There are no nationwide, population-based studies in Spain assessing overall cardiovascular risk. We aimed to describe cardiovascular risk and achievement of treatment goals following the 2012 European Guidelines on cardiovascular disease prevention strategy. We also investigated clinical characteristics (non-classical risk factors) associated with moderate risk.
MethodsParticipants (n=2310, 58% women) aged 40 to 65 years from a national population-based study (Di@bet.es Study) were identified. First, a priori high/very-high risk individuals were identified. Next, total cardiovascular risk (Systematic Coronary Risk Evaluation equation including high-density lipoprotein cholesterol) was used to assess risk of a priori non-high risk individuals. Variables independently associated with moderate versus low-risk were investigated by multiple logistic regression analysis.
ResultsAge-and-sex standardized (direct method) percentages of high/very-high, moderate, and low-risk were 22.8%, 43.5%, and 33.7%, respectively. Most men were at moderate (56.2%), while 55.4% of women were at low risk. Low-density lipoprotein cholesterol (< 70,<100, < 115mg/dL) and blood pressure (<140/90mmHg) goals for very-high, high and moderate risk were met in 15%, 26% and 46%, and 77%, 68% and 85% of the individuals, respectively. Body mass index, high triglycerides concentrations, diastolic blood pressure, and low Mediterranean diet adherence (in women) were independently associated with moderate (versus low) risk.
ConclusionsCardiovascular risk in Spain is mainly moderate in men and low in women. Achievement of treatment goals in high-risk individuals should be improved. The prevalence of non-classical cardiovascular risk factors is elevated in subjects at moderate risk, an important aspect to consider in a population-based strategy to decrease cardiovascular disease in the most prevalent group.
Keywords
Although the incidence of coronary and cerebrovascular disease mortality has declined during recent decades, cardiovascular disease (CVD) is still the leading cause of death and disability in Spain, as well as in the other European countries.1,2 Our current strategy for CVD prevention at the population level is based on multifactorial risk assessment to target interventions accordingly.3 In Spain, the Spanish Committee for Cardiovascular Disease Prevention and the Spanish Society of Cardiology recommend the use of the Systematic Coronary Risk Evaluation (SCORE).4 However, calculation of cardiovascular risk (CVR) based on a calibrated Framingham scale by REGICOR (Registre Gironí del Cor) is also a popular strategy used in Spain.5,6
Relative risk of CVD is higher in high-risk individuals compared with those at low/moderate risk. However, nearly 90% of the population belongs to the latter group, and consequently most of the cardiovascular events (55%-80%) occur in low/moderate risk individuals.7,8 Therefore, additional clinical information is usually gathered to better identify low and, especially, moderate-risk individuals in whom a more aggressive intervention could be considered to improve their risk profile and to reduce the incidence of CVD.9
In Spain, there are only a few studies designed to describe CVR at the population level.10–17 These studies are either limited by their sample size, or focused on specific groups with at least one of the classical cardiovascular risk factors (CVRF), or performed in specific regions that may not be representative of the entire country. Furthermore, none of these surveys included high-density lipoprotein cholesterol (HDL-C) in the estimation of CVR. Therefore, we aimed to describe the situation of CVR in Spain in a population-based study, the Di@bet.es Study,18 following the stepped approach suggested in the European Guidelines on cardiovascular disease prevention in clinical practice.3 We also describe the prevalence and level of control of traditional (and nontraditional) risk factors, the achievement of treatment goals according to CVR, and the clinical characteristics (non-classical CVRF) associated with moderate risk. Finally, we evaluated the degree of concordance between the European Guideline strategy (which includes the SCORE equation) and the Framingham-REGICOR strategy.
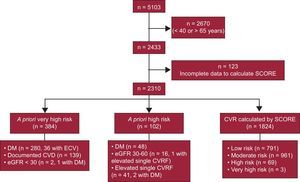
METHODSPopulationThe Di@bet.es Study18 was a national, cross-sectional, population-based survey conducted in 2009-10. A cluster (n=100 primary care centers) sampling design was used to select participants, forming a representative random sample of the Spanish population. Of the eligible adults, 55.8% attended for examination, of whom 9.9% were excluded by protocol (institutionalized, severe disease, pregnancy or recent delivery) giving a final sample of 5072 individuals aged ≥ 18 years (41.6% men and 58.4% women). Individuals (n=2310, 58% women) aged between 40 and 65 years (the age limitation of SCORE equation) from the final sample were selected to estimate their CVR (Figure 1). The study was approved by the Ethics and Clinical Investigation Committee of the Carlos Haya Hospital, and written informed consent was obtained from all participants.
Variables and ProceduresBriefly, participants were invited to attend a single examination visit at their primary health care center. Information was collected using a structured, interview-administered questionnaire followed by a physical examination. Personal history of hypertension, dyslipidemia, or CVD (coronary, cerebrovascular, or peripheral) was recorded, as well as the medications participants were taking.19 Age, sex, education level (no studies, elementary, secondary, technical school or university graduate), marital status (single, divorced, married or living together as a couple, or widowed) and smoking habits were also recorded. Adherence to a Mediterranean diet was assessed as previously described.20 The physical activity was estimated with the IPAQ-SF (Short Form of the International Physical Activity Questionnaire).21 Weight, height, and waist and hip circumferences were directly measured by the research nurses using standardized methods. Blood pressure was measured using a blood pressure monitor (Hem-703C, Omron; Barcelona, Spain) after several minutes in a seated position; the mean of two measurements taken 1 to 2minutes apart was used. After the interview, a fasting blood sample was obtained and a standard oral glucose tolerance test (in nondiabetics) performed. Serum glucose, triacylglycerols, and cholesterol were measured enzymatically, and HDL-C by direct method. Low-density lipoprotein cholesterol (LDL-C) was estimated by the Friedewald formula. Atherogenic dyslipidemia was defined as triglycerides > 150mg/dL and HDL-C < 40mg/dL for men and < 45mg/dL for women. The MDRD (Modification of Diet in Renal Disease) formula was used to estimate glomerular filtration rate.
Estimation of Cardiovascular RiskThe stepped approach suggested in the European Guidelines on cardiovascular disease prevention in clinical practice was used to estimate CVR in our cohort.3 Flowchart of study participants is shown in Figure 1. First, individuals with a priori very-high risk were identified (n=384): diabetes (n=280), either known diabetes (n=177) or diagnosed after the blood test (n=103), with one or more CVRF or microalbuminuria (> 20mg/L); chronic renal failure with estimated glomerular filtration rate ≤ 30ml/min; or documented CVD. From our questionnaire, 105, 42, and 12 individuals who had coronary heart, cerebrovascular, or peripheral vascular disease, respectively, were identified. Overall, 139 (6.02% total, 3.42% women, 9.63% men) participants had CVD. This prevalence was similar to the one reported in previous studies in a population with similar (35-64 years) age range (6.4% all, 3.9% women and 9.2% men).22 Second, we identified individuals with a priori high risk (n=102): diabetes (n=48), either known diabetes (n=34) or diagnosed after the blood test (n=14) without other CVRF and without microalbuminuria; estimated glomerular filtration rate between 30 to 60ml/min; total cholesterol > 8 mmol/L, systolic blood pressure ≥ 180mmHg, or diastolic blood pressure ≥ 110mmHg. For the remaining participants (n=1824), total CVR was estimated with the current version of the SCORE equation for low-risk regions, which includes HDL-C.23 Finally, very-high (a priori very-high risk or SCORE ≥ 10%), high (a priori high risk or SCORE 5%-10%), moderate (non-high risk and SCORE 1%-5%), and low (non-high risk and SCORE ≤ 1%) risk categories were defined. The LDL-C goals according to estimated CVR were defined as: < 130mg/dL in low, < 115mg/dL in moderate, < 100mg/dL in high and < 70mg/dL in very-high risk individuals.3
Similarly, CVR was estimated by means of the Framingham-REGICOR strategy.5 According to this, individuals with documented CVD were classified as very-high risk, while those with one or more markedly elevated risk factors (total cholesterol > 8 mmol/L, systolic blood pressure ≥ 180mmHg or diastolic blood pressure ≥ 110mmHg) as high risk. For the remaining, total CVR was estimated with the latest (which also includes HDL-C) Framingham-REGICOR equation,5 with values ≥ 15% representing very-high, 10-15% high, 5-10% moderate and < 5% low risk.
Statistical AnalysisData are presented as median [interquartile range] and number of individuals (percentage) unless otherwise indicated. To estimate total CVR in Spain, standardized rates (× 100 population) of risk categories (low/moderate/high/very-high) were calculated using the direct method described in Armitage et al.24 The age and sex structure of the Spanish population (INE [Instituto Nacional de Estadística], 2010) was used as the standard population. Therefore, our age- and sex-adjusted rates are the rates that would occur if the observed age- and sex-specific rates in the Di@bet.es study population were present in a population with the age and sex distribution of the standard (INE, 2010) Spanish population. The kappa coefficient was used to examine the agreement between CVR strategies (European Guidelines on cardiovascular disease prevention in clinical practice ans Framingham-REGICOR) in the classification of the participants as very high/high risk vs non–high-risk (moderate/low risk). Differences in age, sex, anthropometric variables, lifestyle, sociodemographic variables, other CVRF, active medications, lipid parameters, and estimated glomerular filtration rate across the different categories of CVR were evaluated by means of chi-square or Kruskal-Wallis tests as appropriate. Logistic multiple regression analysis was used to investigate CVRF not included in the SCORE equation (ie, non-classical risk factors) that were independently associated with moderate risk (vs low risk). Because most of these factors are age- and sex-dependent, a stepwise multiple logistic regression model adjusted for age, and separate for each sex, was built to investigate variables associated with the moderate risk category. Predictive performance of these models was evaluated by area under the receiver operating characteristic curve and Hosmer-Lemeshow goodness-of-fit test. The significance level was set at P ≤ .05. Analyses were performed with SAS software, v.9.2 (SAS Institute Inc.; Cary, North Carolina, United States).
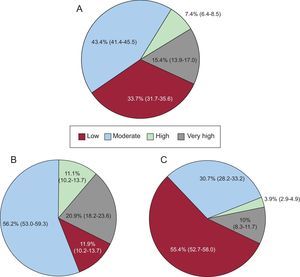
RESULTSPrevalence of Cardiovascular Risk CategoriesIn individuals aged 40 to 65 years, CVR estimated by the European Guidelines on cardiovascular disease prevention in clinical practice is mainly moderate (43.4%; 95%CI, 41.4-45.5), and the prevalence of very-high risk is > 15% (Figure 2). Sex differences were found in the SCORE (P<.0001). In men, 56% and 32% were in moderate and high/very-high risk categories, respectively. However, most of the women (55%) were in the low-risk category and only 4% and 10% of them were at high or very-high risk, respectively. Furthermore, diabetes accounted for a large percentage of the high (25% and 35%) and, especially, very-high (60% and 69%) risk categories in men and women, respectively.
Cardiovascular risk estimated by the European Guidelines on cardiovascular disease prevention in clinical practice strategy in population aged 40 to 65 years adjusted to the age and sex structure of the Spanish population (A), men (B) and women (C). Data are shown as percentage and 95% confidence interval.
Because individuals with diabetes are a priori defined as a high/very-high risk in the European Guidelines on cardiovascular disease prevention in clinical practice, but not in Framingham-REGICOR, which includes specific risk estimates for these individuals, we first investigated risk concordance in individuals with diabetes.5 Participants with diabetes (n=331; 14%) were categorized in the high (n=48; 15%) or very high (n=283; 85%) risk category by the European Guidelines on cardiovascular disease prevention in clinical practice and in the low (n=55, 18%), intermediate (n=130; 43%), high (n=54; 18%), or very high (n=66; 22%) risk category by Framingham-REGICOR. Thereafter, concordance was evaluated in nondiabetic individuals (Tables 1 and 2 of the supplementary material), and because one of the main goals of the CVR prevention strategy is to identify high-risk individuals, our nondiabetic population was dichotomized: individuals at high/very high and at low/moderate risk. After excluding individuals with diabetes, there was a substantial agreement (κ=0.77 [0.73-0.82]) between European Guidelines on cardiovascular disease prevention in clinical practice and Framingham-REGICOR strategies (Table 1). Kappa coefficient was slightly higher for the European Guidelines vs Framingham-REGICOR concordance in women (κ=0.82 [0.75-0.90]) than in men (κ=0.74 [0.67-0.80]) (Table 1).
Concordance of Estimated Cardiovascular Risk Between Registre Gironí del Cor and Systematic Coronary RisK Evaluation in Nondiabetic Population
| Whole sample (n=1979) | |||
|---|---|---|---|
| REGICOR | |||
| Low/moderate risk (n=1819) | High/very high risk (n=160) | ||
| SCORE | Low/moderate risk (n=1752) | 1746 (88.2) | 6 (0.3) |
| High/very high risk (n=227) | 73 (3.7) | 154 (7.8) | |
| Males (n=764)a | |||
|---|---|---|---|
| REGICOR | |||
| Low/moderate risk (n=657) | High/very high risk (n=107) | ||
| SCORE | Low/moderate risk (n=609) | 604 (79.1) | 5 (0.7) |
| High/very high risk (n=155) | 53 (6.9) | 102 (13.4) | |
| Females (n=1215)b | |||
|---|---|---|---|
| REGICOR | |||
| Low/moderate risk (n=1162) | High/very high risk (n=53) | ||
| SCORE | Low/moderate risk (n=1143) | 1142 (94) | 1 (0.08) |
| High/very high risk (n=72) | 20 (1.7) | 52 (4.3) | |
REGICOR, Registre Gironí del Cor; SCORE; Systematic Coronary RisK Evaluation.
Data are expressed as No. (%) of individuals included in each category.
Although the proportion of individuals on lipid-lowering, antihypertensive, and antiplatelet drugs increased with increasing risk (all P<.0001), the proportion of those with LDL-C meeting goals or with blood pressure ≤ 140/90mmHg decreased with increasing risk (P<.0001) (Table 2). Only the proportion of individuals with blood pressure ≤ 140/90mmHg was higher (P=.029) among very-high as compared with high-risk individuals, even after adjustment for antihypertensive medication (P=.003). Although the proportion of individuals at very-high risk with LDL-C<70mg/dL was very low, this proportion increased to 47% when LDL-C < 100mg/dL was the cut-off point. Similarly, the proportion of individuals at high or moderate risk with LDL-C < 130mg/dL was 63% and 69%, respectively. Approximately, one in three (28%-34%) people in moderate, high, and very-high risk categories were smokers (Table 2).
Treatment Goals According to Estimated Cardiovascular Risk
| Low risk (n=791) | Moderate risk (n=961) | High risk (n=171) | Very high risk (n=387) | P | |
|---|---|---|---|---|---|
| LDL-C | |||||
| LDL-C, mg/dL | 104 [85-104] | 118 [99-137] | 118 [99-147] | 102 [83-120] | < .0001 |
| Lipid-lowering treatment | 26 (3.3) | 138 (14.3) | 18 (10.5) | 162 (42) | < .0001 |
| LDL-C meeting goals | 645 (81.5) | 444 (46.2) | 44 (25.9) | 57 (14.7) | < .0001 |
| Blood pressure | |||||
| SBP, mmHg | 120 [110-129] | 134 [123-144] | 148 [133-164] | 140 [127-152] | < .0001 |
| DBP, mmHg | 74 [68-80] | 80 [74-86] | 84 [78-91] | 82 [74-90] | < .0001 |
| Antihypertensive | 49 (6.2) | 216 (22.5) | 50 (29.2) | 239 (61.8) | < .0001 |
| BP < 140/90 | 764 (96.6) | 814 (84.7) | 116 (67.8) | 299 (77.2) | < .0001 |
| Smoking status | |||||
| Current smokers | 128 (25) | 296 (30.8) | 58 (33.9) | 107 (27.7) | .021 |
| Antiplatelet drugs | 6 (0.8) | 18 (1.9) | 8 (4.7) | 108 (28) | < .0001 |
BP, blood pressure; DBP, diastolic blood pressure; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure.
Low-density lipoprotein cholesterol goals according to estimated cardiovascular risk were defined as: < 130 mg/dL for low-risk individuals; < 115 mg/dL moderate-risk individuals; < 100 mg/dL for high-risk individuals, and < 70 mg/dL for very high-risk individuals, respectively.
Data are expressed as median [interquartile range] or No. (%).
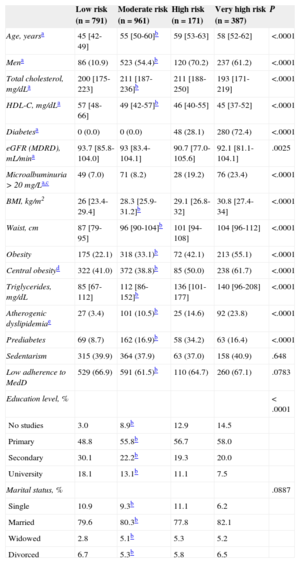
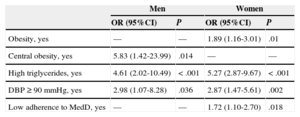
In Table 3, age, sex and several traditional and nontraditional CVRF (which are not a core part of the risk-stratification strategy) are presented by CVR categories. Most, but not all (such as sedentarism and estimated glomerular filtration rate), of the variables shown in Table 3 differed between low and moderate risk individuals. In a stepwise multiple logistic regression model, we found that body mass index (in women), central obesity (in men), diastolic blood pressure, high triglycerides, and low adherence to a Mediterranean diet (in women) were factors associated with moderate risk category (Table 4). This model had good fit based on nonsignificance on the goodness-of-fit Hosmer-Lemeshow test (P=.13 and P=.99 for women and men, respectively, and area under the receiver operating characteristic curves (0.96; 95%CI, 0.95-0.97, and 0.95; 95%CI, 0.93-0.97 for women and men, respectively) indicated good accuracy of predictive models.
Distribution of Other Classical or Non-classical Cardiovascular Risk Factors According to Estimated Cardiovascular Risk
| Low risk (n=791) | Moderate risk (n=961) | High risk (n=171) | Very high risk (n=387) | P | |
|---|---|---|---|---|---|
| Age, yearsa | 45 [42-49] | 55 [50-60]b | 59 [53-63] | 58 [52-62] | <.0001 |
| Mena | 86 (10.9) | 523 (54.4)b | 120 (70.2) | 237 (61.2) | <.0001 |
| Total cholesterol, mg/dLa | 200 [175-223] | 211 [187-236]b | 211 [188-250] | 193 [171-219] | <.0001 |
| HDL-C, mg/dLa | 57 [48-66] | 49 [42-57]b | 46 [40-55] | 45 [37-52] | <.0001 |
| Diabetesa | 0 (0.0) | 0 (0.0) | 48 (28.1) | 280 (72.4) | <.0001 |
| eGFR (MDRD), mL/mina | 93.7 [85.8-104.0] | 93 [83.4-104.1] | 90.7 [77.0-105.6] | 92.1 [81.1-104.1] | .0025 |
| Microalbuminuria > 20 mg/La,c | 49 (7.0) | 71 (8.2) | 28 (19.2) | 76 (23.4) | <.0001 |
| BMI, kg/m2 | 26 [23.4-29.4] | 28.3 [25.9-31.2]b | 29.1 [26.8-32] | 30.8 [27.4-34] | <.0001 |
| Waist, cm | 87 [79-95] | 96 [90-104]b | 101 [94-108] | 104 [96-112] | <.0001 |
| Obesity | 175 (22.1) | 318 (33.1)b | 72 (42.1) | 213 (55.1) | <.0001 |
| Central obesityd | 322 (41.0) | 372 (38.8)b | 85 (50.0) | 238 (61.7) | <.0001 |
| Triglycerides, mg/dL | 85 [67-112] | 112 [86-152]b | 136 [101-177] | 140 [96-208] | <.0001 |
| Atherogenic dyslipidemiae | 27 (3.4) | 101 (10.5)b | 25 (14.6) | 92 (23.8) | <.0001 |
| Prediabetes | 69 (8.7) | 162 (16.9)b | 58 (34.2) | 63 (16.4) | <.0001 |
| Sedentarism | 315 (39.9) | 364 (37.9) | 63 (37.0) | 158 (40.9) | .648 |
| Low adherence to MedD | 529 (66.9) | 591 (61.5)b | 110 (64.7) | 260 (67.1) | .0783 |
| Education level, % | < .0001 | ||||
| No studies | 3.0 | 8.9b | 12.9 | 14.5 | |
| Primary | 48.8 | 55.8b | 56.7 | 58.0 | |
| Secondary | 30.1 | 22.2b | 19.3 | 20.0 | |
| University | 18.1 | 13.1b | 11.1 | 7.5 | |
| Marital status, % | .0887 | ||||
| Single | 10.9 | 9.3b | 11.1 | 6.2 | |
| Married | 79.6 | 80.3b | 77.8 | 82.1 | |
| Widowed | 2.8 | 5.1b | 5.3 | 5.2 | |
| Divorced | 6.7 | 5.3b | 5.8 | 6.5 |
BMI, body mass index; eGFR, estimated glomerular filtration rate; HDL-C, high-density lipoproteins cholesterol; MDRD, Modification of Diet in Renal Disease; MedD, Mediterranean diet.
Unless otherwise indicated, data are expressed as No. (%) or median [interquartile range].
Multiple Logistic Regression Analysis to Identify Variables Associated With Moderate Versus Low Risk
| Men | Women | |||
|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | |
| Obesity, yes | — | — | 1.89 (1.16-3.01) | .01 |
| Central obesity, yes | 5.83 (1.42-23.99) | .014 | — | — |
| High triglycerides, yes | 4.61 (2.02-10.49) | <.001 | 5.27 (2.87-9.67) | <.001 |
| DBP ≥ 90mmHg, yes | 2.98 (1.07-8.28) | .036 | 2.87 (1.47-5.61) | .002 |
| Low adherence to MedD, yes | — | — | 1.72 (1.10-2.70) | .018 |
95%CI, 95% confidence interval; DBP, diastolic blood pressure; MedD, Mediterranean diet; OR, odds ratio.
Variables included in the model: age, obesity (body mass index ≥ 30kg/m2), central obesity (waist/hip ratio > 1 in men and > 0.85 in women), high triglycerides (> 150mg/dL), Mediterranean diet (lower vs medium/higher tertile) adherence, diastolic blood pressure, physical activity (inactive vs active), university education, civil status, and prediabetes (yes vs no).
Multiple logistic regression model (stepwise), value of significance level for entry P<.15.
The Di@bet.es study18 was designed to determine the prevalence of diabetes and other CVRF in a representative sample of the population of Spain. The CVR in population aged 40 to 65 years in Spain is, according to our results, moderate (43.4%), with 22.8% of the population at high/very-high risk. After excluding individuals with a priori defined high/very-high risk, less than 5% of the population was classified in these categories. Indeed, only 40% and 0.8% of the high and very-high risk individuals were identified by calculating total CVR with the SCORE equation. To the best of our knowledge, this is the first population-based probability sample study of the entire country (Spain) evaluating CVR with the stepped European Guidelines on cardiovascular disease prevention in clinical practice strategy and including HDL-C in the risk equation. Most of the previous studies investigating CVR in Spain were focused on patients with prespecified medical conditions (metabolic syndrome, or presence of one or more traditional risk factors)12,13 or were limited to regions that might not be representative of the whole national territory.10–12,14–16 Moreover, none of them included individuals with documented CVD or considered HDL-C in the risk equation, and only some included diabetic patients.10,11,13,16,17
Sex differences in CVR in Spain have been reported in previous studies. Jansen-Chaparro et al12 and Mostaza et al14 showed that the prevalence of high/very-high risk in men and women was 6.9% and 0.5%, and 8.2% and 0.2%, respectively. In our survey, in a population aged 40 to 65 years, the overall prevalence of high/very-high risk in men was more than double that of women (32% vs 13.9%, Figure 2), and after excluding individuals with a priori high or very-high risk, this prevalence was 10.3% and 0.1%, respectively, which is similar to that reported in previous studies.12,14 Although male sex is a well-established CVRF and lifelong risk for CVD is higher in men than in women,25 in Spain, according to the European Heart Network,26 the percentage of deaths from CVD is higher in women compared with men, 35% vs 27%, respectively. Furthermore, in a cohort of 3856 individuals with a mean follow-up of 7.1 years, more than 80% of total cardiovascular events occurred in women who were classified at baseline as low or moderate risk, compared with 55% in men with the same risk.7 These data and the high percentage of women currently classified as low/moderate risk in our, and other, studies indicate that the current strategy to assess CVR in females should be further improved. In addition, the efficacy of acetylsalicylic acid27 and statins28 in primary prevention is lower in women than in men, and women have a worse prognosis after some cardiovascular events compared to men.29 Thus, similar to what the American Heart Association has recently proposed,30 strategies specifically accounting for sex differences in CVR are also needed in European countries.
In Spain, several risk strategies are currently used to estimate CVR in different regions. Among these equations, SCORE and REGICOR are the most popular. It has been previously discussed that the former overestimates and the second underestimates CVR.31 More recently, Gil-Guillén et al11 assessed the agreement of these two equations in the identification of high-risk individuals among more than 8000 people without established CVD, and found low concordance between them (κ=0.463), where SCORE classified as high risk nearly twice as many people as Framingham-REGICOR. In our study, however, the two strategies had substantial (almost perfect for females) agreement when diabetes (a priori high or very-high risk condition for SCORE) was excluded (Table 1), and when situations such as total cholesterol > 8 mmol/L, systolic blood pressure ≥ 180mmHg, diastolic blood pressure ≥ 110mmHg, or documented CVD were a priori defined as high or very-high risk according to European Guidelines on cardiovascular disease prevention in clinical practice and Framingham-REGICOR strategies.5 Therefore, diabetes may be responsible for a large part of this disagreement. Indeed, we have reported how differently the strategies classified the risk of diabetic patients, with 61% of the high/very-high risk diabetic individuals (according to European Guidelines on cardiovascular disease prevention in clinical practice) classified as non-high risk by the Framingham-REGICOR strategy. Although diabetes is not a coronary risk equivalent in Spain,32 as well as in other countries,33 CVR in individuals with diabetes is more than double that of nondiabetics.34 Moreover, only multifactorial, early, and intensive intervention can delay or prevent cardiovascular mortality in patients with diabetes.35 Therefore, strategies failing to identify diabetes as a high-risk condition do not prompt physicians to achieve one of the most important components of this early and intensive intervention, ie, appropriate treatment of diabetic dyslipidemia. Tailored LDL-C goals are intentionally set at a lower range for individuals with diabetes to overcome the fact that LDL-C concentrations are only a marginal aspect in the evaluation of diabetic dyslipidemia.36
Despite the improvement observed in Spain in the control of hypertension or dyslipidemia during recent years, achievement of treatment goals in CVRF remains poor.37 Furthermore, prevalence of risk factors continues to increase, mainly due to an unhealthy lifestyle (sedentarism and inadequate food intake) and a high prevalence of obesity that in Spain is close to 30% according to the Di@bet.es Study.18 Indeed, if ideal cardiovascular health is evaluated in Spain, only 0.2% and 3.4% (3.2% in our study) of participants attained ideal values for 7 or 6 CVD health metrics, respectively.37 Notwithstanding, as reported in the EURIKA Study17, similar trends in control and prevalence of risk factors have been reported in other European countries, with less than 50% of individuals meeting primary prevention goals for blood pressure, lipids, and diabetes. Moreover, randomized clinical trials where secondary prevention is pursued in diabetic (and nondiabetic) individuals demonstrate that treatment goals are not met in a large proportion of this very-high risk population.38 In this sense, in our study, the prevalence and degree of control of classical or non-classical CVRF (Table 2) are poor, in agreement with previous studies.17,38 Only 15% or 47%, respectively of the very-high risk participants (mostly individuals with CVD or diabetes with multiple CVRF) met the proposed LDL-C goals (< 70 or < 100mg/dL, respectively); 23% had blood pressure > 140/90mmHg, and 28% were active smokers.
We were also interested in describing individuals at moderate risk. This is the group of individuals in whom, especially for women, most of the future cardiovascular events at the population level will occur.7 In our study, 54% and 33% of individuals in moderate risk had LDL-C > 115mg/dL (current target, European Guidelines on cardiovascular disease prevention in clinical practice3) or 130mg/dL (a less strict target), respectively. Furthermore, independently of their older age, other CVRF which are not part of the risk stratification strategy were more prevalent in this group, compared with the low-risk group. Hence, the presence of obesity or central obesity, atherogenic dyslipdemia, elevated diastolic blood pressure, or poor adherence to a healthy20 cardiovascular diet also could serve to guide the management of this critical risk group. In this regard, lifestyle interventions, which are not generally well implemented,17,20 are profoundly associated with these features (Table 4), are related to cardiovascular health and events, and (especially for diet) are in part responsible of the coronary heart disease paradox in Spain,39 should be pursued by health authorities in this group at moderate risk.
Strengths and LimitationsSeveral strengths and limitations should be acknowledged in this study. The main strength of the study is that it was intended to be representative of the whole national territory, has no prespecified limitations regarding participant inclusion criteria, and takes into account HDL-C to estimate CVR. The study, however, also has a few limitations. Since the calculation of total risk in the European Guidelines on cardiovascular disease prevention in clinical practice strategy is in part limited (SCORE equation restriction) to persons aged 40 to 65 years, our results does not represent CVR in people > 65 years. Inclusion of this older group would have a priori increased CVR. In addition, the information regarding prevalent CVD, although collected using a structured, standardized, interview-administered questionnaire, was self-reported: an otherwise usual practice in large epidemiological surveys. Finally, population-based studies, although less prone to referral bias, may include several inherent sources of selection and observation bias due to study design, type of sampling, participation rate40 (which was 55.8% in our study), or recall and interviewer bias.41
CONCLUSIONSIn summary, we present current information regarding CVR in a representative sample of the population of Spain. CVR in a population aged 40 to 65 years is mainly moderate in men and low in women, and a large proportion of high/very-high risk individuals do not meet appropriate treatment goals. Furthermore, the presence of other, so-called non-classical CVRF, specifically obesity and hypertriglyceridemia, is elevated in individuals at moderate risk. These data are relevant to public health authorities designing CVD prevention programs to promote, on one side, a better achievement of treatment goals in the high/very-high risk group, the one with higher incidence of cardiovascular events, and, on the other hand, a better identification of individuals (especially women) in the moderate-risk group, the group in which most cardiovascular events will occur.
CONFLICTS OF INTERESTNone declared.
This work would not have been possible without the help and support of the primary care managers and personnel of the health care centers participating in the Di@bet.es. The study was supported by CIBERDEM (Centro de Investigación Biomédica en Red de Diabetes y Enfermedades Metabólicas Asociadas) from the Instituto de Salud Carlos III (Ministerio de Ciencia e Innovación), Ministerio de Sanidad y Consumo and the SED (Sociedad Española de Diabetes). We are indebted to José Rios and Ferran Torres from the Biostatistics and Data Management Core Facility IDIBAPS (Institut d’Investigacions Biomèdiques August Pi i Sunyer) for methodological assessment and statistical recommendations.
F. Soriguer, J. Franch, C. Castell, A. Goday, J. Vendrell, R. Casamitjana, A. Bosch-Comas, E. Bordiú, A. Calle-Pascual, R. Carmena, L. Castaño, M. Catalá, E. Delgado, S. Gaztambide, J. Girbés, A. López-Alba, M.T. Martínez-Larrad, E. Menéndez, I. Mora-Peces, G. Pascual-Manich, G. Rojo-Martínez, M. Serrano-Ríos, I. Urrutía, S. Valdés, J.A. Vázquez, R. Gomis, E. Ortega.