AVNodal reentrant tachycardia is probably the most frequent supraventricular tachycardia, after fibrillation and atrial flutter, and the most commonly treated by catheter ablation. In fact, the ablation of this arrhythmic substrate currently represents around a third of all such procedures in Spain.1-3
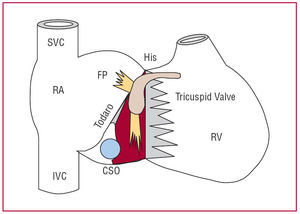
The mechanism of this arrhythmia, although not completely understood, has been fairly well characterized.4,5 Thus, today it is accepted that the atrioventricular node is a more extensive structure than previously believed -- located in the triangle of Koch -- and, from the functional point of view, consists of at least two connections to the surrounding atrial myocardium (Figure).6 The first, in a more cranial position, is known as the fast AV nodal pathway; this has a fast conduction velocity and prolonged refractory period leading, at slow atrial rates, to the heart's electrical impulse being conducted in a very short time, whereas at fast rates it cannot pass through this structure. The second connection is known as the slow AV nodal pathway and has a more caudal location. It presents slow conduction velocities and a short refractory period. This leads, at fast atrial rates and when there is no conduction through the fast AV nodal pathway, to the electrical impulse being conducted over it with longer time to reach the ventricles. This occurs despite the fact that a prolonged PR interval due to circulating catecholamines is often not found, though these are normally present in situations associated with high atrial rates. In the electrophysiology laboratory, it is possible to show the well-differentiated presence of these two pathways in some individuals by the incremental introduction of atrial extrastimuli, progressively slightly earlier, until conduction through the fast AV nodal pathway is blocked, which appears as a sharp and significant increase (>50 ms) in the atrio-His bundle conduction interval (AH interval). This situation is known as dual AV nodal physiology and the instant of the significant increase as AH jump. These differentiated characteristics of the two AV nodal pathways also lead, as a consequence of an atrial extrasystole with a short coupling interval, to the electric impulse encountering the fast AV nodal pathway in its refractory period with very slow conduction via the slow AV nodal pathway. Slow conduction via the latter pathway means, in turn, that the fast AV nodal pathway has time to recover its conduction capacity when the impulse reaches the distal end of the slow AV nodal pathway at its common insertion point with the fast AV nodal pathway at the bundle of His. In this situation, in addition to being conducted anterogradely through the bundle of His toward the ventricles, the impulse will be conducted retrogradely through the fast AV nodal pathway toward the atria, from where it can reenter the slow AV nodal pathway, repeat this sequence and give rise to the common form of AV nodal reentrant tachycardia (AVNRT). This sequence can also occur in the opposite direction, usually triggered by ventricular extrasystole, giving rise to the uncommon form or the fast-slow AVNRT, approximately 10 times less frequent than the previous type. A controversial aspect regarding these tachycardias is the term "nodal reentry," which indicates that reentry is confined to the AV node and that there would be intervening nodal tissue both between the arrhythmic circuit and atria, on the one hand, and between the circuit and the bundle of His, on the other.7 This could be why AVNRT presents different AV conduction relations due to potential conduction block, by blocking conduction toward the atria (upper common pathway) or by conduction block toward the bundle of His (lower common pathway). However, almost all authors reject the existence of the upper and lower common pathways in most patients with common AVNRT at present time.8
Figure 1. Anatomical diagram in right oblique anterior projection of the right cardiac chambers and atrial node in the triangle of Koch with its 2 connections to the atrial myocardium, the fast AV nodal pathway (FP) and the slow AV nodal pathway (SP). RA indicates right atrium; CSO, ostium of the coronary sinus; Todaro, tendon of Todaro; IVC, inferior vena cava; SVC, superior vena cava; RV, right ventricle.
Ablation of AVNRT was described in 1989.9,10 The fast AV nodal pathway was initially targeted, but this frequently resulted in prolongation of the baseline PR interval and in a non-negligible incidence of complete iatrogenic complete AV block. PR interval prolongation could be so exaggerated that some patients developed a syndrome similar to pacemaker syndrome.11 Subsequently, slow AV nodal pathway ablation was targeted, but no significant prolongation of the PR interval was found and there was a very low incidence of complete AV block.12,13 Although this procedure was initially aimed at ablation, it was later seen that instead of complete suppression of conduction, significant modification or modulation of its conduction properties was sufficient for tachycardia sustainment supression except for a single AV nodal echo beat and for the patient not to present recurrence. At present, this procedure to supress recurrence at follow-up is successfully done in more than 98% of such patients with a complication rate barely reaching 1.2%.3 Thus, the clinical practice guidelines of the American Heart Association, American College of Cardiology, and European Society of Cardiology14 consider ablation of nodal reentrant AVNRT as a class I indication, at the same level as beta blockers or calcium-channel antagonists, and which should be offered from the beginning as an alternative to these even in elderly patients, in whom excellent results have also been obtained using this technique.15
However, and despite current knowledge about the pathophysiological mechanism and the good results of catheter ablation, one of the problems frequently seen in the electrophysiology laboratory is that it is not possible to the induce tachycardia, despite the use of various electrical stimulation protocols or infusion of drugs such as isoproterenol. When electrocardiographic documentation is available on a tachycardia which suggests AVNRT and, in addition, there are indirect data on this mechanism, such as electrophysiological demonstration of dual AV nodal physiology, the empirical ablation of the slow AV nodal pathway has been proposed, with complete elimination of its conduction.16,17 However, this approach has some problems. First, it requires the complete elimination of the slow AV nodal pathway, involving a more aggressive procedure and, thus, greater potential risk of complications. Although the authors of these studies did not find a higher rate of complications than with the conventional approach, it should be emphasized that these two series included a limited number of patients (7 and 27 patients) and that their results have not been confirmed by other studies.18 Second, an electrocardiographic recording during an episode of palpitations is not always available. Hence, although the symptoms of the patient may suggest AVNRT, the decision to carry out ablation of the slow AV nodal pathway
-- and to assume its low but existent risk of complications -- should be taken only based on the objective data of not having demonstrated any other mechanisms of tachycardia and the presence of dual AV nodal physiology, which is present in up to 20% of the population.19 Finally, it is sometimes impossible to demonstrate dual nodal physiology, even though the patient has documented tachycardias, which means that, on the one hand, there is uncertainty regarding its mechanism and, on the other, it is not possible to guide the ablation procedure by eliminating the dual nodal physiology.
In this issue of the Journal, Martínez-Sánchez et al20 assess the potential usefulness of incremental atrial pacing for evaluating the effect of radiofrequency ablation on AVNRT. The authors find a relatively high sensitivity and specificity of a PR interval shorter than the RR interval during incremental atrial pacing as a predictor of eliminating nodal reentrant tachycardia AVNRT supression. This work has been suitably designed and implemented, but is not original given that, as the authors mention, Baker et al21 published a similar study 10 years ago. However, its interest lies in the fact that it includes almost three times the number of patients and, more importantly, it provides additional information about this predictor using a softer ablation criterion of nodal tachycardia (AVNRT ablation through complete ablation or modulation of the slow AV nodal pathway) and is more in line with normal clinical practice than the criterion used in the study by Baker et al21 (ablation of the slow AV nodal pathway). This criterion could be useful in those patients in whom it is not possible to demonstrate dual AV nodal physiology or to induce tachycardia, given that the positivity of this criterion was less than 7% in the patients with these characteristics free from AVNRT. Nevertheless, the real usefulness of this criterion in this population is uncertain, given that patients with spontaneous tachycardia in whom it was impossible to induce tachycardia were excluded from this study. The latter does not decrease the value of this predictor. In our opinion, it should be systematically implemented in the ablation protocol for the patient with suspected AVNRT, due to its quick and easy use.
See article on pages 32-7
Dr José L. Merino works with 3M Farmacéutica, Sanofi-Aventis, St Jude Medical, Boston Scientific, and Medtronic Iberica, in continuous training activities and as a scientific evaluator, and researcher.
Correspondence: Dr. J.L. Merino.
Unidad de Arritmias y Electrofisiología Cardiaca (planta 10).
Hospital General La Paz.
Paseo de la Castellana, 261. 28046 Madrid. España.
E-mail: jlmerino@secardiologia.es