Resistant hypertension, also known as refractory hypertension in the literature, is a relatively common disease that is associated with elevated cardiovascular and renal risk.1 Clinical trials suggest that its prevalence is around 35% in hypertensive patients with a baseline blood pressure (BP) > 160/100mmHg. However, data obtained from registries or from the physician's office suggest that its prevalence is around 12%.2 The recent National Health and Nutrition Examination Survey suggests a similar prevalence of 12.3% in diagnosed and treated hypertensive patients.3 An incidence study conducted at Kaiser Permanente Colorado and Kaiser Permanente Northern California4 followed up more than 200 000 hypertensive patients who started antihypertensive therapy. Of these, 0.7/100 patients/year developed resistance to treatment. Furthermore, this study showed that the risk of cardiovascular events was 47% higher in the resistant patients than in the other patients during a mean follow-up of more than 3 years.
Although its definition has undergone changes in the last 30 years, currently the concept applies to patients undergoing antihypertensive treatment with a combination of 3 or more antihypertensive agents at optimal doses, 1 of which must be a diuretic, with BP remaining above the goal of ≥ 140 mmHg and/or ≥ 90 mmHg.1 A new definition of resistant hypertension refers to patients who require treatment with 4 or more drugs to achieve BP control.1 This definition is based on epidemiological studies, but is of little clinical use.
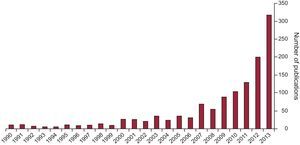
Regardless of its prevalence and definitions, the recent interest in this condition in the medical literature is striking, given that patients with drug-resistant hypertension have always been seen in hypertension units. There has been an increase in the number of publications in PubMed in which the descriptors “resistant hypertension” or “refractory hypertension” appear in the title or abstract (Figure). From an average of 10 articles published per year up to 2008, the number grew to 200 articles published in 2012, and reached a total of 325 articles published in 2013 (as of November 15). The reason for this sudden interest is doubtless associated with the introduction of new procedures for the control of hypertension in these patients, involving nonpharmacological intervention techniques applied to the adrenergic nervous system, renal denervation,5 and baroreflex stimulation.6 Alongside publications indicating the efficacy and safety of these procedures and describing advances in their development and improvement, the characteristics of these patients has also become a topic of interest. In this setting, the current edition of Revista Española de Cardiología has published an article by Gijón-Conde et al,7 who used electronic health records to analyze the demographic and clinical characteristics of resistant hypertension in a large sample of primary care patients in Area 6 in Madrid. Based on these records, prevalence was 9.2% of the whole sample and 12.8% of the treated patients. A total of 6292 patients with “refractory hypertension” were compared to the other diagnosed hypertensive patients in the database (n = 42 452). Caution should be taken regarding both the data and their possible extrapolation to resistant hypertension because the estimate was based on electronic records, which have many limitations regarding their use in clinical and epidemiological studies. In addition, aspects currently accepted as needed for the correct estimation of “true” resistant hypertension were not considered.
In the field of resistant hypertension, efforts should focus on ways to best identify truly resistant hypertensive patients, end-organ damage, and potential causal mechanisms of resistance. This would improve assessment and lead to a better therapeutic approach using pharmacological and nonpharmacological measures, including those recently introduced for treating the sympathetic nervous system.5,6
The initial diagnostic approach should exclude pseudoresistant patients, whereas it should specifically include out-of-office BP measurement, whether home BP monitoring or ambulatory 24-h BP monitoring,8 which is readily available in Spain in many primary care settings or by referring patients to hospital services. Various studies have shown that the implementation of these out-of-office measures reduces the prevalence of observed refractory hypertension by approximately 30%. According to different guidelines, these measures are now mandatory when assessing these patients on antihypertensive treatment. Furthermore, 24-h ambulatory BP monitoring not only reduces prevalence and provides added prognostic value, but should also be used to assess the therapeutic response.9
Along with out-of-office BP monitoring, the diagnostic approach should also exclude patients who are nonadherent to nonpharmacological and pharmacological measures. Nonadherence is the leading cause of pseudoresistance10 and is the most difficult cause to exclude in clinical practice.11 An estimated 30% of patients are nonadherent to treatment, defined as the failure to take medication or the failure to take medication at the scheduled times. Excessive intake of salt12 or alcohol13 and obesity14 also contribute to maintaining high BP, as well as the use of widely used drugs that raise BP, such as non-steroidal anti-inflammatory drugs, corticosteroids, and nasal vasoconstrictors.
Secondary hypertension should also be excluded when assessing resistant hypertensive patients. Although a variety of causes may underlie this condition, primary aldosteronism and severe sleep apnea syndrome are the most common. A recent study showed that primary aldosteronism was present in about 10% of resistant hypertensive patients.15 A very systematic search for signs and symptoms is required to identify primary aldosteronism because most patients will not present the standard signs, such as hypokalemia. Severe sleep apnea syndrome should also be excluded, because its treatment can control BP.16
The assessment of end-organ damage, left ventricular hypertrophy, and urinary albumin excretion and the improved measurement of cardiovascular and/or renal risk provide a reference point to assess the effectiveness of treatments.17 The reduction of ventricular hypertrophy and the persistent reduction of microalbuminuria are considered markers of reduced cardiovascular and/or renal risk.
After excluding these situations and establishing that the patient has true resistant hypertension, the mechanisms maintaining high BP have to be identified. There are 3 main mechanisms: structural arterial abnormalities (remodeling and vascular hypertrophy of the small vessels and/or loss of large vessel vascular elasticity), central hypervolemia, and sympathetic hyperactivity. These mechanisms may be present to varying degrees and 2 or more may be present at the same time in resistant hypertensive patients. Of the 3 mechanisms mentioned, vascular damage is the least susceptible to specific treatment. Vascular damage is usually found in elderly patients with chronic hypertension without regular treatment, with evidence of severe arteriosclerosis, very high BP values, and high pulse wave velocity. Central hypervolemia may be suspected in patients receiving low-dose diuretic therapy or in patients with a high salt intake, sleep apnea, and chronic kidney disease. These patients can be assessed using impedance methods and/or the therapeutic response to antialdosterone drugs if no contraindication exists. Typical contraindications are a glomerular filtration rate < 45 mL/min/1.73 m2 and hyperkalemia.
Finally, adrenergic hyperactivity is not easily assessed in clinical practice. The relevance of knowing if a patient has this condition lies in its usefulness for selecting truly resistant hypertensive patients, since they would respond better to renal denervation. Currently, there is no proven method to select the patients who are most likely to benefit from renal denervation. Of the various predictors, impaired cardiac baroreflex sensitivity appears to be one of the best predictors of response to renal denervation.18
Based on the foregoing, it appears that far more research is required into refractory hypertension to gain a deeper understanding of the condition, with the aim of reducing its prevalence and providing improved treatment. Meanwhile, the recent European Society of Hypertension and the European Society of Cardiology guidelines17 recommend that, in resistant hypertensive patients, physicians should check whether the drugs included in the multiple drug regimen have a BP-lowering effect and withdraw them if their effect if absent or minimal (class I recommendation, level of evidence C). These guidelines also state that mineralocorticoid receptor antagonists, amiloride, and the alpha-1-blocker doxazosin should be considered, if no contraindication exists (class IIa recommendation, level of evidence B). In the case of ineffectiveness of drug treatment, these guidelines suggest that invasive procedures such as renal denervation and baroreceptor stimulation may be considered (class IIb recommendation, level of evidence C). Until more evidence is available on the long-term efficacy and safety of renal denervation and baroreceptor stimulation, it is recommended that these procedures should be performed by experienced operators and that diagnosis and follow-up should be restricted to hypertension centers (class I recommendation, level of evidence C). It is also recommended that invasive procedures should only be considered for truly resistant hypertensive patients with clinical systolic BP values ≥ 160 mmHg or diastolic BP values ≥ 110 mmHg and with BP elevation confirmed by ambulatory BP monitoring (class I recommendation, level of evidence C).
An improved therapeutic approach and greater reductions in the morbidity and mortality associated with this disease will clearly be achieved by following the recommendations of the guidelines and designing future studies to answer current issues concerning the assessment and treatment of resistant hypertensive patients.19
CONFLICTS OF INTERESTNone declared.