Tobacco use is the principle cause of cardiovascular disease (CVD). It puts at risk both the health of smokers and that of passive smokers. Epidemiologic evidence of the relation between tobacco and coronary disease was first published in 1940.1 The Minnesota Business Men and Framingham studies showed the relation between tobacco and mortality.2 Hence, today, the epidemiologic evidence is clearly unquestionable.
Coronary risk increases markedly even with low levels of exposure,3 which explains why one or two cigarettes a day doubles cardiovascular risk4 and environmental tobacco smoke causes CVD in passive smokers.5
RELATION BETWEEN PASSIVE SMOKING AND CARDIOVASCULAR DISEASEThe negative effect of passive smoking was first studied in respiratory disease in children.6 In 1986, the International Agency for Research on Cancer, US Surgeon General, and US National Research Council established the relation between passive smoking and lung cancer.7 Meta-analyses published in the 1990s showed a 20% increase in coronary disease and cardiovascular death in passive smokers.8,9 In 2006, the Surgeon General's Report established that any exposure to second-hand smoke is prejudicial. The relative risk of coronary disease for active smokers is 1.78 and for passive smokers, 1.3. One passive smoker's death is recorded for every 10 active smokers’ deaths.10 Passive exposure to tobacco smoke in the home also increases the risk of CVD. Ischemic heart disease is the principle cause of death among passive smokers—far ahead of lung cancer11 —and its effect is rapid: the risk of acute coronary syndrome (ACS) increases within a few minutes of inhaling tobacco smoke.
PHYSIOPATHOLOGY OF CARDIOVASCULAR DAMAGE FROM TOBACCO IN SMOKERS AND NONSMOKERS EXPOSED TO ENVIRONMENTAL TOBACCO SMOKELipid Profile AbnormalitiesNicotine produces sympathetic stimulation that increases free fatty acids. This translates into elevated low-density lipoprotein levels and declining high-density lipoprotein levels. Moreover, tobacco increases insulin resistance, which is associated with low concentrations of high-density lipoproteins and small, dense, low-density lipoproteins, which are more atherogenic. Smoke reduces paraoxonase activity, which protects low-density lipoproteins from oxidation. The lipid profile gradually returns to baseline level upon giving up smoking.12
Inflammation, Thrombosis, Endothelial Dysfunction, and AtherosclerosisTobacco smoke has a pro-inflammatory, oxidative, thrombotic effect, which induces atherosclerosis and maximizes other cardiovascular risk factors. Smokers, both active and passive, have 20% to 25% more leukocytes in blood. These liberate elastase and oxidizing free radicals, which in turn harm the endothelial wall and favor atherosclerosis.13 Tobacco smoke activates platelets, increasing the proliferation of smooth muscle cells, fibrinogen, factor VIII, tPA and platelet-dependent thrombin, and reducing plasminogen.
Nicotine and tobacco smoke damage endothelial cells, increase free radicals that deactivate vasodilatatory substances and increase the risk of vasospastic angina.14 Increased sympathetic activity reduces the threshold for ventricular arrhythmias, whereas greater heart rate and blood pressure increase the need for myocardial oxygen and added carboxyhemoglobin impedes the oxygen supply.
Dose-response Relation and its Effect on Passive SmokersAll these changes accelerate the progress of atherosclerosis and predispose to coronary spasm and thrombosis, and therefore ACS, even at low levels of exposure such as that affecting passive smokers.
BENEFITS TO CARDIOVASCULAR RISK OF SMOKING CESSATION OR NOT INHALING SECOND-HAND SMOKEGiving up smoking is the most important measure in primary or secondary prevention of CVD. It is associated with a rapid reduction in ACS risk and the progression of coronary disease, cerebrovascular disease, and peripheral vascular disease.15 Cohort studies and meta-analyses have shown that giving up smoking reduces mortality.16 The risk of atherosclerosis associated with tobacco declines at 2 years after cessation; but the reduction in risk of ACS occurs within a few hours.17
MEASURES TO AVOID THE DAMAGE PRODUCED BY TOBACCO: LEGISLATION RESTRICTING SMOKING IN PUBLIC PLACES AROUND THE WORLDThe damage caused by tobacco smoke can only be avoided in 2 ways: having smokers give up smoking and protecting nonsmokers from exposure to environmental tobacco smoke. Exposure in the home and workplace are the most important. In 2007, the World Health Organization's Framework Convention on Tobacco Control set the ground rules for protecting nonsmokers’ health.18,19 Although various countries (among them Spain) have ratified this convention, it has barely been put into practice. Given that standard ventilation systems cannot eliminate the toxic components of tobacco smoke, the only effective way of avoiding the risk of passive smoking is to ban tobacco use in closed spaces. It is very difficult to regulate air quality in the home and the only way to control passive smoking in this context is through education and helping smokers give up the habit. In the workplace and elsewhere in public, legislation does effectively restrict tobacco use, so as to protect the health of nonsmokers faced with a risk they have not chosen to face. Moreover, the laws favor a change in the deceptive perception that smoking is a social habit and clearly establish it as an addiction with severe consequences for smokers and those who live with them.
IMPACT OF LEGISLATION ON CARDIOVASCULAR DISEASE IN THE WORLDBy its very nature, smoking is not susceptible to randomized study. The evidence available is based on observational studies comparing incidence trends before and after the laws came into effect. In the United States, California was the first state to legislate on tobacco use in the workplace, including restaurants and bars, in 1988. In Europe, it was not until 2004 that smoking in public places was first legally banned in Ireland; Norway, the United Kingdom, Italy, Spain, and France followed suit. The legislation cut exposure to tobacco smoke and, consequently, incidence of ACS -above all, in nonsmokers.20 Moreover, some studies show a 3.8% fall in the number of smokers at 1 year, although this could be explained by other causes, like the increase in the cost of tobacco.
In Ireland, one year after the law came into force,21 the rate of ACS had fallen by 12%. In Italy,22 in the 6 months after the anti-smoking law came into effect the incidence of ACS had fallen by 6%. In Scotland,23 it had fallen by 17%, essentially among nonsmokers.
Meta-analyses report 16% to 17% reductions in admissions for ACS in the first year. Hospital costs have fallen in parallel. The more restrictive the law, the greater its impact.24
MEASURES TO AVOID HARM CAUSED BY TOBACCO: LEGISLATION RESTRICTING SMOKING IN PUBLIC PLACES IN SPAINIn Spain, legislation on tobacco use in public places was introduced with Law 28/2005 on Health Care Measures to deal with Smoking and Regulate the Sale, Supply, Consumption and Advertising of Tobacco Products. Although its approval meant a major advance in public health policy, it included exceptions, permitted smoking in bars and restaurants as a function of their surface area, and allowed for designated smoking areas. What was needed was a norm with no exceptions, which would ban smoking in closed public spaces to protect bar and restaurant industry workers and passive smokers in general. Law 42/2010 (30 December 2010) came into effect on 2 January 2011 and modified the former law, extending the smoking ban to any closed space used by the general public. It also banned smoking in some open spaces within education centers, health care centers, and areas bordering on children's playgrounds. The designated smoking areas in closed spaces at airports were eliminated. The new law turned Spain into a role model to be followed on issues of smoking control policy, and has been widely accepted and respected by most of the population.
STUDIES TO DETERMINE THE IMPACT OF THE 2005 LAW ON INCIDENCE OF ACUTE CORONARY SYNDROME IN SPAINIn Barcelona, in the year after the 2005 Law came into force, hospital admissions for ACS fell by 11% in men and 9% in women.25 Moreover, the law contributed to ±5% fall in the prevalence of smoking and a reduction in the number of cigarettes smoked by those who continued to smoke.26 Other factors, such as the increased cost of tobacco, probably contributed as well. The law passed to protect the health of passive smokers brought smokers a secondary benefit as it promoted a change of attitude towards smoking.
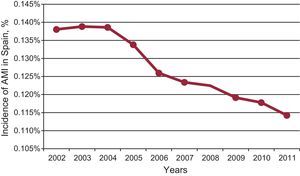
STUDIES TO DETERMINE THE IMPACT OF THE 2005 AND 2010 LAWS ON INCIDENCE OF ACUTE CORONARY SYNDROME IN SPAINTo determine the changes in hospital admissions for ACS in Spain after the 2005 and 2010 laws came into effect, data on number of admissions were collected from Spanish National Institute for Statistics publications, and on associated costs from some regional government publications for 2002 to 2012. Moreover, data on number of admissions for ACS were collected locally at selected hospitals in various autonomous regions. When the first law came into force in 2006, incidence of acute myocardial infarction fell by 4.2% (95% confidence interval [95%CI], 3%-5.4%); when the second law came into effect in 2011, it fell by 3.1% (95%CI, 1.9%-4.3%). Similarly, in 2006 the incidence of ACS, including acute myocardial infarction and unstable angina, fell by 6.9% (95%CI, 5.8%-8.1%); in 2011, it fell by 5% (95%CI, 3.8%-6.1%). The data obtained locally give similar results, although they vary considerably between centers and confidence interval ranges are wider. While it cannot be proven that the fall in incidence is exclusively due to the anti-smoking laws, it is quite remarkable that the sharpest fall should occur in 2006, with a further fall in 2011 (Figure). These data concur with figures on cigarette sales in Spain, although sadly we do not have data on nicotine in nonsmokers (in contrast to the data for Scotland); hence, reduced cigarette sales are an indirect measure of this beneficial effect. If we consider the financial savings on hospital admissions derived from the reduced incidence of acute myocardial infarction in nonsmokers, the law of 2005 saved €23.3 million and the second law, in 2011, saved a further €13.6 million.
THE FUTURE OF ANTI-TOBACCO LEGISLATIONLegislating to restrict tobacco use in public places and raising taxes on tobacco are efficient strategies to reduce the damage tobacco causes. Other initiatives are also useful. In July 2013, the European parliament's public health committee passed a resolution—by 50 votes for, 13 against, and 8 abstentions—to toughen legislation to dissuade young people from starting to smoke by banning the use of flavorings like strawberry and menthol in tobacco products, increasing the size of health warnings on all sides of cigarette packs, and banning slim cigarettes and attractive packaging. The objective is to prevent the tobacco industry from recruiting new smokers among the young. The European Society of Cardiology (ESC) has supported the European Commission's initiatives and stresses that, aside from writing laws that ban smoking in public places, the regulation of tobacco derivatives is crucial to ensure citizens perceive that smoking puts their health at risk. Cardiovascular disease causes 1.9 million deaths per year in the European Union and of these, 41% are due to tobacco. In total it is estimated that patients with CVD cost the EU €195.5 billion per year. The Spanish Society of Cardiology backs the ESC and supports its initiatives against the major public health problem facing Europe: tobacco.
CONCLUSIONSThe ban on smoking in public places protects the population from passive exposure to smoke, mainly reducing the risk of tobacco for passive smokers and, specifically, cutting the incidence of ACS and its cost. It probably also reduces risk for active smokers, with the consequent reduction in the number of smokers and the mean number of cigarettes smoked per smoker. In Spain, over a period of 5 years, 2 laws have been passed that restrict tobacco use in public places; the second—and more restrictive— has enhanced the efficacy of the first.
CONFLICTS OF INTERESTThe first author directs a project studying the relation between legislation banning smoking in public places and CVD, which is financed by an unconditional grant from Pfizer.
Jaime Fernández de Bobadilla (Servicio de Cardiología, Hospital La Paz, Madrid), Regina Dalmau (Servicio de Cardiología, Hospital La Paz, Madrid), Enrique Galve (Servicio de Cardiología, Hospital Vall d’Hebron, Barcelona), Ramón Bover (Servicio de Cardiología, Hospital Clínico San Carlos, Madrid), Carlos Ávarez (Servicio de Cardiología, Hospital La Paz, Madrid), Alberto Cordero (Hospital de San Juan, Alicante), Leticia Fernández (Servicio de Cardiología, Hospital Costa del Sol, Marbella, Málaga), Juana Freire (Servicio de Cardiología, Hospital Arquitecto Marcide, Ferrol, A Coruña), Juana Umarán (Servicio de Cardiología, Hospital Galdakao Usansolo, Bizkaia), Francisco Roncales (Servicio de Cardiología, Hospital Clínico Universitario Lozano Blesa, Zaragoza), Susana del Prado (Servicio de Cardiología, Hospital La Paz, Madrid), Xavier Garcia-Moll (Servicio de Cardiología, Hospital de la Santa Creu i Sant Pau, Barcelona), and Esteban López de Sá (Servicio de Cardiología, Hospital La Paz, Madrid).