Beta-blocker treatment has a class I indication, level of evidence A, in guidelines for the treatment of heart failure, ischemic heart disease, and atrial fibrillation. However, beta-blocker use continues to be less than optimal. In this study, beta-blocker use in Spain is analyzed in patients with heart failure, ischemic heart disease, and atrial fibrillation.
MethodsObservational, epidemiologic, cross-sectional, multicenter study including 1608 patients with heart failure, ischemic heart disease, and/or atrial fibrillation, recruited in 150 healthcare centers by cardiologists and internal medicine specialists.
ResultsCardiologists enrolled 78.6% patients and internal medicine specialists 21.4%; 25.8% were recruited at hospital discharge and 74.2% at outpatient centers. Men accounted for 77% of the sample, and age was 68 (12) years. Of the total, 73% had ischemic heart disease, 42% heart failure, and 36% atrial fibrillation (multiresponse variable). beta-blockers were given to 82.8% of those consulting in cardiology compared to 71.6% of those treated in internal medicine (P<.0001). By pathology, the prescription rate was 85.1% of patients with ischemic heart disease, 77.0% of those with heart failure, and 72.4% of those with atrial fibrillation. Cardiology prescribed significantly more beta-blockers for ischemic heart disease and heart failure than did internal medicine. Multivariate analysis showed that beta-blocker use increased when the patient had ischemic heart disease, was treated by a cardiologist, and had dyslipidemia, stroke, and/or left ventricular hypertrophy. Beta-blocker use decreased with age and with a history of bronchospasm, asthma, bradycardia, chronic obstructive pulmonary disease, and/or intermittent claudication.
ConclusionsThere is still room for improvement in beta-blocker prescription in Spain for patients with ischemic heart disease, heart failure, and/or atrial fibrillation.
Keywords
Cardiovascular diseases constitute an important public health problem. These severe chronic conditions, particularly ischemic heart disease and cerebrovascular disease, are the main cause of death in our society.1
The prevalence of some of these conditions, for example, chronic heart failure (CHF), is continuously increasing (around 10% in the population older than 70 years),2 affecting the quality of life and survival of patients. The prognosis of patients with heart disease has improved with the advances in preventing cardiovascular risk factors and in treatments, but mortality and morbidity rates remain very high. This is due, in part, to improper use of medication with a proven beneficial effect on cardiovascular disease in general, such as antiplatelet agents, lipid-lowering drugs, angiotensin-converting enzyme inhibitors (ACEIs), and beta-blockers (BBs).3, 4
BB treatment has a significant role in cardiovascular disease, being used for years because of its anti-ischemic, antiarrhythmic, and antihypertensive properties. The favorable effects of adrenergic blockade have been recently established in patients with heart failure.5 The benefits and clinical indications for BB use have been clearly established in several European and American guidelines for the diagnosis and treatment of these conditions (eg, CHF, stable angina, atrial fibrillation [AF]),6, 7, 8 and there is consensus on their use with a class I indication, level of evidence A, in the treatment of chronic ischemic heart disease, CHF, and AF (in this last indication, together with nondihydropyridine calcium channel blockers). Nonetheless, adherence to the guidelines in general and to the use of BBs in particular remains less rigorous that would be desirable and is very disparate between European countries.9, 10, 11
The main objective of this study is to determine the therapeutic use of BBs for class I indications, level of evidence A (ischemic heart disease, CHF, and/or AF) in the clinical practice of specialists prescribing treatment for these patients. The secondary aims are to evaluate which factors determine the use of BBs and whether there are differences regarding the medical specialties in which these patients are treated.
METHODSCARACTER-BETA is a multicenter, cross-sectional, observational study, performed under the aegis of the Hypertension Section of the Spanish Society of Cardiology and conducted in Spain.
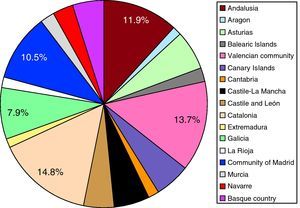
A total of 1608 consecutive patients were recruited in 150 centers from across the country. The geographic distribution of participants by autonomous communities is shown in Figure 1. The recruiting physicians were internal medicine specialists and cardiologists, working in outpatient clinics and hospital wards.
Figure 1. Distribution of the patients included by autonomous communities.
Physicians were chosen from all over Spain, and participation of the patients included by autonomous community was proportionate to the demographic weight of each community within the total in Spain (Figure 1). Patients were consecutively recruited and the number that each participating physician could include was limited to minimize the possibility of selection bias. The inclusion criteria were the following: signed informed consent; age older than 18 years; having been diagnosed of and treated for ischemic heart disease, CHF, and/or AF; and attending regular follow-up visits in an outpatient clinic or having received a hospital discharge. With regard to the heart failure criterion, the condition had to be in a stable phase because the indication for BBs in unstable heart failure is class IIb, level of evidence C.
The exclusion criteria were current participation in a clinical trial involving BBs or presence of any abnormality that could compromise the ability to provide written informed consent for participation and/or fulfill the procedures required for the study.
Among the 1608 patients initially enrolled, 1582 (98.38%) patients were ultimately eligible for the analysis. Patients were considered invalid for the analysis if they did not fulfill one or more of the proposed selection criteria (n=17), had no record of treatment of any kind (n=7), or were receiving more than one BB (n=2).
The study was approved by an independent ethics committee (Ethics Committee for Clinical Research, Hospital de San Juan de Alicante) on 28 March 2007 and was carried out in keeping with the ethics requirements expressed in the Declaration of Helsinki. Patients were informed before recruitment, and they received an information form and signed an informed consent for participation before the study was initiated. The data collected were identified by codes, and confidentiality was maintained in accordance with Organic Law 15/1999 (13 December) for the protection of personal data, and Royal Decree 994/1999 (11 June) regarding security measures for computer files containing personal data.
Statistical Analysis and Sample CalculationThe main study variable was the percentage of patients who, at the time of the visit, were receiving pharmacological treatment in keeping with the guidelines of the European Society of Cardiology, in particular regarding BB use (treated/untreated, indicated/not indicated because of a contraindication).
Sample Size CalculationThe sample size was calculated assuming maximal uncertainty or indifference (p=q=0.5) related to the therapeutic approach in the use of BBs, because of the fact that precise, homogeneous data were not available. Therefore, based on inclusion of 1800 patients in the study, it was calculated that a precision of 2.3% would be achieved in estimating a percentage by a normal bilateral asymptotic 95% confidence interval, assuming that the percentage would be 50% and setting the patient loss rate due to incomplete data at 10%. Nonetheless, following a quality control process of the data obtained, 1582 patients were ultimately included in the study. Because the premise of maximum uncertainty or indifference was not met in the study, but instead was P=.804 and q=0.196, and assuming the same confidence interval, the degree of precision reached was calculated at 1.96%, which was better than the initial target.
Statistical AnalysisThe descriptive statistics included the distribution of frequencies, measures of central tendency, standard deviation, and calculation of 95% confidence intervals. Bivariate analysis of categorical values was performed by comparing contingency tables, using the χ2 test with variables of a nominal type and the Fisher exact test when appropriate. Continuous variables that met the assumptions of normality for dichotomous variables were analyzed with the Student t test and variables with more than 2 categories, by analysis of variance. Variables with a non-normal distribution were analyzed with the Mann-Whitney U test and Kruskal-Wallis test, respectively. The principal study variable, BB use, underwent descriptive evaluation and logistic regression analysis using the stepwise method and including all factors that could have an influence on BB prescription. Significance was set at a two-tailed P value of .05.
RESULTSA total of 1608 patients from across the country were recruited, and 1582 (98.38%) patients fulfilled the selection criteria for inclusion in the analysis. Of the patients included, 79% were from cardiology (1244 patients vs 338 patients from internal medicine), 26% had been discharged from hospital, and 74% were from outpatient clinics.
The baseline characteristics of the population studied are shown in Table 1 and the baseline analytical parameters are summarized in Table 2.
Table 1. Demographic Characteristics of the Study Population.
| Cardiology | Internal medicine | P | |
| Men, % | 67 | 60 | .0027 |
| Age, years | 66.6 | 70.8 | <.0001 |
| Systolic pressure, mmHg | 133.8 (19.7) | 138.1 (18.9) | .001 |
| Diastolic pressure, mmHg | 76.4 (11.5) | 78.9 (18.9) | .0007 |
| Heart rate, bpm | 70 (13) | 74 (12) | <.0001 |
| Hypertension, % | 70 | 81.1 | <.0001 |
| Diabetes mellitus, % | 28 | 45.3 | <.0001 |
| Dyslipidemia, % | 63.4 | 60.4 | NS |
| Stroke, % | 7.6 | 17.8 | <.0001 |
| LVH on ECG, % | 42.9 | 47.4 | .037 |
| Intermittent claudication, % | 5.8 | 11.8 | .0003 |
| COPD, % | 9.7 | 12.1 | .19 |
COPD, chronic obstructive pulmonary disease; ECG, electrocardiography; LVH, left ventricular hypertrophy.
Data expressed as the mean (standard deviation), unless otherwise indicated.
Table 2. Baseline Laboratory Data of the Study Population.
| Analytic parameters | Mean (SD) range |
| Hematocrit, % | 40.4 (5.95) 10.8-60 |
| Hemoglobin, g/dL | 14.1 (3.98) 1.2-53 |
| Creatinine, mg/dL | 1.1 (0.45) 0.1-8.7 |
| Total cholesterol, mg/dL | 189.11 (42.16) 79-346 |
| HDLc, mg/dL | 45.44 (13.45) 10-137 |
| LDLc, mg/dL | 113.76 (35.64) 24-268 |
| Triglycerides, mg/dL | 143.91 (79.44) 28-1085 |
| Glucose, mg/dL | 113.43 (37.53) 20.9-470 |
| Glycohemoglobin, % | 6.84 (1.59) 1-14.2 |
| Sodium, mEq/L | 139.86 (3.71) 105-153 |
| Potassium, mEq/L | 4.39 (0.5) 2.9-6.4 |
| BNP, pg/mL; median (95% CI) range | 77.5 (213.99-750.44) 15-6100 |
BNP, B-type natriuretic peptide; CI, confidence interval; HDLc, high-density lipoprotein cholesterol; LDLc, low- density lipoprotein cholesterol; SD, standard deviation.
Mean age of the study patients was 67.5 (11.6) years, two-thirds were men, and the mean body mass index was 28.35 (4.15). The body mass index was ≥25 in 81.1% of patients. Mean abdominal girth was 97.8 (13.18) cm, and 47.7% of patients had criteria for abdominal obesity (men, >102cm; women, >88cm). The prevalence of hypertension was 72.2%, diabetes mellitus 31.7%, and dyslipidemia 62.8%.
Patients seen in cardiology were younger (66.6 [11.6] vs 70.8 [10.9] years in internal medicine; P<.0001) and there was a higher percentage of men (68.7% vs 59.4% in internal medicine; P<.003). These differences were also seen according to the heart disease under study: patients with ischemic heart disease were significantly younger (66.8 [11.6] years vs 70.2 years for patients with heart failure and 70.8 years for those with AF; P<.0001) and were more often men (72.4% vs 59.6% of patients with heart failure and 56.9% of those with AF).
Echocardiography was performed in 89.8% of the study patients, with no differences between those seen in cardiology or in internal medicine. Mean left ventricular ejection fraction was 55% (55% in ischemic patients, 49% in those with CHF, and 55% in patients with AF). This was an older population, in which the prevalence of heart failure with preserved ventricular function was notable, above all in patients consulting in internal medicine.
With respect to the patients’ habits, 23% consumed alcohol, although only 3% of the total population (11.8% of those who drank alcohol) admitted to drinking more than 80 mg per day. Among the total, 15.3% were active smokers of a mean of 16.1 (9.9) cigarettes per day, and 40.4% practiced some type of physical exercise. Patients consulting in cardiology smoked somewhat less (15.6 [10.2] cigarettes vs 18.5 [7.9] in internal medicine) and exercised more (44.4% vs 25.8% in internal medicine).
BB were prescribed to 85.1% of patients with ischemic heart disease, 77% of those with CHF, and 72.4% of those with AF. In general, patients with ischemic heart disease consulted more often with cardiologists (74% vs 67.5% in internal medicine), whereas internal medicine specialists treated a larger number of patients with CHF (52.1% vs 39% in cardiology) and/or AF (40.8% vs 34.1%).
Use of BBs was similar in hospitals and in the outpatient setting (82.3% at hospital discharge and 79.6% in outpatient clinics). However, BB use was significantly higher in cardiology than in internal medicine (82.8% vs 71.6%; P<.0001). Furthermore, most cardiologists contemplated BB use, and among patients who did not receive them, there was a specific reason in 63.2% and in 11% it was because of intolerance (in internal medicine, 51.8% and 10.8%, respectively). Thus, no reason was given in 25.9% of patients who were not treated with BBs in cardiology (37.4% in internal medicine; P=.05).
Reasons for Not Prescribing Beta-BlockersBB were not prescribed in 19.6% of all patients: in 5.7%, it was not considered to be indicated, in 11.7% it was not prescribed because of a specific reason, and in 2.1%, it was indicated, but not tolerated by the patients.
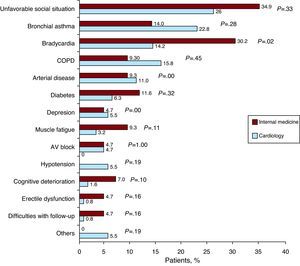
The reasons why BB treatment was not prescribed in cardiology and internal medicine are shown in Figure 2, In internal medicine, an “unfavorable social situation” was given as the main limitation to prescribing BBs. It is worthy of note that the presence of a respiratory disorder was more often the reason for not prescribing BBs in cardiology than in internal medicine, despite the fact that there is a higher prevalence of these disorders in patients treated by internal medicine specialists. In contrast, bradycardia and diabetes mellitus were more important reasons for not prescribing these drugs in internal medicine than in cardiology.
Figure 2. Reasons why beta-blockers were not indicated in patients for whom their use was considered. AV, atrioventricular; COPD, chronic obstructive pulmonary disease.
Beta-Blockers in Ischemic Heart DiseaseThe most common condition under study was ischemic heart disease (72.6% of patients), in which BB use was high, always exceeding 80%. No differences in prescribing these drugs were observed between outpatient treatment and at hospital discharge (84.0% vs 87.9%, respectively). However, their use was more frequent in cardiology than in internal medicine (86.3% vs 80.3%; P<.05). The most commonly used combined regimen was a BB, ACEI, antiplatelet agent, and lipid-lowering drug (42.1% of patients with ischemic heart disease).
Beta-Blockers in Heart FailureAmong the patients included, 41.8% had CHF. New York Heart Association functional class II was the most common (54.5%), accounting for 46% of hospital admissions during the year prior to the study. A depressed ejection fraction (left ventricular ejection fraction<35%) was documented in 46%. Use of BBs was less intense in patients with CHF, with no significant variation between outpatient prescription and hospital discharge (76.9 vs 77%). Similar to what was seen in ischemic heart disease, CHF patients treated in cardiology received BBs more often than patients treated in internal medicine (81.7% vs 64.2%; P<.00005). The most commonly used combination was a BB, ACEI/angiotensin II receptor antagonist, antiplatelet/anticoagulant, diuretic, and lipid-lowering drug (46.4% of CHF patients).
Beta-Blockers in Atrial FibrillationAmong the total series, 35.5% of patients had AF. The diagnosis of this condition had been made in the 3 years before the study (interquartile range, 1-6 years). In 55.6%, AF was permanent, and 25.2% of patients had undergone cardioversion in the previous 2 years. Treatment with BBs was similar in both settings under consideration (outpatient, 71.6%; hospital discharge, 74.8%) and in both medical specialties (cardiology, 74.3%; internal medicine, 66.7%). The most commonly prescribed combination was a BB, ACEI/angiotensin II receptor antagonist, and an anticoagulant (23.1% of FA patients).
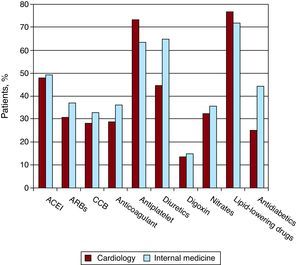
Other TreatmentThe treatments patients received are summarized in Figure 3. Proper use of the other drug groups is evident, such as lipid-lowering drugs, antiplatelet agents, ACEI, and angiotensin II receptor antagonists. These findings are consistent with recently published data in Spanish registries of ischemic heart disease.12
Figure 3. Other treatments received by the patients in this study. ACEI, angiotensin-converting enzyme inhibitor; ARBs, angitesin receptor blockers; CCB, calcium channel blocker.
Independent Predictors of Beta-Blocker UseThe use or not of BBs was considered the dependent variable, and the following variables were considered explicative variables: sex, age, cardiovascular diseases under study (ischemic heart disease, CHF, and AF or atrial flutter), specialty (patient treated in cardiology/internal medicine) and various concomitant diseases (hypertension, diabetes mellitus, dyslipidemia, stroke, left ventricular hypertrophy, hepatic failure, second- or third-degree atrioventricular block, history of bronchospasm and bronchial asthma, bradycardia, hypotension, chronic obstructive pulmonary disease [COPD] and intermittent claudication). Multiple regression analysis was used to determine which variables were independently associated with BB use (Table 3). We entered in the model variables showing differences between using and not using BBs as well as variables with differences between internal medicine and cardiology to adjust for the various baseline characteristics of the patients in these two settings. We saw that as the age of the patient increased, the probability of being prescribed a BB decreased, and that the same was true for a history of respiratory conditions, bradycardia, and intermittent claudication. In contrast, if a patient with ischemic heart disease and/or a history of dyslipidemia, stroke, and/or left ventricular hypertrophy consulted in cardiology, the probability of receiving BB treatment increased. The Hosmer-Lemeshow test indicated that the regression model had satisfactory goodness-of-fit (P=.8808), ie, the degree to which the predicted probability coincides with the observed probability. Lastly, the ROC curve obtained with the model showed good discrimination (P=.758).
Table 3. Multiple Regression Analysis to Identify Variables That Independently Explained the Use or Not of Beta-Blockers in Study Patients.
| Effect | OR (95% CI) | P |
| Constant | 8.3 (2.98-23.13) | <.0001 |
| Age, years | 0.97 (0.96-0.98) | .0003 |
| Ischemic heart disease | 2.3 (1.6-3.31) | <.0001 |
| Follow-up by cardiology | 1.7 (1.24-2.34) | .001 |
| Dyslipidemia | 1.72 (1.28-2.3) | .0002 |
| Stroke | 1.64 (1.02-2.66) | .041 |
| Left ventricular hypertrophy | 1.51 (1.13-2.03) | .0051 |
| History of bronchospasm and bronchial asthma | 0.22 (0.13-0.38) | <.0001 |
| Bradycardia | 0.28 (0.15-0.54) | .0002 |
| COPD | 0.39 (0.26-0.6) | <.0001 |
| Intermittent claudication | 0.35 (0.22-0.57) | <.0001 |
CI, confidence interval; COPD, chronic obstructive pulmonary disease; OR, odds ratio.
Other variables entered in the model that were not statistically significant: diabetes mellitus, atrial fibrillation, hypertension, hypotension, heart failure, hepatic failure, and sex.
BB use in Spain has improved over the past decade. Data from the Spanish registries PREVESE I and II (patients with acute myocardial infarction), 3C program (patients at discharge following an acute coronary syndrome), PRIAMHO (acute coronary syndrome with ST segment elevation), and DESCARTES (acute coronary syndrome without ST segment elevation) show BB use in 50% to 60% of patients with acute ischemic heart disease.13, 14, 15, 16, 17, 18 Furthermore, in the more recent studies BB use is seen to increase, as shown in Table 4, which also includes data from the EUROASPIRE and TRECE registries.19, 20, 21, 22 In the present study, we observed an increase in the use of these drugs for ischemic heart disease (more than 80% of patients) and for CHF (around 75%). The ischemic heart disease data are in line with the overall results from EUROASPIRE III (around 80%),19 in which the data were collected 2 years before those from the present study. The specific data for Spain, however, were lower (around 60%).
Table 4. Evolution of Beta-Blocker Treatment Over the Past 15 Years in Ischemic Heart Disease Registries.
| PREVESE I 13 | EUROASPIRE I 19 , a | Programa 3C 15 | PREVESE II 16 | EUROASPIRE II 20 , a | EUROASPIRE III 21 , a | TRECE 22 | CARACTER BETA b | |
| Year | 1994 | 1995 | 1998 | 1998 | 1999 | 2006 | 2006 | 2008 |
| Patients, n | 1329 | 4863 | 3074 | 2054 | 5556 | 8966 | 2897 | 1582 |
| Beta-blockers, % | 33.3 | 53.7 (34.7) | 37.4 | 45.1 | 63 (47) | 80 (60) | 64.5 | 80.4 (85.1) |
a Between parentheses, data for Spain.
b Between parentheses, data for ischemic heart disease.
In the present study, we found differences in BB use according to the attending specialty (cardiology or internal medicine) and according to the setting (hospital discharge or outpatient treatment). Overall, BBs were used more in cardiology than in internal medicine, whether to treat ischemic heart disease, CHF, or AF. Although in AF the difference showed a trend similar to that of the other 2 disease groups, it did not reach statistical significance, likely because of the smaller number of patients included. The difference was, however, very evident in the treatment of heart failure, in which 64.2% of patients treated in internal medicine received BBs compared to 81.7% of those treated in cardiology, with both values being lower than the BB use reported in the recently published SHIFT study.23 A part of the treatment differences between specialties can be explained by the differing baseline characteristics of the patients treated in each of them. For example, the percentage of women was higher in internal medicine, and women received BBs less frequently than men. Nonetheless, patients treated in internal medicine had a higher prevalence of cardiovascular risk factors (older age and a higher prevalence of hypertension and diabetes) and more extracardiac manifestations of atherosclerotic disease (stroke and intermittent claudication); hence, one could infer the opposite: because they had a higher risk profile, internal medicine patients should show a greater prevalence of BB treatment than those in cardiology. As to the setting in which patients were treated, at discharge from hospital or on an outpatient basis, this factor had a smaller impact on BB prescription.
It was interesting to note that the reasons for not prescribing BBs differed between cardiology and internal medicine. One of the stated causes, “unfavorable social situation”, could be interpreted as an umbrella category that would encompass various conditions. It was found that cardiologists cite COPD more often than internal medicine specialists as a reason for not prescribing these drugs (38.6% vs 23.3%), whereas internists cite bradycardia more often (30.2% vs 14.2%). Furthermore, it is worthy of note that diabetes mellitus remains a reason for not indicating treatment in 11.6% of patients in internal medicine and 6.3% of those in cardiology. These differences may be explained by the type of disease: COPD is treated more commonly in internal medicine, whereas bradycardia is seen and treated more often in cardiology.
The matter in which there were significant differences between the two specialties was in the percentage of patients for whom BB treatment was not contemplated: 25.9% in cardiology and 37.4% in internal medicine, a statistically significant difference on which efforts should be focussed to improve daily clinical practice.
Multivariate analysis showed various areas in which the BB prescription rate can be improved. A series of variables that have been historically related to a “contraindication” for BB treatment (eg, respiratory disease or intermittent claudication) are now considered free of this contraindication (with the exception of respiratory disease with a potential for bronchospasm). Another variable, age, is a classic in interventional studies. In the present study, it was reaffirmed that as age increased, treatment decreased, in this case BBs, despite the published evidence on BB use in patients of advanced age.24
The limitations of this study are those inherent to any observational registry that does not allow a stratified adjustment of the patients. Furthermore, there is some selection bias related to nonrandomized recruitment of the participating medical specialists, as well as a unbalanced representation of acute phase (at discharge) and ambulatory patients included, which could detract from the external validity.
CONCLUSIONSThe data from this study show that the BB use for cardiovascular diseases in which treatment with these drugs is highly recommended by scientific societies has improved in Spain with respect to previous registries. Nevertheless, there are still significant differences between cardiology and internal medicine, even after adjusting for the baseline characteristics between patients treated in these two specialties. The reasons for not prescribing BBs differ between cardiologists and internal medicine specialists, and there remains a considerable number of patients in whom the use of these drugs is not contemplated even though there is a clear indication, particularly outside the cardiology setting. These data, the first obtained in a nationwide study, show that there is still room for improvement in BB prescription in Spain, in particular for patients with CHF or AF.
FUNDINGThis project was funded by an unrestricted grant from Laboratorios Menarini S.A.
CONFLICTS OF INTERESTSAntonio Zapata and Remei Artigas are employed in the Medical Department of Menarini, the laboratory that provided an unrestricted grant to carry out this study.
Appendix A. Investigators Participating in the First Phase of the CARACTER-BETA StudyCarlos Pons de Beristain, Carme Amorós, Mohammad Elsaheb Daaboul, Pere Álvarez García, Josep Pinar Sopena, Nicolás Ortega López, Carlos Lafuente Gormaz, Antonio Castilla Núñez, Fermín Martínez García, Salvador Moreno Honorato, M. Luz Cardo Maeso, Manuel Rayo Gutiérrez, Alejandro Berenguel Senén, Fernando López Sánchez, Jorge Raúl Castro Dorticos, Jesús Saavedra Falero, Óscar González Lorenzo, José Antonio Núñez Gamero, Vilma Monagas Miller, Verónica Suberviola Sánchez-Caballero, Alberto Chocamo Higueras, Luis Miguel Cuadrado Gómez, Florentino García González, Francisco Alonso Montero, José Luis Álvarez Cuesta, Eddi Velasquez Arias, José Carlos Porro Fernández, Fernando Samaniego Rodríguez, José María Martínez Díaz, Juana Freire Corzo, Milagros Pedreira Pérez, José Enrique López Paz, Rosa María Campo Pérez, María Bastos Fernández, M. Dolores Martínez Ruiz, Eduardo Caballero Dorta, Egon Gross Kasztovits, Efrén Martínez Quintana, Federico Segura Villalobos, Xavier García-Moll, Jose Manuel García Ruiz, Alvaro Gonzalez Franco, María Dolores Martín Cid, José Sergio Hevia Nava, Vicente Barriales Álvarez, Gonzalo Marcos Gómez, Sabino Antonio Sáez, Andrés Pérez Garrido, Manuel Maestre García, Alfredo Luis Michan Doña, Juan Manuel Adriasens Abad, Miguel Ángel Rico Corral, Román Calvo Jambrina, Gonzalo Barón Esquivias, Juan Andreu Álvarez, José Antonio Bernal Bermúdez, María Amalia Acuña Lorenzo, Humberto Mendoza Ruiz De Zuazu, Teresa M. Pérez Sanz, José Javier Moreno Palomares, Luis María Álvarez Gallego, Virginia Montero Gato, Javier Cabezón Gutiérrez, Juan María Irigoyen Rodríguez, Miren Morillas Bueno, Julio Martínez Flores, Javier Andrés Novales, Juan José Villareal, Ángel Brea Yernando, Imad Eldin Yousef Hat Hat, Joaquín Canoves Femenia, Antonio Toral Noguera, Juan Quiles Granado, Juan Luján Martínez, Miguel García Martínez, Javier Pereira García-Tizón, Ernesto Ortiz Vecino, Jesús Grandes Ibáñez, Francisco Alonso Valladares, Jesús Segovia Castro, Manuel Rodríguez Revuelta, Jaime Fernández-Dueñas Fernández, Francisco Javier Rivera Guzmán, Eduardo Carmona Nimo, Martín Ruiz Ortiz, Fernando Olaz Preciado, Juan María Arnedillo Pardo, Juan Pérez Calvo, Fidel Sardaña Cardiel, Julio Sánchez Álvarez, Jorge Parra Ruiz, José Luis Ramos Cortés, Hipólito Pousibet Sanfeliu, Carmelo Ruiz Ortiz, Antonio Jesús Martín de la Higuera, Jorge M. Alegret, Guillermo Federico Mazzanti, Pedro Castellanos Llauger, Lluis Carles Olivan Sayrol, Moisés Cadierno Carpintero, Agustín Ardiaca Capell, Miguel Ángel Sáanchez-Corral Mena, Ramon de Castro Aritmendiz, Rosa Gilabert Gómez, Vicente Oliver Morena, Julio Núñez Villota, Pau Federico Zaragoza, Pablo Aguar Carrascosa, Araceli Roselló Serralta, Carlos García Palomar, Lorenzo Fácila Rubio, M. José Bosch Campos, Pedro Rollán García, Juan Cosin Sales, Rafael Cuenca Luque, Ramon Boixeda Viu, Edgardo Kaplinsky, Julio Carballo Garrido, Joan Sala Montero, Rosa Piulats Egea, Francisco Martí Ramón, Carlos Alberto Valle Gort, Julio Jesús Ferrer Hita, Miguel Bethencourt Muñoz, Ángel Montiel Trujillo, Juan Robledo Carmona, Eloy Rueda Calle, Carlos Gómez Navarro, María Guil García, Álvaro Rubio Alcaide, Juana Núñez Morcillo, Joan Torres Marqués, José María Gamez Martínez, José María Turiel Martínez, Inés Möller Bustinza, Alberto Riera Garcia, José Alonso González, Francisco González Vilchez, Salvador Diez-Aja López, Santiago Cantabrana Miguel, Juana María Gallego García, José Manuel Rubio Campal, Honorio Gervás Pabón, Jorge Oria Vidal, Javier David Romero Roldán.
Received 31 January 2011
Accepted 29 May 2011
Corresponding author: Servicio de Cardiología, Hospital de la Santa Creu i Sant Pau, Sant Antoni Maria Claret 167, 08025 Barcelona, Spain. xgarcia-moll@santpau.cat