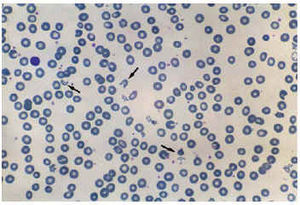
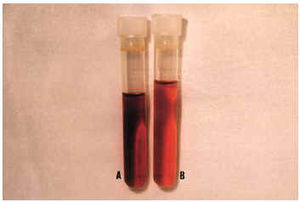
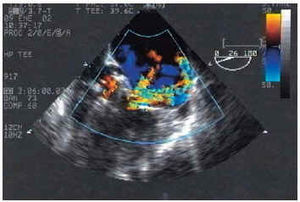
A 73-year-old woman was admitted for severe anemia 2 months after mitral and aortic cardiac valve replacement with Saint Jude mechanical prostheses. The differential blood count showed macrocytic anemia (hemoglobin 7.1 g/dL; MCV 111 fl; corrected reticulocyte count, 3.5%). The blood smear revealed marked anisopoikilocytosis, intense polychromasia, and abundant schistocytes (Figure 1, arrows). Total bilirubin was 1.76 mg/dL (indirect bilirubin, 1.36 mg/dL). LDH was markedly increased (5259 U/L) and haptoglobin reduced (6.0 mg/dL; normal, 100-300 mg/dL), which was compatible with intravascular hemolysis. The serum was brownish colored secondary to hemoglobinemia and the presence of methemalbuminemia, a product of erythrocyte fragmentation, which originates a characteristic color (Figure 2 A). The urine had a similar color (Figure 2 B). Transesophageal echocardiography revealed severe mitral periprosthetic regurgitation (Figure 3), as well as moderate aortic periprosthetic regurgitation.
Fig. 1.
Fig. 2.
Fig. 3.
Conservative treatment was attempted, but the patient required a large number of transfusions (more than 2 units of packed red blood cells per week), so surgical repair was decided on. Mitral and aortic cardiac valve replacement was performed with Carpentier-Edwards biological prostheses, with good results.
The most frequent causes of hemolytic anemia in patients undergoing valve replacement are mechanical trauma by disks to red blood cells and periprosthetic regurgitation. The treatment is generally medical, but surgical repair is required for periprosthetic regurgitation.