individuals with CVD would have been controlled. However, our study shows that cholesterol control in these patients needs to be substantially improved, because they are at greater cardiovascular risk and are therefore the individuals who can most benefit from treatment.
As expected, and as a previous study in the United States showed,14 awareness, treatment, and control of hypercholesterolemia increases with the number of doctor visits. The association between better control of hypercholesterolemia and medical consultation was stronger for the specialist than for primary care physicians. This could be explained by the fact that poor control of cholesterol in primary care is an indication for referral to a specialist.
Our results illustrate that TC overestimates the risk associated with cholesterol in women because they have higher HDL cholesterol than men. Specifically, TC (≥200mg/dL) suggests 52.5% of women are hypercholesterolemic, compared to only 43.6% when LDL cholesterol (≥130mg/dL) is used. The present study also illustrates the influence of different clinical practice guidelines in determining the prevalence and degree of control of hypercholesterolemia. Among hypercholesterolemic subjects receiving drug treatment, control of high LDL cholesterol ranged from 31% when the highest standards in European guidelines were applied, to 66% using the less stringent criteria in the ATP III and Spanish primary care guidelines. This large variation may generate uncertainty among medical staff and health care managers regarding the quality of health care and may hinder the adoption of strategies for improvement.
There is a substantial geographic variation in the distribution of dyslipidemia, particularly as regards low HDL cholesterol and high TGC. This indicates both the level of health inequities as well as the potential for cardiovascular prevention if lipid values in the regions with the worst rates could be brought more in line with those in the regions with better rates. It is not clear what underlies these geographic variations in dyslipidemia in Spain. However, the geographic distribution of low HDL cholesterol and high TGC was similar to the pattern seen with obesity.27 In fact, the adjusted rates of low HDL cholesterol correlated with central obesity (r = 0.72 in men and r = 0.63 in women) and general obesity (r = 0.58 and r = 0.60 in men and women). Similarly, the adjusted rates of high TGC also correlated with central obesity (r = 0.44 in men and r = 0.41 in women) and general obesity (r = 0.40 in men and r = 0.73 in women).
LimitationsThis study had some limitations. First, the fact that we did not include the institutionalized population, which is usually elderly and often hypercholesterolemic, may have led us to underestimate the prevalence of hypercholesterolemia. Similarly, as in other population surveys, some selection bias cannot be excluded, as the main reason for not participating in the study was the extraction of blood. Furthermore, if this bias exists, it is not possible to know how it might affect the study results. Second, information on drug treatment and lifestyle advice received and adhered to was based on patient report, which may be subject to errors of interpretation and memory. Thirdly, it is possible that some people with high cholesterol followed the lifestyle advice and achieved control, in which case they would be wrongly classified as normocholesterolemic. However, as in other studies, this is likely to have affected only a small proportion of subjects and would only have a minor influence on the prevalence of hypercholesterolemia.
ConclusionsHigh cholesterol levels are poorly controlled in Spain, particularly among individuals with higher levels of cardiovascular risk, such as those with diabetes or CVD. A determined approach to tackling these problems is required and eminently feasible, given the availability of safe and effective treatments to control high cholesterol. Strategies can also take into account the increasing amount of evidence on how best to reorient health care provision towards the management of chronic health problems.36
FundingThe data for this analysis come from the ENRICA study, which was funded by Sanofi-Aventis. We obtained additional funding from the Fondo de Investigación Sanitaria (FIS), projects PI09-1626 and PI08-0166, and the UAM Chair in Epidemiology and Control of Cardiovascular Risk. The study was led by an independent scientific committee.
Conflicts of interestJoseph M. Taboada is employed by Sanofi-Aventis. However, Sanofi-Aventis does not currently market any cholesterol-lowering drugs.
Received 8 February 2012
Accepted 16 February 2012
Corresponding author: Departamento de Medicina Preventiva y Salud Pública, Facultad de Medicina, Universidad Autónoma de Madrid, Avda. Arzobispo Morcillo s/n, 28029 Madrid, Spain. mpilar.guallar@uam.es