To the Editor,
A 41-year-old patient was referred to our center for ablation of accessory pathways (AP) in the context of Wolff-Parkinson-White (WPW) syndrome. The patient, who was still asymptomatic, had been diagnosed with WPW 9 years earlier in a routine examination. Three years before the present admission she began to refer to short episodes (<5min) of sudden-onset, sudden-offset palpitations, which were never recorded by electrocardiogram (ECG). In the past 9 months, she began to show signs of heart failure in the form of New York Heart Association functional class II effort dyspnea. Physical examination was normal, but during exercise testing she only achieved 6 METs. The ECG showed sinus rhythm with pre-excitation manifested by a right antero-septal AP suggesting a classic pattern of left bundle branch block (LBBB) (Figure 1A). Both echocardiography and magnetic resonance imaging (MRI) showed a marked intraventricular dyssynchrony, with early activation of the septum compared to the free wall and a mildly depressed ejection fraction (48%).
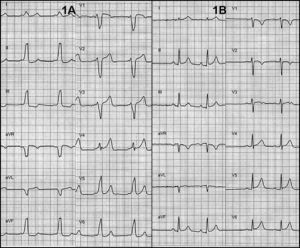
Figure 1. A: electrocardiogram showed a pattern of pre-excitation by a right antero-septal pathway suggesting a classic pattern of left bundle branch block. B: normalization of the electrocardiogram after ablation.
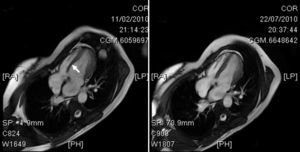
The patient remained asymptomatic after ablation. The ECG after ablation was strictly normal (Figure 1B). At 3 months after ablation, functional class was normal. An MRI 4 months after ablation showed normalization of the ejection fraction (63%) and absence of asynchrony (Figure 2).
Figure 2. Left: telesystolic image of the left ventricle, with a clear paradoxical septal movement (arrow) secondary to activation by a right septal accessory pathway. Right: normalization of the ejection fraction after ablation.
It has been reported that intraventricular dyssynchrony and subsequent systolic dysfunction due to early septal activation in patients with a right septal AP occur relatively frequently (in up to 50% of patients).1 In addition, some prospective studies have emphasized that dysfunction in the left ventricle can lead to its expansion over the long term.2 The incidence of asynchrony and its progression to ventricular dysfunction and myocardial dilatation may be underestimated in these patients as they generally undergo early ablation due to the presence of palpitations secondary to paroxysmal tachycardia, and these can occur before heart failure symptoms appear.1 For that reason, it has been suggested that right septal AP ablation should be carried out even before palpitations occur.3
It seems reasonable to rule out tachycardiomyopathy in this patient, as imaging techniques did not show ventricular growth and short episodes of tachycardia make this diagnosis unlikely.
Several studies have shown abnormalities in ventricular wall motion in patients with WPW syndrome.4, 5, 6 Left-sided pathways can produce premature anterior motion in the rear wall, while right septal APs can show motion abnormalities similar to those described in patients with LBBB.
In a recent study,3 a significant reduction in systolic function was observed in patients with right septal AP compared to patients with right or left free wall AP. Other series have confirmed that systolic function normalizes after ablation or spontaneous disappearance of preexcitation through the right septal pathways.7
This case illustrates how ventricular preexcitation through a right antero-septal AP can cause heart failure secondary to left ventricular dysfunction and intraventricular asynchrony, similar to the effect of LBBB. Ablation of the AP subsequently improved heart failure symptoms and normalized myocardial contractility.
Corresponding author: jmarti@parcdesalutmar.cat