High-sensitivity cardiac troponin (hs-cTn) assays were introduced in Spain in 2010. These methods can detect minimal concentrations of cTn with analytical precision and identify the slightest amount of myocardial damage. However, their ability to detect myocardial injury not identifiable with pre-existing methods (contemporary or conventional cTn) has reduced the diagnostic specificity of acute myocardial infarction (AMI) because the myocardial damage detected can have any cause, not just ischemia, particularly when it is minor. Because there is a tendency to prioritize the diagnosis of AMI over other possible diagnoses, the use of hs-cTn fosters uncertainty in emergency departments and overload in cardiology services. Hence, it can be considered a false friend.
With the support of the Spanish Society of Cardiology, the Spanish Society of Emergency Medicine, and the Spanish Society of Laboratory Medicine, a consensus document was recently published with recommendations on the use and interpretation of cTn in emergency departments.1 The objective of this editorial is to discuss the contributions and limitations of hs-cTn in the evaluation of patients with suspected acute coronary syndrome (ACS).
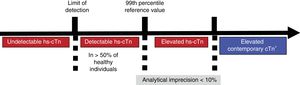
HIGH-SENSITIVITY TROPONIN VS CONTEMPORARY TROPONINCurrent ways to measure cTn comprise contemporary methods, which include all “point of care” assays, and “high-sensitivity” methods. The latter have 2 characteristics lacked by the contemporary methods, either totally or partially: an analytical imprecision less than 10% to measure concentrations corresponding to the 99th percentile (p99) of a reference population (Figure 1) and detection of cTn concentrations above the”limit of detection“but lower than the p99 in more than 50% of healthy individuals. A troponin level above the p99 is considered to indicate significant myocardial damage. Some contemporary methods can measure the p99 with sufficient precision, allowing this value to be used in decision-making, but they do not detect cTn in more than 50% of healthy individuals.
Diagram showing increasing blood concentrations of cardiac troponin in relation to high-sensitivity cardiac troponin and conventional cardiac troponin. cTn, cardiac troponin; hs-cTn, high-sensitivity cardiac troponin. *Some contemporary methods for measuring cTn allow the use of the 99th percentile for detecting myocardial injury by measuring it with an imprecision < 10%. For the other methods, the use is recommended of the measurable concentration with 10% imprecision as the decision limit.
The results of the Spanish multicenter PITAGORAS study contrasted the usefulness of hs-cTn with that of the contemporary method.2 The study enrolled patients attending the emergency department for chest pain who did not have elevated cTn on a contemporary assay. Using the same blood samples, hs-cTn was centrally determined and the patients were classified into 3 groups according to hs-cTn concentration: a) undetectable, hs-cTn <the limit of detection (35% of patients); b) detectable, hs-cTn ≥ the limit of detection but <the p99 (51%); and c) elevated, hs-cTn ≥ the p99 (14%). After adjustment for clinical variables, patients with a detectable or elevated hs-cTn experienced more cardiovascular complications during follow-up than those with undetectable hs-cTn. Consequently, determination of hs-cTn allows AMI diagnosis with cTn concentrations lower than those required for contemporary cTn, as well as detection of hs-cTn concentrations less than the p99 with potential prognostic value.
RULE-OUT OF ACUTE CORONARY SYNDROME: HIGH-SENSITIVITY TROPONIN AS A TRUE FRIENDA considerable number of patients attending the emergency department for chest pain do not have an ACS. The aim in emergency departments is to optimally select candidates for rapid discharge with a minimal risk of cardiovascular complications. In the diagnosis of ACS, a percentage of diagnostic errors ≤ 1% is considered acceptable, which implies a negative predictive value (NPV) of 99% with a sensitivity (S) of 99%.3 This is a challenge because, among patients with normal hs-cTn (< the p99), up to 3.4% may experience adverse cardiovascular events at 30 days, which probably indicates that an ACS was indeed the cause of the chest pain leading to the emergency department visit.4
The rapid rule-out algorithms of AMI are possibly the main clinical contribution of hs-cTn. These algorithms have been developed by expert consensus to exclude a diagnosis of AMI, without consideration of a diagnosis of unstable angina. They assume that an AMI can be ruled out from the initial hs-cTn result or after its short serial measurement. However, because they have also been validated for the occurrence of cardiovascular complications during short-term monitoring, which can occur in both patients with AMI and those with unstable angina, from a practical point of view, we will consider them algorithms with the ability to exclude ACS. Thus, by combining the clinical history, electrocardiography, and hs-cTn algorithms, we can often rule out ACS without the need for noninvasive ischemia tests or coronary computed tomography. Noninvasive tests substantiate the diagnosis, at the expense of speed. In general, they are not continuously available and some patients without heart disease have to wait or be admitted to the hospital until the examination. In addition, the systematic use of noninvasive tests has not been proven to improve prognosis and may increase the number of unnecessary invasive procedures and revascularizations.5
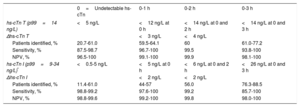
The proposed algorithms are as follows (Table 1):
- 1.
Algorithm with hs-cTn determination at admission (0hours). Several studies and meta-analyses indicate that ACS is ruled out by undetectable hs-cTn concentrations and an ECG on arrival at the emergency department that does not indicate ischemia.3,6 This suggestion is highly appealing because it implies discharge after a single determination of hs-cTn. The NPV and S are very high, reaching the 99% safety criterion, although not in all studies. With this algorithm, it should be considered that analytical variations affecting the measurement of the limit of detection (reagent generation or lot, measurement instrument) can affect both the NPV and the S.
- 2.
Algorithms with hs-cTn measurement at admission and 1 or 2hours later. These algorithms use the concentration of hs-cTn on arrival at the emergency department and its kinetics—or delta (Δhs-cTn)—1 or 2hours later.7 The initial concentration of hs-cTn and its Δhs-CTn, expressed in absolute values, determine the exclusion criteria for ACS. The yield of these algorithms is excellent in terms of the number of patients excluded and their NPVs, although the S fails to reach 99% in all studies, particularly with the 0- to 1-hour algorithm (Table 1). Practically, there may be logistical difficulties in obtaining 2 samples and 2 hs-cTn results at 1 hour.
- 3.
Algorithm with hs-cTn measurement at admission and 3hours later. A hs-cTn less than the p99 at both admission and 3hours later indicates that ACS can be excluded.7 The NPV of the algorithm is very high, but the S is far from 99%. The algorithm may be more useful for ruling out AMI than unstable angina. In contrast, the 0-, 0- to 1-, and 0- to 2-hour algorithms can identify the entire spectrum of ACS when considering hs-cTn concentrations between the limit of detection and the p99.
Algorithms for serial determination of high-sensitivity cardiac troponin for ruling out the diagnosis of acute myocardial infarction
| 0=Undetectable hs-cTn | 0-1 h | 0-2 h | 0-3 h | |
|---|---|---|---|---|
| hs-cTn T (p99=14 ng/L) | <5 ng/L | <12 ng/L at 0 h | <14 ng/L at 0 and 2 h | <14 ng/L at 0 and 3 h |
| Δhs-cTn T | <3 ng/L | <4 ng/L | ||
| Patients identified, % | 20.7-61.0 | 59.5-64.1 | 60 | 61.0-77.2 |
| Sensitivity, % | 87.5-98.7 | 96.7-100 | 99.5 | 93.8-100 |
| NPV, % | 96.5-100 | 99.1-100 | 99.9 | 98.1-100 |
| hs-cTn I (p99=9-34 ng/L)* | <0.5-5 ng/L | <5 ng/L at 0 h | <6 ng/L at 0 and 2 h | <26 ng/L at 0 and 3 h |
| Δhs-cTn I | <2 ng/L | <2 ng/L | ||
| Patients identified, % | 11.4-61.0 | 44-57 | 56.0 | 76.3-88.5 |
| Sensitivity, % | 98.8-99.2 | 97.6-100 | 99.2 | 85.7-100 |
| NPV, % | 98.8-99.6 | 99.2-100 | 99.8 | 98.0-100 |
hs-cTn, high-sensitivity cardiac troponin; NPV, negative predictive value; p99, 99th percentile.
The percentages of patients identified for exclusion, NPV, and sensitivity represent the range found in the different studies.
In summary, the rule-out algorithms are an excellent aid to confidently identify patients who are candidates for rapid discharge. However, the following limitations should be borne in mind: a) they should be applied with caution to “early presenters” (in the first 3hours from the beginning of the pain), particularly the algorithm comprising a single hs-cTn determination at admission (0hours), because at least 3hours may be required for an increase in blood hs-cTn concentrations; b) they require that the analytical inaccuracy of the hs-cTn measurement be as low as possible, especially at very low concentrations, as well as rigorous adherence to blood sampling times in the emergency department; c) age, sex, and renal function, factors that modify the hs-cTn concentration, can affect the NPV and S; d) the diagnostic S to exclude/identify ACS does not reach 99% with all of the algorithms; and e) the algorithms have been developed and validated in observational studies without interventions. Thus, intervention studies with decision-making based on algorithms are required for the complete clinical validation of these algorithms.
Risk scales including clinical data, such as the GRACE, TIMI, and HEART, have been used when considering the discharge of patients with chest pain and low probability of ACS. None of these scales has the NPV or S of the hs-cTn algorithms4; however, they can be an excellent complement. Thus, the integrated use of a hs-cTn algorithm and a clinical evaluation should be sufficient to determine the rapid discharge of a low-risk patient and to limit noninvasive tests to very specific situations. This strategy, as well as expediting discharge, would avoid invasive procedures and unnecessary revascularization motivated by noninvasive tests.
All of these factors allow hs-cTn to be considered a”true friend“for ruling out ACS.
RULE-IN OF ACUTE MYOCARDIAL INFARCTION: HIGH-SENSITIVITY TROPONIN AS A FALSE FRIENDThe fourth definition of AMI generically defines myocardial injury as a cTn elevation above the p99.8 The myocardial injury is considered acute if a significant Δhs-cTn is evident in serial measurements of cTn. The magnitude of the Δhs-cTn value indicating acute myocardial injury is being debated; some studies indicate that an absolute value allows acute injury to be ruled out/identified better than a percentage value. However, the fourth definition of AMI states that a Δhs-cTn indicates acute myocardial injury if it is> 50% of an initial hs-cTn value <the p99 or> 20% of an initial hs-cTn value> the p99.8
Clinical scenarios with evidence of myocardial injury can be acute (with a Δhs-cTn) or chronic (without a Δhs-cTn). This classification is not entirely perfect because the absence of a Δhs-cTn does not completely rule out acute myocardial injury.9 In addition, when the hs-cTn concentrations have peaked, the Δhs-cTn may not be significant. The most frequent causes of acute myocardial injury are type 1 AMI, type 2 AMI, and nonischemic myocardial injury. The most frequent causes of chronic myocardial injury are chronic ischemic heart disease, nonischemic structural heart disease, and extracardiac factors (eg, renal failure). Occasionally, a hs-cTn elevation greater than the p99 can be seen without the presence of acute heart disease in men, the elderly, or patients with renal failure.1
The diagnosis of AMI caused by coronary atherothrombosis (type 1 AMI) requires, in addition to the characteristic hs-cTn pattern, a clinical context of acute ischemia defined by symptoms, ECG, imaging tests, or coronary angiography.8 As mentioned above, as a precaution, there is a tendency to overdiagnose type 1 AMI, a situation that causes consultations with cardiology services, the establishment of powerful antithrombotic treatments, and cardiac catheterizations. All of this may be unnecessary in some patients.5
It can be difficult to distinguish among type 1 AMI, type 2 AMI, and nonischemic myocardial injury. The clinical context is fundamental for the differential diagnosis. In type 2 AMI, the myocardial ischemia is not due to the rupture of atheromatous plaques in the coronary arteries, but to an imbalance between the myocardial oxygen supply and demand. It can occur in a variety of conditions, which are generally highly evident, both cardiac (eg, acute heart failure or tachyarrhythmias) and extracardiac (eg, severe anemia or respiratory failure). Nonischemic myocardial injury can also occur due to cardiac (myocarditis, tako-tsubo syndrome) or extracardiac (sepsis, renal failure) causes. Because it is difficult to properly classify diagnoses, there is wide variation among studies in the proportion of patients with type 1 AMI, type 2 AMI, or nonischemic myocardial injury treated in emergency departments. The distinction among the 3 diagnoses is critical because type 2 AMI and nonischemic myocardial injury require treatment of the disease causing the myocardial injury, which is different from the treatment of type 1 AMI. Finally, it should be noted that any elevation in cTn is associated with a poor prognosis, particularly in type 2 AMI and nonischemic myocardial injury, which also highlights the usefulness of hs-cTn in these different scenarios of type 1 AMI.10,11
Because it identifies more patients as potentially having type 1 AMI, hs-cTn can be a”false friend”. These patients require careful clinical evaluation before their diagnosis. The keys to ruling out a type 1 AMI are: a) absence of clinical, electrocardiographic, or, eventually, echocardiographic data indicating this type of AMI; and b) the identification of a possible cause of type 2 AMI or myocardial injury. Unfortunately, hs-cTn itself contributes little information to this final diagnosis. The absolute concentrations of cTn tend to be higher in type 1 AMI than in type 2, but the magnitude of the Δhs-cTn does not allow the types of AMI to be distinguished.12,13 The 0-, 0- to 1-, and 0- to 2-hour hs-cTn algorithms define, together with the exclusion criteria of the AMI, confirmation criteria for AMI based on the initial hs-cTn value and after 1, 2, or 3hours (Table 1).7 Although its positive predictive value is not optimal (around 75%) for the diagnosis of type 1 AMI, the algorithms are still useful for stratifying the risk of cardiovascular and noncardiovascular complications because most patients with criteria confirming AMI that are not type 1 are also at high risk of type 2 AMI or nonischemic myocardial injury. Nonetheless, they leave the problematic final diagnosis and the treatment plan to the discretion of the cardiologist. In addition, in all of the algorithms, there is a gray area that includes patients with hs-cTn concentrations between those excluding and confirming AMI. In these patients, a longer observation period or noninvasive tests are recommended for the final diagnosis. This gray area would contain patients with unstable angina or type 1 AMI with a small hs-cTn elevation, among others.
HIGH-SENSITIVITY TROPONIN IN CHRONIC DISEASESIn patients with chronic cardiac and extracardiac diseases, hs-cTn can be chronically elevated, as well as in asymptomatic individuals with high cardiovascular risk.8,14,15 These increases involve a wide variety of mechanisms, such as chronic ischemia, myocardial injury secondary to catecholamines or endotoxins, apoptosis, ventricular wall stress, and conditions that increase myocardial oxygen demand. In all of these situations, the hs-cTn elevation is a risk marker for both cardiovascular and noncardiovascular complications. Chronic hs-cTn elevations, which are usually small in magnitude, generate confusion when these patients attend an emergency department for some reason and a high hs-cTn is detected without Δhs-cTn. The absence of a Δhs-cTn does not rule out acute myocardial injury, although it makes it more unlikely.9 The clinical context should be the key to the correct interpretation of the mechanism involved.
CONCLUSIONSDetermination of hs-cTn has improved the evaluation of chest pain and is, together with the clinical assessment, the best instrument to exclude ACS. However, it can generate diagnostic doubts when there are concentration increases that would have gone unnoticed with contemporary cTn, and these situations may force cardiologists to intervene to rule in or rule out type 1 AMI. In this scenario, the cardiologists and other specialists involved should trust their clinical judgment, beyond the simple hs-cTn criterion, for the correct diagnostic and therapeutic orientation of the patients.
CONFLICTS OF INTERESTThe institute of J. Sanchis (INCLIVA) has received donations from Biotronik, Prosmedica, and Bayer to support research. A. Alquézar-Arbé has received personal honoraria from Roche Diagnostics. J. Ordóñez-Llanos has received personal honoraria from BioMerieux, Roche Diagnostics, Thermo-Fischer, and Singulex Inc. A. Bardají has no conflict of interest to declare.
The authors would like to thank Eva Guillén and Oscar Miró for their excellent work in checking the article.