Keywords
INTRODUCTION
Angiography provides excellent anatomical data on the epicardial coronary arteries, but its contribution regarding the functional significance of a given level of coronary stenosis is quite limited. However, this information is essential when the stenosis is of intermediate severity. The fractional flow reserve (FFR), as measured with a pressure-monitoring guidewire, is defined as the ratio of the peak coronary flow to the myocardium in the presence of stenosis divided by the peak coronary flow in the hypothetical absence of such stenosis.1,2 This parameter is easy-to-obtain and replicate, and some studies have shown a good correlation between this and non-invasive ischemia detection tests,3-6 establishing a 0.75 cutoff value for FFR. However, there is a gray area for FFR ranging from 0.75 to 0.80 where the results should be interpreted with caution.
The induction of maximum hyperemia is the key requirement for this technique, as in such conditions the pressure-flow relationship becomes linear.7 Microcirculatory dysfunction modifies the slope of this relationship, reducing the pressure gradient across the stenosis8 and overestimating FFR. On the other hand, if maximum hyperemia is not obtained, the gradient is also underestimated and FFR overestimated. Theoretically, diabetes mellitus entails microvascular dysfunction,9-11 which could interfere in the measurement of FFR and lead to false normal results.
This paper assesses the long-term prognosis of diabetic patients with intermediate severity coronary lesions, in whom revascularization was deferred based on an FFR 30.75.
METHODS
Patients
This was an observational retrospective cohort study that included every consecutive patient with intermediate severity coronary stenosis (40%-70% of stenosis by visual estimation under angiography) undergoing a pressure-monitoring guidewire study to calculate the FFR in a cardiac catheterization laboratory between 1997 and 2004. Patients with a recent coronary syndrome in a stable clinical condition (>4 days from onset) were included. Criteria for diabetes were diagnosed prior to cardiac catheterization. Multivessel coronary artery disease was defined as stenosis ≥ 50% in 2 or more epicardial coronary arteries. The final population in our study was 136 patients (144 lesions), as 2 coronary lesions were studied in different arteries in 6 non-diabetic patients and in 2 diabetic patients. The study met the Declaration of Helsinki criteria and was approved by the local Ethics Committee. Informed consent was obtained from all patients.
Fractional Flow Reserve Calculation
A 0.014 intracoronary pressure-monitoring guidewire was used (Radi Medical, Uppsala, Sweden, or Cardiometrics EndoSonics, Hut Cordova, California, USA). A 6 Fr guide catheter was advanced up to the ostium of target coronary artery. Fifty U/kg of intravenous heparin and 200-300 µg of intracoronary nitroglycerin were administered. The guidewire was calibrated before introducing it into the guide catheter and the guide catheter pressure matched to that of the guidewire. The distal pressure-monitoring guidewire was advanced toward to the lesion site. The FFR (ratio between average pressure obtained at the guidewire and the average pressure obtained at the catheter) was calculated after intravenous infusion of 140 µg/kg/min of adenosine over 2 min to induce maximal coronary flow. The cutoff point was set at 0.75 (negative, ≥ 0.75), based on the literature.
Quantitative Coronary Angiography
A second angiography was performed by an independent observer blind to clinical data and FFR values. This was done using validated edge-detection software (CAAS II 4.1 for Windows, Pie Medical Imaging, Maastricht, Netherlands). A calibrated guide catheter was used to calculate the reference diameter and the minimum luminal diameter, as well as the percentage of stenosis (ratio of both values). The final values were taken from the mean of 2 orthogonal projections.
Follow-up and Clinical Events
Follow-up was performed in all patients by a checkup visit in the cardiology department or, if this was not possible, by telephone. Indications for a new coronary angiography was left to the discretion of the physician in charge of the patient based on myocardial ischemia symptoms or signs. The following were considered major events at follow-up: death (considered as cardiac unless another cause could be demonstrated), myocardial infarction (thoracic pain plus increased creatine kinase levels double the laboratory's reference values), and the need for percutaneous or surgical revascularization in the lesion initially assessed using the FFR.
Statistical Analysis
The quantitative variables are expressed as mean (standard deviation). Qualitative variables are expressed as percentages. The Student t test was used to compare the means of quantitative variables with a normal distribution, and the c2 test or Fisher's exact test for qualitative variables. Combined event-free survival or death/heart attack-free survival were assessed in the 2 groups by Kaplan-Meier analysis (log-rank test). A P value less than .05 was considered statistically significant. The statistical analysis was done using SPSS for Windows software, version 12.0. (SPSS, Chicago, Ill., USA)
RESULTS
A total of 222 lesions of intermediate severity were studied in the period (206 patients); of these, the FFR was <0.75 in 72 lesions (70 patients), where revascularization was indicated. The FFR was 30.75 in 150 lesions. In 6 of these cases, the specialist recommended revascularization despite the result not being indicative of ischemia. In line with the results obtained by the pressure-monitoring guidewire, revascularization was not indicated for the remaining 144 lesions in 136 patients, which became our study population.
Comparison Between Diabetic and Non-Diabetic Patients
Table 1 summarizes the baseline characteristics of both groups of patients.
Of the diabetic patients, 17/40 (42.5%) were insulin-dependent and 23/40 (57.5%) were non-insulin-dependent (only 10% were undergoing dietary treatment). The diabetic population was older and presented a higher prevalence of cardiovascular risk factors (hypertension and dyslipidemia), as well as a higher frequency of multivessel disease. No differences were found regarding the target vessel nor in indications for coronary angiography. The lesions assessed in the cases evaluated after an acute coronary syndrome (most of which involved non-ST segment elevation) were, in general, non-causal; there was an average of 6.5 days (Table 1) between admission and the FFR study.
Quantitative angiographic data are shown in Table 2. No differences were found between diabetic and non-diabetic patients in the parameters under analysis (stenosis percentage, reference luminal diameter, minimum luminal diameter, lesion length). The average FFR values were similar in both groups.
Long-Term Follow-up
All patients underwent clinical follow-up (average, 30 [21] months). The patients who underwent major events did not initially present more severe lesions as indicated by angiography or FFR values (0.87 in both groups). There were 10 deaths and 3 acute myocardial infarctions (AMI) (Table 3). In 4 cases, death was due to non-cardiac causes (lung cancer, lung thromboembolism, digestive hemorrhage, and acute kidney failure). In the 6 remaining cases, the cause of the death was cardiac with sudden death occurring in 3 patients; no association could be established with the target artery by the FFR. Of the 3 AMI cases, 2 cases (1 in each group) were related to the target lesions. Major events (cardiac death/AMI) probably associated with the lesions initially evaluated as moderate was estimated at 3/96 (3.1%) in non-diabetic patients and 2/40 (5%) in diabetic patients (without statistical significance).
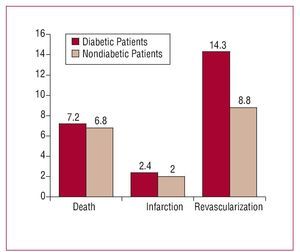
Revascularization was performed in 15 (10.4%) lesions during follow-up. Table 4 shows the main characteristics of these patients. Revascularization was indicated by clinical evidence, recurrence of angina, or positive ischemia induction tests. Disease progression was observed in two-thirds of these patients, with no differences between diabetic and non-diabetic patients. Revascularization was performed in 6/42 diabetic patients (14.3% of lesions), and in 9/102 non-diabetic patients (8.8%; P=.32) (Figure 1). Within the diabetic group, revascularization was performed in 4/18 (22.2%) of insulin-dependent patients and in 2/24 (8.3%) non-insulin-dependent patients(P=.20).
Figure 1. Major coronary events in diabetic and non-diabetic patients.
No differences were found in cardiovascular mortality (3.5% vs 5.4%; P=.23), infarction (2.3% vs 0%; P=.37), or need for revascularization (12.5% vs 7.1%; P=.30) between patients assessed after acute coronary syndromes and stable patients.
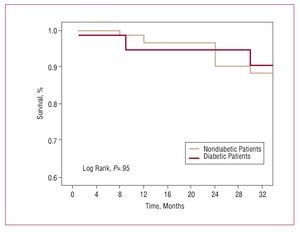
Figure 2 shows the event-free Kaplan-Meier survival curve (mortality and AMI) and Figure 3 shows the combined event-free Kaplan-Meier survival curve (death, infarction, and need for revascularization). No significant differences were found.
Figure 2. Death/infarction-free Kaplan-Meier survival curve.
Figure. 3. Death/infarction/revascularization-free Kaplan-Meier survival curve.
Safety of the Procedure
As reported by other groups,12 no major complications occurred when using this technique. There was 1 case of coronary vasospasm. Intravenous adenosine infusion had to be suspended in 2 patients due to bronchial hyperreactivity, and so this agent was administered via the intracoronary route.
DISCUSSION
One of the most frequent and difficult issues to resolve in a cardiac catheterization laboratory is to establish whether a lesion is important or not, whether it is causing ischemia, and whether it should be treated.13 In the last decade, the calculation of the FFR using an intracoronary pressure-monitoring guidewire has become a useful tool to study coronary circulation physiology in order to assess intermediate lesions.
Both retrospective14-17 and randomized18 studies have shown that deferring coronary intervention based on an FFR ≥ 0.75 is safe and does not lead to a worse prognosis for patients with stable angina. Recently, several works have found that this approach is safe in patients with acute coronary syndrome.19,20 In our study, lesions in patients undergoing an acute coronary syndrome were assessed after suitable clinical stabilization; most of these lesions were not the cause of the acute situation.
Criticism of the use of FFR focuses on the fact that it has been validated in patients with preserved ventricular function and vessel disease. In addition, the FFR value is modulated by the status of the microcirculation.7,8 Diabetes mellitus is a good example of a condition where functional and structural microcirculation abnormalities might lead to apparently normal FFR values. Furthermore, multivessel disease (with moderate lesions) after acute coronary syndrome is a frequent finding in diabetic patients.
Our work is the first to assess the strategy of deferring coronary intervention based on FFR in the diabetic population. The results indicate that this strategy appears to be safe: there was a slight but non-significant tendency for more target lesion revascularization procedures in the diabetic group (14.3% vs 8.8%) and the incidence of major events (death/AMI) associated with the target lesion during long-term follow-up was low (5% in diabetic patients vs 3.1% in non-diabetic patients; non-significant).
The direct treatment of intermediate lesions offers an alternative to this strategy. In an ad hoc analysis of 4 clinical trials. Moses et al21 reported that the treatment of stenotic lesions <50% with drug-eluting stents seemed safe: an event rate of 5.6% versus 25.4% with bare-metal stents. However, only a quarter of this population was diabetic and follow-up was just 1 year; besides this, the cost of these strategies would be far higher and the incidence of late thrombosis, although minimal, would not be well-tolerated in this population.
In the diabetic group, 2 new revascularization procedures were performed in non-insulin-dependent patients (8.3%), whereas 4 were performed in insulin-dependent patients (22.2%)—who might have greater microvascular impairment—without reaching statistical significance probably due to sample size.
In a previous study, Yanagisawa et al22 studied 304 stable coronary lesions in 96 diabetic patients and 149 non-diabetic patients assessed by FFR and pyrophosphate myocardial scintigraphy (SPECT), to determine the value of FFR in diabetics, demonstrating that a cut-off value of 0.75 was valid for detecting ischemia in this population. Glycemic control had an effect on FFR, since in those patients with poor control (glycohemoglobin >7%) the specificity of FFR was lower, probably related to inadequate arteriolar vasodilatation. This suggests that chronic hyperglycemia may have an important influence on vascular dysfunction.10
Another aspect to take into account is the presence of target-vessel infarcted territory. Previous studies23 have reported that for a similar degree of stenosis, the FFR value depends on viable myocardium. In our study, few lesions with these characteristics were included (11.7%), and only 1 patient needed revascularization during follow-up.
The agent used and the form of administration to obtain maximum vasodilatation are key factors, especially in the diabetic population where the capacity to obtain vasodilatation may be reduced. Suboptimal levels of coronary hyperemia lead to underestimating the pressure gradient. We use intravenous adenosine (140 µg/kg/min) as the standard protocol in our laboratory, which has been validated in initial studies. A recent study24 that compared 50 lesions with different hyperemic stimuli (increasing doses of intracoronary adenosine and intravenous adenosine) concluded that stimulation with intravenous adenosine at 140 µg/kg/min produces the most pronounced hyperemia and should be the method of choice for the calculation of FFR.
In 12.5% of the lesions, the use of a pressure-monitoring guidewire was compatible with intravascular sonography (mainly in lesions in the left main coronary artery and in the proximal segment of the anterior descending artery). Both techniques are complementary, and the anatomical data on the vascular wall provided by intracoronary ultrasound is highly relevant. Nevertheless, the calculation of the FFR offers the advantage of determining the level at which the stenosis restricts maximum myocardial flow and therefore the improvement rate derived from the intervention.
Limitations of the Study
Our work has important limitations. The main one is that it was a retrospective observational study, which can affect the quality of data collection. The number of cases involving diabetic patients was low, which means that this should be considered a hypothesis-generating study. There was a selection bias, since the decision to use FFR to assess lesions of intermediate severity was made at the specialist's discretion, and not all such lesions were assessed in the given period. This means that the conclusions should not be extrapolated to all intermediate severity lesions in diabetic patients, but rather only to those assessed (basically, focal lesions, and proximal segments). Data on glycemic control are not available which may have affected the results of FFR. Coronary flow reserve as assessed by Doppler guidewire for the detection of microvascular disease was not studied.
CONCLUSIONS
Our results indicate that deferring coronary intervention in diabetic patients with intermediate coronary stenosis and FFR 30.75 seems to be a safe strategy.
ABBREVIATIONS
AMI: acute myocardial infarction
DM: diabetes mellitus
FFR: fractional flow reserve
SEE EDITORIAL ON PAGES 343-5
Dr Domínguez-Franco has a support contract in Postgraduate Specialist Health Care research from the Instituto de Salud Carlos III (Carlos III Health Care Institute), 2005.
Correspondence:
Dr. A.J. Domínguez Franco.
Campus de Teatinos, s/n. 29010 Málaga. España.
E-mail: antoniodominguez@secardiologia.es
Received July 4, 2007.
Accepted for publication December 18, 2007.