Cardiac resynchronization therapy (CRT) has been demonstrated as being an extraordinarily effective technique that improves symptoms leading to reverse ventricular remodeling and reducing mortality in patients with a wide QRS complex and advanced heart failure.1-3 However, only a minority of possible candidates currently receive this treatment. As far as we know, there are 2 basic reasons for this: first, it continues to be applied too late and as palliative therapy in patients with very advanced, or almost terminal, disease; second, there are serious technical limitations that make the application of CRT difficult.
Selection Criteria for CRT
The growing adherence to treatment guidelines and evidence-based medicine has had many positive effects. However, there have also been less positive effects, which include the selection criteria for CRT being applied too strictly. The selection of patients for inclusion in multicenter studies is based on 2 very subjective criteria: being in functional class III or IV, and receiving optimal medical therapy.4 However, the assessment of functional class is clearly imprecise and often open to interpretation. What can be made, for example, of a patient with dilated cardiomyopathy and left bundle branch block admitted in class III and changing to class II after increasing the doses of diuretics? According to the guidelines, this patient does not fulfill criteria for CRT and thus CRT is delayed until it is too late. The SCAR study, conducted in Spain with CRT patients, showed that a very dilated left ventricle (end-diastolic diameter >75 mm) and severe mitral valve failure are predictors of nonresponse to CRT, that is, they indicate advanced disease.5,6 Recent data from the REVERSE7 study show that CRT leads to significant remodeling when it is applied to patients in class II. Other studies have shown, for example, that patients with extensive posterolateral scar tissue are less likely to respond to therapy.8,9 Other candidates for CRT who are not considered in some guidelines are patients with atrial fibrillation, whereas several observational studies, such as the SPARE study conducted in Spain,10-12 have shown that patients with atrial fibrillation also benefit from CRT whenever the heart rate is suitably controlled. Thus, it seems clear at this point that it is important to prescribe CRT in less advanced stages of the disease in patients with left bundle branch block.
Cardiac imaging techniques are indisputably useful to evaluate cardiac dimensions and function, and are thus indispensable in assessing patients with heart failure and, specifically, in assessing possible candidates for CRT. Their potential usefulness in the assessment of mechanical dyssynchrony is more controversial and debated, especially in view of the expected results of the PROSPECT study.13,14 Although the concept of being able to assess mechanical dyssynchrony using a noninvasive imaging technique is obviously appealing, current technology and knowledge do not allow us to do this with sufficient accuracy. On the other hand, the detection of mechanical dyssynchrony does not guarantee that it can be corrected using CRT.
Technical Difficulties Involved in Implantation
In addition to poor patient selection, either due to late indication or too extensive necrosis, the lack of efficacy of CRT has been attributed to the incorrect implantation of the lead in the left ventricle. It is evident to the physicians who implant CRT devices that the technique involves serious multifactorial challenges that limit its applicability. First, such physicians have to learn unusual techniques, such as venous angiography, selective catheterization of vascular branches, the manipulation of angioplasty guidewires, etc.15 The fact that in most centers the number of devices implanted per year is low means that the learning curve is excessively prolonged, which often leads to failure and frustration due to a poor approach to training.
The available tools are still limited and the success of implantation fully depends on the type of materials used, regarding which there is still great room for technical improvement. Furthermore, it depends to a great extent on the materials provided by manufacturers. It should be possible to use materials from different manufacturers to obtain better performance.
Another very important aspect is related to the equipment normally used in Spain when implanting these devices. Despite the technical difficulties inherent to implantation, the radiology devices and the electrophysiology laboratories or operating rooms are not of sufficient quality to obtain good images. The monitoring of patients who are often in a hemodynamically unstable condition is clearly inadequate, as well as the provision of personnel.
The present issue of the Revista Española de Cardiología includes an article by Arbelo et al,16 an especially active group regarding implanting CRT devices and that usually use the standard equipment found in a cardiac catheterization laboratory. This, combined with this group's experience of implantation, explains the excellent results reported, with an efficacy of 98% using the transvenous route, and that are well above other published results indicating failure rates of around 10%.17
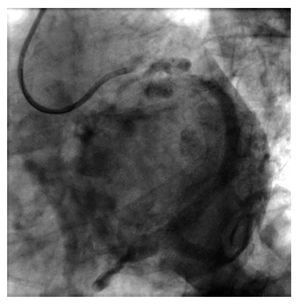
The present study investigates the efficacy of analyzing the venous phase of coronary angiography in order to study the venous anatomy before implantation. The study concludes that in most patients a good image can be obtained of the venous anatomy of the left lateral region. The study raises an unresolved issue in the context of device implantation. To what extent does previous knowledge of the venous anatomy facilitate device implantation? A randomized study which, in addition to analyzing the results, could analyze the costs of adding imaging techniques to the implantation process would probably be needed to answer this question. The advantage of analyzing the venous anatomy during coronary angiography is that it does not add costs. The disadvantage is that coronary angiography is often performed well before implantation takes place, even in other centers, which means that many patients should undergo a new coronary angiography during admission to the center performing the implantation in order to visualize the venous phase of coronary angiography (Figure 1).
Figure 1. Venous phase of left coronary angiography. The image shows the existence of patent posterolateral veins suitable for implanting the lead in the left ventricle.
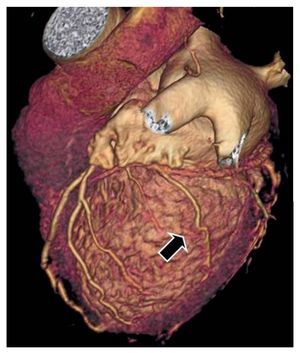
Currently, there is another technique that enables visualizing the coronary venous tree in great detail, ie, high resolution computerized tomography (HRCT) (Figure 2). The images obtained using HRCT make it possible to reliably see if there are suitable veins available for implanting the lead and to appropriately plan the implantation.18
Figure 2. Multislice computerized tomography showing the coronary venous tree. A lateral vein is shown which is suitable for implanting the left lead (arrow).
Even though no randomized studies have shown whether previous knowledge of the anatomy increases implantation efficacy, it is certain that any physician involved in this technique would prefer to know this information beforehand, if it could be easily and effectively obtained. It has become increasingly evident that positioning a lead, or even more than one lead, in the segments with the latest contraction19,20 can improve response, as recently reported by Leclerq et al.21 Therefore, preparing the patient by choosing the vein before implantation will possibly become of increasing importance in daily practice. Thus, regardless of the technique used, it is almost certainly worth knowing the venous anatomy prior to implantation. The fact that this is still not a compulsory requirement is due to organizational difficulties in obtaining, for example, the venous phase of coronary angiography or HRCT of all patients who should undergo implantation.
In conclusion, despite the efficacy of CRT, its application in daily practice is far from being ideal. The technique should be indicated much earlier. The laboratories where these devices are implanted should be better equipped and, finally, it would be advantageous to know the venous anatomy previous to implantation to better prepare for the intervention.
SEE ARTICLE ON PAGEs936-44
Correspondence:
Dr. L. Mont.
Servicio de Cardiología. Hospital Clínic.
Villarroel, 170. 08036 Barcelona. España.