To the Editor:
Inappropriate sinus tachycardia or non paroxysmal tachycardia is characterised by persistent cardiac arrhythmias, with sinus P waves, and an exaggerated response to a minimal physical effort. It usually appears in young women and manifests through palpitations, dyspnoea, fatigue, and intolerance to exercise. After excluding other types of tachycardia and discarding secondary symptoms of other affectations, the reproduction of symptoms during an episode of tachycardia allowed for confirmation of the diagnosis. Beta-blockers and calcium channel blockers are the most frequently used medications for treating symptomatic patients and in general are not tolerated well at the doses required for the control of tachycardia. Invasive treatment with selective or complete catheter ablation of the sinoatrial node is not exempt from complications and on occasions requires the implantation of a permanent pacemaker. Ivabradine is a selective inhibitor of the I channels that has recently been approved for the treatment of stable angina pectoris. It is considered an attractive alternative for heart rate control in inappropriate sinus tachycardia.1
We shall present the case of a 29-year-old woman with a history of smoking and a difficult twin labour 2 years earlier. Over the preceding months and almost on a daily basis, she had been experiencing frequent episodes of general asthenia with palpitations, nausea and a suffocating sensation. One of theses episodes included atypical chest pain and signs of presyncope, for which she was attended to in the emergency service of a nearby hospital. The physical examination and the diagnostic tests revealed no significant alterations, except for the sinus tachycardia at 105 beats/min and borderline low blood pressure of 90/60 mm Hg. After being kept under observation, she was assessed in the chest pain unit with echocardiography, chest x-ray and thyroid hormone and catecholamine analysis, all of which were normal. During the exercise stress test, she surpassed 85% of the MHR in the first stage of the Bruce Protocol Test and finally reached 97% of the MHR and 11 MET, with no data indicating myocardial ischaemia. On discharge, she was diagnosed with an anxiety disorder and was prescribed treatment with sedatives, which did not improve the symptoms. She was referred to a local psychiatrist, who found no illness and discarded anxiety as a cause of the symptoms. New diagnoses were contemplated in the internal medicine unit, but these were discarded after analytical study, pulmonary perfusion scintigraphy, computerised chest tomography, and gastroscopy. She was then referred to the cardiology department to complete the study.
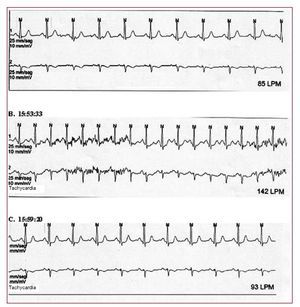
On arrival at our consultation, the symptoms had progressed and episodes of weakness and palpitations manifested several times throughout the day, which would greatly interfere in her working life and in the care of her children. The physical examination presented no alterations with a body mass index of 17 and blood pressure of 100/70 mm Hg. The ECG showed a sinus tachycardia of 100 beats/min and unspecified repolarisation changes, with increases in heart rate up to 145 beats/min, both on assuming a standing position and on minimal efforts, reproducing, although in a less intense manner, the symptoms for which she was being analysed. The 24 h Holter monitor indicated frequent episodes of progressive start and finish sinus tachycardia with a maximum rate of 142 beats/min and 10 minute duration, moments in which the patient pressed the event button, which allowed the discarding of other types of tachycardia (Figures 1 and 2). Low dose treatment with propranolol was then introduced, which she did not tolerate well due to her tendency towards hypotension. Substitution of propranolol with ivabradine2 was considered in this situation. Despite the fact that its use had been approved only for treatment of stable angina, its mechanism would infer an eventual benefit in the patient's disorder. The patient accepted the treatment, which was started with a dose of 10 mg/day and later increased to 15 mg/day. This last treatment managed to finally control the patient's symptoms, which she tolerated well at a resting heart rate of 63 beats/min and showed no side effects; allowing her to resume her working routine and the care of her children without limitations. An improvement of 47 points in the quality of life evaluation was noted according to the MLWHF questionnaire. In the first 3 months, only 2 episodes of palpitations have occurred, coinciding with a fever and with the use of nasal decongestants, respectively. A new ergometry was performed: clinically negative, without surpassing 80% of the MHR and with a functional capacity of 13.7 MET.
Figure 1. Heart rate Holter: sinus tachycardia at 142 beats/min with progressive start and end. The patient pressed the event button at the start of the tachycardia for clinical reference of palpitations and general weakness; at that moment she was seated chatting with a friend, which discards a stressful situation or the performing of a physical exercise.
Figure 2. Heart rate Holter: traces in sinus rate before (A) and after (C) the appearance of the tachycardia, as well as its record (B).
To conclude, Ivabradine could represent an efficient alternative to beta blockers in the treatment of inappropriate sinus tachycardia prior to invasive studies. Prospective and random studies allow for an evaluation of its long term efficiency and safety.