Cardiac pacing has drastically improved over the last 2 decades, with complex treatment and technologies focused mainly on resynchronization. Less progress has been made in advancing pacing therapy for bradyarrhythmias and therefore apical and septal pacing represent daily practice in most electrophysiology laboratories. Over time it became clear that abnormal impulse conduction was leading to “iatrogenic” dyssynchrony, which has a significant impact on ventricular function, both acutely and in the long-term. His bundle pacing (HBP) is the most physiological way to pace the heart, as it replicates the ventricular activation that spreads through the specific conduction system, avoiding dyssynchrony, ventricular dysfunction, and heart failure (HF). Several single-center studies have demonstrated the feasibility, safety and positive clinical outcomes of HBP. Data are becoming available on long-term performance in multicenter experiences. Our group has contributed to the development of the HBP technique with extensive experience since 2004. Interesting scenarios are emerging on HBP in cardiac resynchronization therapy (CRT) both alone or in combination with left ventricular (LV) pacing. An intriguing alternative called intraseptal left bundle branch pacing (LBBp) is extending the possibilities for physiologic pacing. Today we can safely consider HBP in overall heart rhythm disturbances. In this article we aim to guide the reader through the journey of HBP starting with the initial enthusiasm, leading to disillusionment with its possibilities, and finally reaching widespread acceptance and approaching the standard of care.
RATIONALEMuch evidence indicates that not only apical pacing but any myocardial site in the right ventricle (RV) is associated with detrimental hemodynamic effects. The slow propagation through the ordinary myocardium produces dyssynchrony and LV dysfunction, particularly in patients requiring a high percentage of pacing, thus increasing the risk of HF, atrial fibrillation, and mortality. As a consequence, physicians searched for alternative pacing sites allowing a more physiological activation pattern and better hemodynamics. In this scenario, HBP has been proposed as it yields fast and normal ventricular activation via the specific conduction system, drastically reducing the dyssynchrony index. Several studies have shown the feasibility, safety, and positive clinical outcomes of HBP compared with standard RV apical pacing. A recent systematic review and meta-analysis of single-center studies performed in China, the United States and Europe has shown that HBP is practical and feasible with acceptable pacing thresholds, and a low rate of complications in routine clinical practice.1 HBP not only maintains synchrony but can also reverse pacing-induced cardiomyopathy (PICM). In a multicenter experience, the upgrade to HBP after a mean of 6 years of RV apical pacing significantly decreased QRS duration (114±20ms during HBP vs 177±17ms during RV pacing; P <.001) and improved ejection fraction (48.2±9.8 during HBP vs 34.3±9.6% during RV pacing; P <.001).2 Another study reported better left atrial function during HBP compared with RV apical and septal pacing with a lower incidence of persistent or permanent atrial fibrillation.3 In a direct comparison with RV apical pacing, HBP showed better clinical outcomes: HF hospitalizations were significantly reduced (2% vs 15%; P=.02) in patients with> 40% ventricular pacing.4
SHOULD HIS BUNDLE PACING REPLACE ALL RV PACING?The clinical benefits of HBP are no longer in doubt. However, to implement HBP in regular clinical practice, its application needs to be easier. The initial experience with a standard lead and stylet5 resulted in prolonged procedures and low success rates. Zanon et al.6 first described the feasibility of HBP by means of a steerable delivery system and a lead with a fixed helix, obtaining an implant success rate of 92% in 26 patients with preserved conduction. Sharma et al.7 reported an implant success rate of 80% in 94 patients. Initially proposed in patients with preserved His-Purkinjie conduction, HBP is now indicated in all kinds of conduction disturbances, including infra-nodal, infrahisian block, and bundle brand block (figure 1 and figure 2). With increased procedural experience, the feasibility of HBP in all-comers is> 90%. Although HBP demonstrates clear clinical benefits, appropriate patient selection remains to be defined.
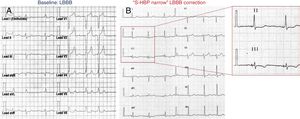
Case report: a 54-year-old woman with nonischemic cardiomyopathy, mild ejection fraction reduction. Pacing indication due to first and paroxysmal second degree atrioventricular block. A, baseline ECG and left bundle branch block (LBBB) morphology. B, ECG after 10 months of follow-up. The small window shows the narrow paced QRS (84ms). S-HBP, selective His bundle pacing.
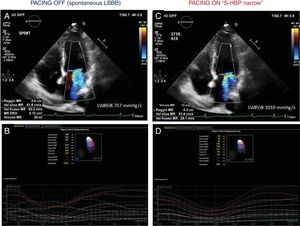
Echocardiography analysis of the same case as in figure 1, at 10 months of follow-up. Panels A and B are recorded during “PACING OFF” which means turning pacing at VVI 40/min. Panels C and D are recorded during “PACING ON” which means during selective His bundle pacing with QRS and left bundle branch block (LBBB) normalization. His bundle pacing reduced mitral regurgitation, increasing left ventricular dP/dt and drastically reduced dyssynchrony indexes. S-HBP, selective His bundle pacing.
Pacing the His bundle may result in different ECG patterns, reflecting the anatomic position of the lead in relation to the His bundle and the amplitude of the pacing output. Recently, a multicenter collaborative working group refined the definition of HBP.8 Selective HBP (S-HBP) is the capture of the His bundle only, producing a QRS identical to the native QRS, with the characteristic spike-QRS delay, expression of the HV interval. Nonselective HBP (NS-HBP) is defined as the simultaneous activation of His bundle and myocardial ventricular septum creating 2 activation fronts. The former result is easier to perform and is associated with similar beneficial effects of S-HBP due to early propagation through the rapid-conducting His-Purkinjie system without impacting the total LV activation time. Kronborg et al.9 studied 37 patients with high degree atrioventricular (AV) block, narrow QRS, and normal ejection fraction. During NS-HBP the QRS was close to baseline and hemodynamics were significantly improved. Occhetta et al.10 showed a significant improvement in clinical outcomes with both S-HBP and NS-HBP during a mean of 27 months; moreover, QRS duration and pacing threshold did not exhibit any significant variations during follow-up.
IMPLANT PROCEDURE: CHANGES OVER THE YEARSThe small target and fibrous tissue surrounding the bundle challenges the localization and fixation of the lead at the His. In 2000, Deshmukh et al.5 first reported permanent HBP in patients with HF and rapid atrial fibrillation. During 42 months of follow-up, ejection fraction increased from 23±11% to 33±15% and the New York Heart Association class improved from 3.5 to 2.2. This pioneering study paved the way for several investigations across the world from small single center experiences to randomized studies. Due to the positive results, HBP has been recently implemented in the American guidelines with a Class II indication.11 The development of a specialized pacing lead (SelectSecure 3830 Medtronic, United States) and sheaths (C304 deflectable and C315 fixed curve SelectSite, Medtronic, United States) have made HBP feasible in routine clinical practice, with marked improvement in implant success rates (> 90%) and highly acceptable lead positioning and fluoroscopy times.6 The initial experience was guided by the electrophysiology mapping catheter to locate the largest His deflection. The system (delivery plus lead) was directed near the distal dipole of the diagnostic catheter confirming the correct position by fluoroscopic views. This technically challenging and time consuming approach was a necessary step to increase knowledge in the new technique. The mapping catheter was gradually abandoned in favor of a unipolar mapping from the tip of the lead. In addition, we shifted from the deflectable to the fixed curve delivery sheath when it became available, using the distal curve points perpendicularly to the septum, which ensured a more precise and secure lead fixation.12 From the beginning, the importance of the continuous 12-lead ECG monitoring together with the unipolar signals from the lead (sweep speed, 100mm/s; gain, 0.05mV/mm) during HBP implantation was clear in order to verify the capture of the conduction system and to compare the paced QRS morphology during output maneuvers. When an acceptable His signal was obtained (atrial to ventricular electrogram ratio at least 1:2), unipolar pacing was tested starting at a high voltage (10V/1ms), documenting changes in QRS morphologies, named His and RV capture thresholds along with bundle brand block correction thresholds, for the purpose of programming final output settings and follow-up. In the case of unsatisfactory parameters, the lead was unscrewed and a new position was tested. In selected patients, an additional back-up lead can be implanted in the RV apex or septum for safety reasons (the block can broaden, encompassing the lead) to overcome low sensing issues and to reduce the His safety margin output if there are high thresholds. Ventricular pacing avoidance algorithms, when appropriate, were used. Algorithms for automatic capture were never used for the Hisian lead.
CAN HBP BE USED FOR CRT?CRT is certainly an important advancement in HF treatment, as it reduces morbidity and mortality in patients with LBB block (LBBB) and severe LV dysfunction.13 However, its success strictly depends on adequate patient selection and LV lead position. Nevertheless, 30% of patients are nonresponders. Small reports suggest that HBP could represent an intriguing alternative in CRT candidates. It can re-engage the left fascicular tissue overcoming the longitudinal dissociation. Narula et al.14 had already shown in the 1970s that pacing distally to the block leads to normalization of the QRS in LBBB. A crossover study by Lustgarten et al.15 compared NS-HBP with CRT in patients with standard indication for CRT and LBBB. In that study, a Y-adapter connected both HB and LV leads to the LV port. The authors were able to normalize the QRS in 72% of cases. Clinical and echocardiographic responses were similar to those of BIV patients, suggesting that NS-HBP was at least as effective as CRT. The LV ejection fraction improved from 26% to 32% and 31% in NS-HBP and standard CRT, respectively, after 6 months. A Spanish study16 showed ventricular mechanical synchrony in addition to electrical resynchronization and optimal clinical response. The authors underlined the immediate abolition of septal-to-posterior wall delay during HBP at M-mode color tissue Doppler, and the shortening of isovolumetric conduction time at pulsed wave tissue Doppler. Padeletti et al.17 demonstrated that HBP plus LV pacing improves systolic function and LV synchrony regardless of the AV delay setting. Our group also tested the hypothesis that permanent HBP could be combined with LV epicardial pacing in patients with CRT indication to obtain a more physiologic resynchronization.18 In 24 patients with a CRT-P indication, we added the Hisian lead (RV port) to the LV lead (LV port). Interestingly, after a mean of 5.3 years of follow-up, the patients showed persistence of narrow QRS (mean 128ms) and significant ejection fraction improvement (mean 45%), and only 8 patients (33%) experienced HF hospitalization. The mean longevity of the device was 4.3 years. No significant increases were reported in the Hisian lead threshold. This first pioneering experience mimics the “adaptive CRT” algorithm with the advantage of stable pacing independent of variations in PR interval due to heart rate increase during effort. Recent observations by Upadhyay et al.19 provided new insights into the electrophysiology of LBBB. Among 72 patients studied, the authors showed complete conduction block in 46 (64%) (46% left infrahisian; 18% LBBB) and obtained QRS narrowing/correction with HBP in 94% and 62% respectively. A total of 26 patients (36%) had intact Purkinje activation without QRS correction with HBP. HBP is not able to overcome distal disease. In those cases, an integrated approach with multiarea pacing sites to capture a wider area and restore synchronicity is probably the best approach. The latter is the idea behind the His-optimized-sequential LV pacing (HOT-CRT). In patients with only a partial narrowing of bundle brand block or intraventricular conduction delay, CRT could be optimized by sequential HBP followed by LV pacing to maximize electrical resynchronization. Tested in 25 patients over a mean follow-up of 14 months, ejection fraction improved from 24±7% to 38±10% (P <.0001) and New York Heart Association class improved from 3.3 to 2.2. A total of 84% were clinical responders and 92% were echo responders.20
LBBp: THE EVOLVING CONCEPT OF CONDUCTION SYSTEM PACINGThe His bundle penetrates the ventricular septum and then divides into 2 branches, right and left. Following this anatomic route, Huang et al.21 proposed to directly pace the left bundle with a lead screwed deeply inside the ventricular septum. The lead is screwed 1 to 2 centimeters below the His from the right side of the septum until it reaches the left side, capturing the left bundle selectively or nonselectively. This approach broadened the possibilities for physiologic pacing and evolved into the new concept of cardiac conduction system pacing. LBBp maintains the physiologic activation of the LV and promising preliminary reports show better electrical parameters (low thresholds and better sensing values). A report of 100 patients described 3% of lead dislodgement. As a new and promising technique, long-term follow-up and feasibility are needed.
LONG-TERM FOLLOW-UPMost published studies describe a small number of patients with short follow-up. Three studies, a single center in China with more than 300 patients,22 a multicenter study in the UK with more than 500 patients,23 and a multicenter study in Italy-United States with more than 800 patients,12 reported the feasibility and reliability of HBP in long-term follow-up. Recently, a 2-center experience was published on long-term technical and safety endpoints in a large cohort of patients with pacemaker indications treated with HBP. Zanon et al.24 reported the outcome of 307 patients treated with HBP with a mean follow-up of 20±10 months and showed that electrical parameters remained stable over time. The event rate was 5.7%, all due to high pacing thresholds (> 5V), with need for lead replacement in 2 patients. In a minority group of patients, the threshold problems were solved by switching to RV apical pacing. The main problem is the possible increase of threshold over time due to microdislodgement or local fibrosis. Acute thresholds can be higher than RV apical pacing, but chronic thresholds remain stable over a 2-year follow-up. Some authors suggested that the injury current at the time of HB implant is associated with significantly lower pacing thresholds at implant and during follow-up. Similar to our experience, Dandamudi et al.25 reported no cases of syncope due to loss of capture over nearly 7 years of follow-up. Up to 5% of lead revisions were needed due to intermittent loss of capture or significant increase in threshold, and less than 1% of lead revisions were due to sensing issues.
FINAL CONSIDERATIONSConventional myocardial pacing could alter the global physiology and function of the heart. Pacing of the conduction system aims to maintain or restore physiologic conduction. Data are available on its reliability and feasibility. Growing evidence is strengthening both good technical performance and clinical outcomes, even during long-term follow-up. Both S-HBP and NS-HBP can be regarded as physiologic pacing modalities. HBP requires its own learning curve and the beginner could encounter challenges, possibly needing longer implant times and higher pacing thresholds. Improving implanting tools, devices, and algorithms could solve some issues. LBB pacing is emerging as a new and promising technique to extend the pacing of the conduction system, but is still limited due to a lack of long-term data. Large, randomized multicenter clinical trials are needed to definitively prove mortality benefits. Cost-effectiveness analyses are still lacking. Guidelines are already opening the way to consider HBP as a first-line approach in patients who need a high frequency of pacing.
CONFLICTS OF INTERESTF. Zanon reports having received modest speaker fees from Abbott, Biotronik, Boston Scientific, Medtronic and Microport. G. Pastore and L. Marcantoni have no conflicts to disclose.
.