It has been estimated that in 2017, 55 million people died worldwide, and that 17.7 million of these deaths were due to cardiovascular disease (CVD).1 Most of the epidemiological studies aiming to identify risk factors associated with death from CVD have been performed in high-income countries (HICs),2 yet nowadays most deaths from CVD occur in medium- (MICs) and low-income countries (LICs).1
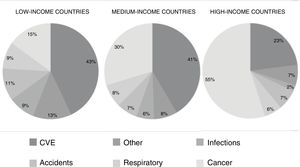
Recently,3,4 the morbidity and mortality results from the PURE (Prospective Urban Rural Epidemiology) study were published. This was a prospective, population-based cohort study that included individuals aged 35 to 70 years from 21 countries and 5 continents. The primary outcomes were the incidence of fatal and nonfatal CVD, cancer, injuries, respiratory disease, and hospital admissions. The study calculated the age- and sex-standardized incidence per 1000 person-years. Between January 2005 and December 2016, 162 534 participants were enrolled and were followed up for a mean of 9.5 years. Overall, there were 11 307 deaths (7%), 9329 cases (5.7%) of CVD, 5151 cases (3.2%) of cancer, 4386 cases (2.7%) of injury requiring hospitalization, 2911 cases (1.8%) of pneumonia, and 1830 cases (1.1%) of chronic obstructive pulmonary disease. CVD was higher in LICs (7.1 cases/1000 person-years) and MICs (6.8 cases/1000 person-years) than in HICs (4.3 cases/1000 person-years). Cancer, injuries, chronic obstructive pulmonary disease, and pneumonia were more common in HICs and less common in LICs. The overall mortality rate in the LICs (13.3 deaths/1000 person-years) was double that of MICs (6.9 deaths/1000 person-years) and 4 times that of HICs (3.4 deaths/1000 person-years). This pattern of higher mortality in LICs and lower mortality in HICs was observed for all causes of death except for cancer, which had a similar mortality rate in HICs, MICs, and LICs. CVD was the cause most common cause of death overall (40%), with wide variations depending on the country's income level: 23% of deaths in HICs, 41% in MICs and 43% in LICs, even though HICs had higher cardiovascular risk scores according to the INTERHEART scale. The proportion of deaths from CVD/cancer was 0.4% in HICs, 1.3% in MICs and 3.0% in LICs. Figure 1 shows cause of death by national income level according to the 2006 World Bank classification.
Yusuf et al.4 reported the associations and population-attributabe fractions (PAFs) of 14 modifiable CVD risk factors with overall mortality. These risk factors inlcuded behavioral factors (smoking, alcohol, diet, physical activity, and sodium intake), metabolic factors (hypertension [HTN], poorly-controlled blood sugar, diabetes, raised nonhigh-density lipoprotein cholesterol [non-HDLc], and abdominal obestity), psychosocial factors (education and symptoms of depression), grip strength, and ambient and household air pollution from the use of solid fuels such as wood or coal. The primary outcome was a composite of cardiovascualr events defined as cardiovascular death (acute myocardial infarction [AMI], cerebrovascular event [CVE], heart failure) and overall mortality. The study enrolled 155 722 participants with no past history of CVD, who were followed up for a mean of 9.5 years. Mean age was 50.2 years and 58.3% were women. There were 10 234 deaths, of which 2917 were due to CVD; 3559 participants had a nonfatal AMI and 3577 had a nonfatal CVE.
More than 70% of CVD was attributable to a small number of modifiable risk factors. Of these, HTN was the largest, representing more than 20% of the PAFs. Raised non-HDLc, household air pollution, smoking, poor diet, low educational level, abdominal obesity, and diabetes each represented between 5% and 10% of the PAFs, while low levels of physical activity, symptoms of depression, and excessive alcohol intake made a slight contribution to the development of CVD. Approximately two thirds of the deaths were due to noncardiovascular causes and most were associated with low educational level, smoking, poor diet, weak grip strength, ambient and household air pollution, HTN, and diabetes. The association between low educational level and CVD and overall mortality was stronger in HICs (which included the 4 South American countries that participated in the study: Argentina, Brazil, Chile, and Colombia) and in the LICs, possibly related to the greater inequality between people with high and low educational levels in the poor countries, and persisted after adjustment for healthy behaviors, with a stronger association than that observed for financial income. Education level affects conditions such as the home, work, diet, and access to health and recreational services; it is therefore suggested that greater investment in education would have beneficial effects on the prevention of CVD and overall mortality.
Weak grip strength is a risk factor for overall mortality and CVD comparable to other conventional risk factors, especially in MICs and LICs. We previously demonstrated that low muscle strength is a risk factor in the general population5 and in diabetic patients,6 and we proposed that this risk factor begins in-utero and is associated with the quality of maternal nutrition.7 Low birth weight for gestational age is known to be a major risk factor for subsequent CVD, associated with lower weight and muscle strength.8 Therefore, in MICs and LICs, one of the actions that should be taken to prevent CVD in the long-term is to develop a good prenatal monitoring system that ensures a healthy maternal diet during pregnancy.
In HICs, modifiable factors are present in around 70% of CVD, the most significant ones being metabolic factors and smoking. In MICs, they also occur in around 70%, the most significant being HTN and low educational level, but also abdominal obesity, raised non-HDLc and smoking. However, in LICs, modifiable factors are present in around 80% of CVD, the most significant being metabolic factors, air pollution, especially in the home, and poor diet. Regarding overall mortality, modifiable risk factors are present in 65% of all deaths in HICs, 70% in MICs and 80% in LICs; smoking is the predominant factor in HICs, followed by HTN and abdominal obesity. As for MICs and LICs, the modifiable risk factors for overall mortality were low educational level, weak grip strength, poor diet, and air pollution. These results highlight the need to make changes to socioeconomic models to increase educational levels and improve diet and air quality, particularly in the home—actions that go beyond the scope of the health sector and require the involvement of all social stakeholders.
The health sector must increase awareness and improve diagnosis, treatment, and control of HTN and atherogenic dyslipidemia, factors that can be controlled with pharmacological interventions with demonstrated effectiveness in reducing CVD mortality in studies such as HOPE-3,9–11 which included 12 500 patients, 28% of whom were South American, and the HOPE-4 study, with more than 1300 hypertensive patients from Colombia and Malaysia.12
The HOPE-3 study included patients with no past history of CVD with moderate cardiovascular risk, who took 2 antihypertensive medications at fixed doses (candesartan 16 mg/d plus hydrochlorothiazide 12.5 mg/d) and rosuvastatin (10 mg/d). The antihypertensives reduced cardiovascular events only in the group in the highest third for systolic blood pressure (SBP) (> 143.5 mmHg; mean, 154 mmHg), had a neutral effect in the middle third (131.6-143.5 mmHg; mean, 138 mmHg), and showed a tendency to increase events in the lowest third for SBP (< 131.6 mmHg; mean, 122 mmHg).9 These results were taken into account in making the recommendation of fixed-dose combined treatment only for patients with SBP > 140 mmHg in the Latin American guidelines on the management of HTN.13
Administration of rosuvastatin reduced low-density-lipoprotein cholesterol (LDLc) by 34.6 mg/dL (27%) and the relative risk (RR) of cardiovascular events by 25%. These effects were independent of the baseline values of LDLc, SBP, INTERHEART score, high-sensitivity C-reactive protein, and ethnicity. There was no increase in rhabdomyolysis, myopathy, or new cases of diabetes,10 findings that are important for South American countries in which the prevalence of dyslipidemia among adults older than 35 years is very high.14 The concurrent administration of the 2 treatments produced a 30% reduction in the RR of major cardiovascular events, and a 40% reduction in individuals in the highest third for SBP.11
In conclusion, it appears that it would be beneficial to implement public health programs to guarantee the availability of these medications, as well as access and adherence to them, for all individuals older than 55 years with hypertension and abdominal obesity. If the SBP is < 140 mmHg, only the statin should be prescribed.
The HOPE-4 trial,12 carried out in Colombia and Malaysia, demonstrated the efficacy of a new, community-based health care model, to improve current suboptimal control of HTN with monitoring and treatment. The trial included 1371 patients with HTN from 30 urban and rural communities: 15 were followed up using the new model and 15 using the standard model. The study identified that the 3 main barriers to controlling HTN (< 140/80 mmHg) were the cost of transport to the health center, copayment for prescribed medications, and the time spent in the health center. A strategy was implemented based on home monitoring visits with nursing auxiliaries who were chosen to ensure that they lived in the districts where the study was conducted. They were trained using a program developed by the World Health Organization, and given a tablet device containing recommended treatment algorithms, including any potential adverse events. These nursing auxiliaries made a monthly free delivery of a fixed dose of candesartan 16mg/d, amlodipine 5mg/d, and rosuvastatin 10 mg/d. A relative or friend was appointed to encourage adherence to the recommended lifestyle changes: healthy diet, smoking cessation, avoiding excess alcohol, increasing physical activity, and avoiding excessive weight gain. HTN control improved from 30% in the communities with standard care up to 69% in the group with the community-based strategy, Framingham score decreased 40%, and there was a greater reduction in LDLc, as well as an increase in physical activity and intake of fruit and vegetables.
These results confirm that access to medications is crucial and is affected by social inequality as measured with the Wagstaff concentration index, which uses a scale from −1 (pro-poor) to 1 (pro-rich), corrected for age and sex. Among the 8492 individuals from the PURE study that had had a cardiovascular event, the use of proven effective medications as secondary prevention (antiplatelet agents, statins, and antihypertensives) ranged from 0% in South Africa (96% confidence interval [95% CI], 0-0.7), Tanzania (95% CI, 0-3.6) and Zimbabwe (95% CI, 0-5.1), to 49.3% in Canada (95% CI, 44.4-54.3). The proportion of patients who received at least 1 medication ranged from 2.0% (95% CI, 0.5-6.9) in Tanzania to 91.4% (95% CI, 86.6-94.6) in Switzerland. There was significant pro-rich inequality (P <0.05) in Saudi Arabia, China, Colombia, India, Pakistan, and Zimbabwe, and public spending on health was the best predictor of inequality.15
A specific analysis in South America16 demonstrated that, of the 910 people who had experienced an AMI, only 30.1% were taking aspirin; 34.2%, beta-blockers; 36%, an angiotensin-converting enzyme-inhibitor (ACE-I) or angiotensin II receptor blocker (ARB), and 18%, statins. Of the 407 that had experienced a CVE, only 24.3% were taking aspirin; 37.6%, an ACE-I/ARB, and 9.8%, statins. Of the individuals with a previous AMI, 31% were not taking any medication; in patients with a previous CVE, 54% were not taking any medication. Only 7.4% of patients with a history of CVE were receiving 3 or more of the effective medications for secondary prevention; the most important factor was socioeconomic level, as the people with the fewest resources were those that were taking fewest medications. Of the 4 South American counties, Colombia had the worst figures: 48% of patients with a history of AMI and 66% of patients with a history of CVE were taking no medications. The use of beta-blockers in patients with a previous AMI ranged from 22% in Colombia to 42.5% in Argentina, and the use of ACE-I/ARB, from 29.1% in Colombia to 45.6% in Brazil. Statin use ranged from 2.2% in Colombia to 30.3% in Brazil. Aspirin was the most-used drug, ranging from 25.9% in Argentina to 48.3% in Chile. Of the patients with previous CVE, only 24.3% were receiving aspirin; 37.6%, ACE-I; and 9.8%, statins.
CONCLUSIONSThe results from the large international epidemiological and clinical studies that we have reviewed demonstrate that, while in HICs cancer has replaced CVD as the leading cause of death, in MICs and LICs, CVD remains the leading cause of morbidity and mortality. In LICs and MICs, the main risk factors identified for death from any cause and CVD are low educational level, HTN, and factors linked to socioeconomic status, such as poor diet and household pollution due to the use of solid fuels. In HICs, the main risk factors are smoking, HTN, and high levels of non-HDLc. Therefore, preventative strategies must be adapted to each country according to their socioeconomic conditions: in LICs and MICs, investment is required to improve education levels, reduce poverty, improve diet, and replace solid fuels for cooking in the home with less polluting fuels such as electricity or gas. However, universal interventions are also required, such as improving the availability of and access to antihypertensive medications and statins, drugs that have been proven to be effective in reducing cardiovascular risk in hypertensive populations with moderate risk. Innovative, community-based strategies must also be considered, which include the identification of barriers, specific to each country, that prevent adequate control of metabolic risk factors, the participation of nonphysician health care workers, and the use of simplified, standardized algorithms for proven effective pharmacological treatments in primary and secondary prevention.
FUNDINGPopulation Health Research Institute (PHRI), Hamilton, Canada, and Secretaría de Salud de Santander and COLCIENCiAS, Colombia. Grant n.° 651777758228.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.