Heart failure is a major health care problem in Spain, although its precise impact is unknown due to the lack of data from appropriately designed studies. In contrast with the 2% prevalence of heart failure elsewhere in Europe and in the United States, studies in Spain report figures of 5%, probably because of methodological limitations. Heart failure consumes enormous quantities of health care resources; it is the first cause of hospitalization in persons aged 65 years or older and represents 3% of all hospital admissions and 2.5% of health care costs. There are two patterns of heart failure: one with preserved systolic function, more often associated with high blood pressure, and another with depressed systolic function, more often associated with ischemic heart disease. In 2010, heart failure accounted for 3% of all deaths in men and for 10% of all deaths in women. In recent years, the mortality rate from heart failure has gradually fallen. The rise in hospital admissions for heart failure and the decrease in mortality from this cause could partly be explained by temporary changes in diagnostic coding, but there is evidence that the reduced mortality could also be due to adherence to clinical practice guidelines.
Keywords
Heart failure (HF) is a major concern in public health.1 In the developed world, this disease affects approximately 2% of the adult population, a prevalence that increases exponentially with age. The prevalence is lower than 1% in the population aged less than 50 years but doubles with each decade, and exceeds 8% in persons aged more than 75 years.2 In Spain, the large number of patients with HF is essentially due to progressive population aging. In the interval between the 1991 census and 1 January 2012, the Spanish population aged 65 years and older grew from 5 370 252 to 8 029 674 inhabitants, a 50% increase. Moreover, from 1991 through 2011, life expectancy rose more than 2 years in persons aged 65 to 76 years and 1-2 years in those aged 77 to 87 years.3,4 In contrast, although a lack of definitive empirical evidence precludes certainty, it can be assumed that advances in the treatment of ischemic heart disease and improved blood pressure control have successfully reduced mortality, even though survivors may have left ventricular dysfunction and HF.5
The total impact of HF is increased by its unfavorable medium-term prognosis, which is similar to that of the most prevalent neoplasms.6,7 Mortality due to HF has changed little, although it seems to have fallen in the subgroup of patients with HF with depressed systolic function, who have benefited from improved prognosis due to pharmacologic and nonpharmacologic interventions in recent decades.6
In addition, HF leads to huge health care resource consumption. Historically, HF has caused 3% to 5% of hospital admissions in Spain and is the highest-ranked cause of hospitalization in patients aged more than 65 years.7,8 It is estimated that 2% of health care expenditure in the developed world is allocated to HF and no apparent trend toward a reduction in admissions for HF has appeared in the last 10 years. However, HF is very “sensitive” to care in the community. Several disease management programs for the out-of-hospital management of HF, in which nursing takes the leading role, have proven efficient at reducing admissions.
The present study aims to review the most relevant epidemiologic aspects of HF reported in the last 20 years in Spain—a task that represents a not inconsiderable challenge. The main difficulty is due to the scarcity of population-wide studies and high-quality registries of HF. In Spain, data on the prevalence of HF and its associated hospitalization and mortality rates mainly come from regional studies, and their results and estimates cannot always be extrapolated to the general population. Moreover, most studies are of hospital-based populations, which implies a bias because only patients with the most severe symptoms attend hospital. In fact, approximately 50% of patients with a left ventricular ejection fraction of less than 30% are asymptomatic or have few symptoms.9 As described below, in the out-of-hospital setting, the problem is reversed because the limitations of a clinical diagnosis of HF lead to an incorrect diagnosis rate around 50%.10
INCIDENCE AND PREVALENCE OF HEART FAILURE IN SPAINIncidence is defined as the number of new cases of a disease appearing in a given population over a specific period. In Spain, there is only one study of the incidence of HF.11 This study was performed the population of Puerto Real, a provincial town in the southwest of the country, and analyzed the population older than 14 years (267 231 inhabitants) registered with the Spanish National Health Service between 2000 and 2007. Diagnosis of HF was based on the Framingham clinical criteria. The incidence was 2.96/1000 persons-year in 2000 and 3.90/1000 persons-year in 2007. Essentially, these figures do not differ from those of the Framingham study, conducted in the United States in the 1980s, with an incidence of 4.7/1000 persons-year among the population older than 45 years.12 More recent European studies, such as those conducted in Rotterdam13 and Hillingdon,14 reported that the incidence of HF increased with age. In the latter study, the incidence was 1.4 (for each 1000 persons-year) at age 50 to 59 years, 3.1 at 60 to 64 years, 5.4 at 65 to 69 years, 11.7 at 70 to 74 years, and 17.0 in persons aged 75 years or older.14 Up to the age of 75 years, the incidence of HF was higher in men; after 75 years, it was similar in both sexes, before becoming higher in elderly women (age>85 years).
Prevalence of Heart FailurePrevalence quantifies the proportion of persons in a given population with a specific disease at a particular moment or over a specific period. Prevalence studies are cross-sectional and can be population-based or region-based. Population-based studies require a representative national registry and substantial investment and consequently, in practice, region-based studies are more common.
Only 2 population-based studies of the prevalence of HF have been conducted in Spain: the PRICE (Prevalencia de Insuficiencia Cardiaca en España [Heart Failure Prevalence Study in Spain]) study and the EPISERVE (Insuficiencia cardiaca en consultas ambulatorias: comorbilidades y actuaciones diagnóstico-terapéuticas por diferentes especialistas [Heart failure in outpatients: comorbidities and management by different specialists]) study. PRICE study data were drawn from 15 centers in 9 Spanish autonomous communities, selected without preestablished randomization criteria (the centers met the required characteristics and volunteered to participate). By random sampling, 2703 people older than 45 were invited to participate and 66% accepted. A diagnosis of HF was suspected in primary care (PC) using Framingham criteria and was confirmed by cardiologists if there were echocardiographic findings of significant organic or functional abnormalities. When these criteria were applied, the prevalence of HF was 6.8% and was similar in men and women. By age, the prevalence of HF was 1.3% at age 45 to 54 years, 5.5% at 55 to 64 years, 8% at 65 to 75 years, and 16.1% at >75 years.15
EPISERVE involved 507 researchers from regions all over Spain (except La Rioja), attending outpatient PC, cardiology and internal medicine clinics. Some 2534 patients were studied (5 per researcher) and HF was defined using Framingham criteria. The prevalence was 4.7%.16
Similar figures have been found by other regional studies in Spain. In Asturias, the prevalence in 2001 was 5%17; in Zaragoza, in 1994, Gallego-Catalán et al. described a prevalence of 6.3% in patients older than 65 years: 4.5% at age 65 to 74 years and 8.5% at >5 years.18 In these two regional studies, diagnosis of HF was based on Framingham criteria alone. Consequently the figures reported by PRICE, which applied more exacting criteria, would be expected to be lower than those in these regional studies. This discrepancy could be explained by the limitations of PRICE (selection bias of the participating centers and no data on 34% of the participants selected).
Other regional prevalence studies have been based on computerized registries that codify diagnoses using ICD (International Classification of Disease) criteria. The prevalence data in these registries are clearly lower: a study performed in Lérida (published in 2011) reported a prevalence of 1% in Spanish National Health Service patients older than 14 years,19 and another study performed in Madrid in the same period reported a prevalence of 0.69%.20
To contextualize these figures, a well-designed study in the United States, published in 2003, reported a total HF prevalence of 2.2%, with a significant increase from 0.7% in persons aged 45 to 54 years to 8.4% in those older than 75 years.21 In Europe, two important studies of HF diagnosis were based on the sum of clinical criteria and echocardiographic findings, as recommended in the Clinical Practice Guidelines of the European Society of Cardiology.1 One of these studies, performed in Glasgow, reported a total prevalence of 1.5%.8 The other, which was performed in Rotterdam and included the population older than 55 years (mean, 74 years), reported a prevalence of 1% at 55 to 65 years, 4% at 65 to 74 years, 9.7% at 75 to 84 years, and 17.4% at 85 years or older.14
Overall, the prevalence of HF reported in Spanish studies is higher (by approximately 2-fold) than prevalence figures described in other western countries. Although some authors believe this discrepancy could reflect a real difference and might be due to differences among the populations studied, we believe it more likely that the figures differ because of the methodological peculiarities of the various studies. As previously mentioned, participation in Spanish population-based studies has been based on practical considerations or on volunteering, which suggests a “positive” selection bias.
Other epidemiologic studies, specifically those reporting lower prevalence figures, used registries using ICD-9 or ICD-10 codes, and were essentially based on the Minimum Basic Data Set of Hospital Discharges, which has been compulsory in Spain since 1992. The validity of these registries depends on accurate coding. Several authors have reported wide interinstitutional variability and a lack of reliability in HF diagnoses recorded in administrative registries.22,23 Data retrieval is obviously limited by the quality of the data stored. Therefore, any epidemiologic study of HF based on administrative registries should validate the quality of the data by an independent audit, as well as by interobserver and intraobserver correlation studies of data coding and extraction.
We conclude this review of studies on the incidence and prevalence of HF in Spain by emphasizing their scarcity and the discrepancies between their results and those of neighboring countries, which can partly be explained by methodological failings. In the words of Dr Alonso-Pulpón, “the jury is still out” on Spanish HF studies.24 To obtain reliable information on the situation in Spain, appropriately-designed population-based studies that use current HF diagnostic criteria are needed.
DEMOGRAPHIC AND CLINICAL CHARACTERISTICS OF PATIENTS WITH HEART FAILURE IN SPAINDespite the discrepancies in the reported incidence and prevalence of HF, this disease clearly has a substantial impact on health care in Spain. For this reason, research into the causes of HF and its risk factors, clinical profile, and associated comorbidities, etc., are important to plan appropriate prevention and treatment strategies. Because of the environmental, dietary, and cultural peculiarities of a Mediterranean country such as Spain, the risk factors and clinical course of patients with HF in this country may differ from those of patients in other western countries.25
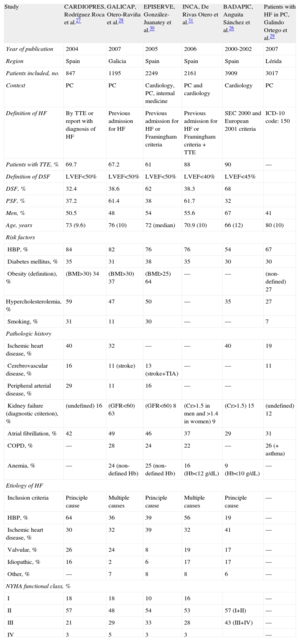
Numerous registries, some with broad-ranging patient samples, provide important information on the clinical characteristics of patients with HF in Spain. The findings of the last 20 years from the main registries are summarized in the Table.
Characteristics of Patients With Heart Failure
| Study | CARDIOPRES, Rodríguez Roca et al.27 | GALICAP, Otero-Raviña et al.28 | EPISERVE, González-Juanatey et al.30 | INCA, De Rivas Otero et al.31 | BADAPIC, Anguita Sánchez et al.26 | Patients with HF in PC, Galindo Ortego et al.29 |
| Year of publication | 2004 | 2007 | 2005 | 2006 | 2000-2002 | 2007 |
| Region | Spain | Galicia | Spain | Spain | Spain | Lérida |
| Patients included, no. | 847 | 1195 | 2249 | 2161 | 3909 | 3017 |
| Context | PC | PC | Cardiology, PC, internal medicine | PC and cardiology | Cardiology | PC |
| Definition of HF | By TTE or report with diagnosis of HF | Previous admission for HF | Previous admission for HF or Framingham criteria | Previous admission for HF or Framingham criteria + TTE | SEC 2000 and European 2001 criteria | ICD-10 code: 150 |
| Patients with TTE, % | 69.7 | 67.2 | 61 | 88 | 90 | — |
| Definition of DSF | LVEF<50% | LVEF<50% | LVEF<50% | LVEF<40% | LVEF<45% | |
| DSF, % | 32.4 | 38.6 | 62 | 38.3 | 68 | |
| PSF, % | 37.2 | 61.4 | 38 | 61.7 | 32 | |
| Men, % | 50.5 | 48 | 54 | 55.6 | 67 | 41 |
| Age, years | 73 (9.6) | 76 (10) | 72 (median) | 70.9 (10) | 66 (12) | 80 (10) |
| Risk factors | ||||||
| HBP, % | 84 | 82 | 76 | 76 | 54 | 67 |
| Diabetes mellitus, % | 35 | 31 | 38 | 35 | 30 | 30 |
| Obesity (definition), % | (BMI>30) 34 | (BMI>30) 37 | (BMI>25) 64 | — | — | (non-defined) 27 |
| Hypercholesterolemia, % | 59 | 47 | 50 | — | 35 | 27 |
| Smoking, % | 31 | 11 | 30 | — | — | 7 |
| Pathologic history | ||||||
| Ischemic heart disease, % | 40 | 32 | — | — | 40 | 19 |
| Cerebrovascular disease, % | 16 | 11 (stroke) | 13 (stroke+TIA) | — | — | 11 |
| Peripheral arterial disease, % | 29 | 11 | 16 | — | — | |
| Kidney failure (diagnostic criterion), % | (undefined) 16 | (GFR<60) 63 | (GFR<60) 8 | (Cr>1.5 in men and >1.4 in women) 9 | (Cr>1.5) 15 | (undefined) 12 |
| Atrial fibrillation, % | 42 | 49 | 46 | 37 | 29 | 31 |
| COPD, % | — | 28 | 24 | 22 | — | 26 (+ asthma) |
| Anemia, % | — | 24 (non-defined Hb) | 25 (non-defined Hb) | 16 (Hb<12 g/dL) | 9 (Hb<10 g/dL) | — |
| Etiology of HF | ||||||
| Inclusion criteria | Principle cause | Multiple causes | Principle cause | Multiple causes | Principle cause | — |
| HBP, % | 64 | 36 | 39 | 56 | 19 | — |
| Ischemic heart disease, % | 30 | 32 | 39 | 32 | 41 | — |
| Valvular, % | 26 | 24 | 8 | 19 | 17 | — |
| Idiopathic, % | 16 | 2 | 6 | 17 | 17 | — |
| Other, % | — | 7 | 8 | 8 | 6 | — |
| NYHA functional class, % | ||||||
| I | 18 | 18 | 10 | 16 | — | |
| II | 57 | 48 | 54 | 53 | 57 (I+II) | — |
| III | 21 | 29 | 33 | 28 | 43 (III+IV) | — |
| IV | 3 | 5 | 3 | 3 | — | |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; Cr, creatinine; DSF, depressed systolic function; GFR, glomerular filtration rate; Hb, hemoglobin; HBP, high blood pressure; HF, heart failure; ICD, International Classification of Disease; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; PC, primary care; PSF, preserved systolic function; SEC, Spanish Society of Cardiology; TIA, transitory ischemic accident; TTE, transthoracic echocardiography:.
Unless otherwise indicated, data are expressed as mean (standard deviation).
Analysis of these data reveals that there are two clearly distinct clinical profiles, which, in the Spanish health system, are linked to the setting where patients are attended. Patients followed up by cardiology services—who are systematically recorded in the BADAPIC26 registry—are younger, mainly men, and usually have depressed systolic function (two-thirds of patients). In this group, the predominant etiology of heart disease is ischemic, and symptoms are more severe. In contrast, patients with HF followed up in PC—recorded in CARDIOPRES27, GALICAP,28 and in the study of Galindo Ortego et al.29 on patients with HF in PC are older (mean age typically >70 years), with a higher proportion of women. The patients frequently have a history of high blood pressure, obesity, and other cardiovascular risk factors and have a greater number of comorbidities, such as kidney failure and atrial fibrillation. Most have preserved systolic function, although echocardiographic studies are not conducted systematically in PC. The most common etiology of heart disease was hypertensive cardiopathy and, generally, symptoms were mild or moderate.
Two studies, EPISERVE30 and INCA31, include populations attended both in cardiology and in PC and internal medicine services; these patients show characteristics midway between those of the two previously-described profiles.
Overall, the profile of patients attended in PC is similar to that in population-based studies, whereas patients attended by cardiologists are more similar to series of patients admitted to hospital and those included in clinical trials of HF.
Significantly, despite being the oldest publication, the BADAPIC registry of HF patients, who were attended by cardiologists, has the highest percentage of patients undergoing echocardiographic studies. This practice increases diagnostic reliability and facilitates the identification of HF with preserved or depressed systolic function, which is crucial to selecting the correct therapeutic approach. BADAPIC compared the baseline characteristics of patients older than 70 years with preserved function with those of patients with systolic dysfunction. The group with preserved systolic function included more women (53% vs 34%), and the most frequent etiology was high blood pressure (62%). In contrast, in the group with depressed systolic function, the most prevalent risk factors were hyperlipidemia and smoking, and the most common cause of HF was ischemia (62%). Another interesting health care datum is the number of admissions in each group: 62% of patients with depressed systolic function had previously been admitted to hospital compared with 40% of those with preserved systolic function (P<.001).
HOSPITAL ADMISSIONS FOR HEART FAILUREThe natural history of HF is punctuated by decompensations that usually require hospitalization and tend to follow a bimodal pattern, with more frequent peaks after diagnosis (30% of readmissions in HF) and in the final stage of the disease (50% of readmissions).32 In Spain, as in other industrialized countries, HF is the leading cause of hospitalization in persons older than 65 years.7 One direct consequence is the financial burden on the Spanish National Health Service. In 1997, Antoñanzas et al.33 reported that the total cost of health care for HF in Spain amounted to 1.8% to 3.1% of the total public health care budget, and that 73% of this expenditure corresponded to in-hospital care. These data have been confirmed in studies elsewhere in the developed world.34
Studies of Hospitalization Rates for Heart Failure and Their LimitationsBetween 1980 and 1993, admissions for HF increased by 71%, and the hospitalization rate due to HF increased by 47% (from 348/100 000 in 1980 to 511/100 000 in 1993). This increase was essentially limited to patients older than 65 years, and a higher number of women were hospitalized. As a result, in 1993 there were nearly 80 000 hospitalizations for HF in Spain.7 Subsequently, Boix Martínez et al.35 showed that the number of discharges for HF rose from 25 000 to 40 000 in men and from 30 000 to 45 000 in women in only 3 years (from 1997 to 1999). Regional studies also reflected an increasing tendency for admissions for HF: in Catalonia, the absolute number of discharges for HF rose from 1735 in 1989 to 6072 in 1994—a relative increase of 250%36; whereas in Andalusia the absolute number of admissions for HF in patients older than 45 years rose from 4345 (1848 men and 2497 women) in 1990 to 10 153 (4488 men and 5665 women) in 2000—a relative increase of 230%; this increase was more pronounced in patients older than 65 years.37
Since 2003, Spain's National Institute of Statistics has gathered data on hospitalizations with a main diagnosis of HF. From 2003-2011, the number of admissions for HF in patients older than 65 years increased by 26%, at a time when the population older than 65 years grew by 13%.38 In other words, the increase in admissions for HF in the older population was 2-fold greater than the population growth.
Although data on the progressive increase in admissions for HF in Spain in the last 30 years are consistent, these figures should be interpreted with caution due to the methodological peculiarities of the studies.5,39 Admission rates for HF are obtained from hospital databases such as the Minimum Basic Data Set. Although the accuracy and quality of the coding system has improved, there remain notable limitations. Reports of patients with HF commonly contain other diagnoses—eg, the factor triggering the episode, baseline cardiomyopathy or comorbidities—that can be mistaken for the main diagnosis, depending on the criteria applied by the person responsible for coding. Moreover, each hospital has different admission criteria, and admissions for HF are spread among cardiology, internal medicine, geriatric, and emergency services, further increasing the difficulty of standardizing discharge diagnoses. Furthermore, in a complex syndrome such as HF, coding is complicated by ambiguous criteria for assigning codes. The classic ICD-9 and ICD-10 systems used in most centers have multiple codes and descriptions for HF diagnosis, and coding can be subject to interpretation. Several authors have shown notable interinstitutional variability and a lack of reliability in HF diagnoses recorded in administrative registries.22,23 All these factors obviously affect the retrieval and exploitation of Minimum Basic Data Set results.5,24
Hospital Admissions for Heart Failure: Clinical Characteristics, Triggering Factors, Presentation and Mean Hospital StayA population-based study conducted in Catalonia by Frigola et al.25 used data from the Minimum Basic Data Set to estimate the frequency of admission of patients with HF followed-up in outpatient clinics. During a 3-year follow-up, 9.5% of the patients required hospitalization for cardiovascular causes—fewer than expected.2,5 This result seems to reflect inaccurate diagnosis of HF in PC when, as in the study by Frigola et al., diagnosis is not based on objective diagnostic criteria such as those of the European Society of Cardiology.1,5,10 In contrast, 37% of admitted patients (whose HF diagnosis is more reliable) were readmitted, confirming the tendency for admissions to cluster in the initial and final stages of HF, as indicated by Desai and Stevenson32 in 2012. The independent predictors of hospitalization identified by these authors were chronic kidney disease (odds ratio [OR]=1.82), ischemic heart disease (OR=1.79), diabetes mellitus (OR=1.51), and chronic obstructive pulmonary disease (OR=1.39).25
Many of the baseline clinical characteristics of patients admitted for decompensated HF are obviously similar to those of outpatients. However, admitted patients are usually older (70% are older than 70 years) and have a greater number of comorbidities (62%) and more advanced NYHA (New York Heart Association) functional class than outpatients (NYHA III-IV in 60% of patients).40
The EAHFE (Epidemiology Acute Heart Failure Emergency) study, that included 944 patients attended in the emergency departments of 10 Spanish tertiary hospitals, investigated gender differences in the presentation and characteristics of patients with acute HF. Women were older (79.7 [9.4] vs 75.6 [10.1] years in men) and had a higher prevalence of high blood pressure (83% vs 75%), valvular heart disease (23% vs 18%) and dementia (7.4% vs 2.5%), while men had a greater prevalence of ischemic heart disease (27% vs 43%), smoking (4.4% vs 19%), chronic obstructive pulmonary disease (14% vs 29%), and chronic liver disease (1.2% vs 4.3%). Diastolic dysfunction was more frequent in women (49% vs 28%) and systolic dysfunction was more frequent in men (51% vs 72%).41
Admissions in patients with HF are usually due to decompensations. Formiga et al.42 identified infections (mostly respiratory in 29% of the patients), arrhythmias (22%), anemia (16%), and lack of treatment adherence (12%) as factors triggering decompensations.42 Of note is that most of these factors are foreseeable and can be corrected with appropriate patient follow-up, which may explain the success of outpatient HF management units in preventing admissions. The most frequent symptoms in patients hospitalized for HF were dyspnea (96%), edema (53%), chest pain (24%), and oliguria (20%).
Approximately 30% of these patients are discharged from the emergency departments rather than other services.43 About 38% of hospitalizations are in cardiology services, and 62% are in internal medicine or geriatrics. As stated earlier in relation to the outpatient management of HF, patients managed outside cardiology services are older (by a mean of 5 years), with a higher proportion of women and a greater number of associated comorbidities—particularly dementia, chronic obstructive pulmonary disease, stroke, and peripheral artery disease.44
The mean length of hospital stay for HF in the most recent studies is around 9 (5) days.25 Predictors of longer hospitalization include female sex and worse functional class at clinical presentation.45
In-hospital Mortality in Admissions for Heart FailureAlthough episodes of decompensated HF are considered relatively benign, in-hospital mortality in patients admitted for HF is greater than mortality among those admitted for entities with a worse “reputation” such as acute coronary syndromes. Specific figures obviously depend on the characteristics of the sample studied. Hermida et al.46 analyzed patients admitted for HF to internal medicine services and found that 9.5% died during admission; in geriatric patients—who were older, had a greater number of comorbidities and worse functional class—Formiga et al.47 reported that 11% died. In the latter study, the variables independently related to an increased risk of death were creatinine level in excess of 200 μmol/l, the presence of lower limb edema, and low functional capacity.
In a study analyzing admissions for HF to all services of the Vall d’Hebron Hospital in 2002, in-hospital mortality was 6.4%, rising to 46% when total mortality from admission to 18 months postdischarge was quantified. In this study, age greater than 75 years, worse functional class, biventricular failure, and comorbidities were independent predictors of death at 18 months.40 Other authors report that low blood pressure at admission is independently associated with higher mortality and an increase in readmission compared with higher blood pressure values.48
HEART FAILURE AS A CAUSE OF DEATHIn the European Union, cardiovascular diseases are the principle cause of death,49 whereas in Spain they come second to cancer.50 In Spain, HF is the fourth cause of cardiovascular death (after ischemic heart disease, cerebrovascular disease, and other heart diseases) and is responsible for 10% of deaths from a circulatory cause in men and 16% in women. Data from Spain's National Institute of Statistics50 indicate that HF caused an absolute 3% of deaths in men and 10% in women in 2010. Overall, HF mortality in Spain has fallen substantially in the last 10 years: in 2000, the overall rate was 46/100 000 inhabitants (28 men and 56 women), falling to 35/100 000 inhabitants (25 men and 45 women) in 2010.50
However, this reduction in HF mortality should be interpreted with caution. In Spain, mortality rates are calculated from registry office data based on death certificates. Since 1974 (when the government's statutory requirements for completing death and cremation certificates were published), the cause of death must be recorded according to official cadaver classification categories. Unfortunately, the validity of certification has scarcely been studied51–54 and therefore there may be temporary differences in diagnostic coding that prevent appropriate comparisons. Similarly, errors in death certificates may result from daily clinical practice. HF is a common outcome in many clinical entities and, therefore, can be used to summarize all the clinical scenarios affecting a patient. This seems more likely in older patients with multiple comorbidities. In addition, the cause of HF (ischemic heart disease, specific cardiomyopathy) is sometimes certified as the cause of death without using the term “heart failure”. Both of these practices can lead to over- and underestimation of real HF rates, respectively.
In support of the validity of data reflecting reduced HF mortality, in 2012 Laribi et al.55 analyzed data from 7 European countries over the last 20 years.55 This analysis confirms that age-adjusted HF mortality is tending to fall, with a mean 40% reduction during follow-up. Spain, together with France, Germany and Greece, is one of the countries where this reduction has been most marked. This study supports the hypothesis that this decrease could be due to a radical improvement in the medical treatment of systolic HF in the last 20 years through the introduction of angiotensin converting-enzyme inhibitors, beta-blockers, aldosterone receptor antagonists, and resynchronization therapy. In the United States, a recent study reports the notable impact of optimized medical treatment following clinical practice guideline recommendations.56 However, in the European Union, the sharp fall in mortality from ischemic heart disease in the last 10 years (30% between 2000 and 2009) suggests the existence of population-wide epidemiologic causes beyond the scope of direct medical intervention.49
Studies of Heart Failure Mortality in SpainTo adequately interpret published data, it is important to distinguish between populations with HF enrolled in outpatient clinics and patient populations followed-up after hospitalization.
In series of outpatients with HF, mortality rates are lower and vary according to baseline characteristics. Hence, BADAPIC reported 6% mortality after a 13 (4) months follow-up,26 a figure lower than that of other Spanish and European studies with a longer follow-up, which typically report 20% to 30% mortality.57 This difference could be a consequence of the BADAPIC population which, as already stated, had a lower mean age (66 years) and fewer comorbidities than the other series.
Two more recent publications underline the same phenomenon: the multicenter MUSIC study reported 27% mortality in a 44-month follow-up,58 whereas, in the Badalona Hospital, Pons et al.59 reported higher mortality (37% at 36 months). In the latter study, patients had a higher mean age (69 vs 65 years), worse functional class, and a higher percentage of comorbidities (kidney failure and diabetes mellitus) and of ischemic HF.
The MUSIC study constructed a model to predict the risk of death. This model is similar to the well-known Seattle Heart Failure Risk Score and includes variables such as left atrium diameter, left ventricular ejection fraction less than 35%, intraventricular conduction abnormalities, analytic values such as hyponatremia, glomerular filtration rate, N-terminal pro-brain natriuretic peptide and troponin positivity. This model allows estimation of the risk of all-cause mortality, cardiac mortality, pump-failure death, and sudden death.
In-hospital mortality during admission for HF has already been discussed, but the prognostic implications of admission for HF go far beyond the period of hospitalization. As stated, in patients admitted to the Vall d’Hebron Hospital40 in-hospital mortality was 6.4% but at 18 months postdischarge cumulative mortality had risen to 46%.
Grigorian-Shamagian et al. studied mortality and its causes in 1360 patients hospitalized for HF, with a long mean follow-up (8 years).60 Mortality at 3.7 years was 45%. In 2005 this group, from the northwestern city of Santiago de Compostela, reported that survival at 1 year after hospitalization for HF had progressively improved over the preceding 10 years in patients with left ventricular dysfunction, whereas mortality in patients with preserved systolic function was unchanged.61 This finding seems to confirm the “real world” effectiveness of distinct treatments that reduce mortality from HF with systolic dysfunction in clinical trials in recent decades, as well as the absence of significant advances in treating diastolic HF.6
Causes of Death in Patients With Heart FailureSeveral of the previously mentioned studies have analyzed cause of death. Pons et al.59 reported that 66% of deaths were of cardiovascular cause, essentially progression of HF (32% of total deaths), followed by sudden death, acute myocardial infarction, and other cardiovascular causes.
Grigorian-Shamagian et al.61 studied patients admitted for HF with a follow-up of up to 8 years and reported that the causes of death were decompensated HF (39%), sudden death (16%) and noncardiovascular causes (17%), myocardial infarction (15%), and vascular death (12%). Comparing these causes of death with ventricular function, these authors found no significant differences between patients with preserved function and those with depressed function, although the proportion of sudden deaths tended to be higher among patients with depressed left ventricular ejection fraction (21% vs 16%). However, they did find differences in the distribution of cause of death at 18 months follow-up postdischarge. Therefore, patients with depressed function had a cumulative risk of death from myocardial infarction of 50% in the first month after discharge, while patients with preserved function had a lower risk until 8 months after discharge. This latter group has a greater probability of death from noncardiovascular causes in the first 5 months postdischarge.
Sudden death in the context of HF remains a major challenge for clinicians. Uncertainty about the benefit of automatic defibrillator implantation is due to the low probability of sudden death reported (5.8% in Pons et al. study and 9.1% in MUSIC study) and the difficulty of accurately stratifying risk of sudden death. Hence, the indication for automatic defibrillator implantation in current guidelines extends to symptomatic patients with left ventricular ejection fraction of less than 35% if they have been under appropriate medical treatment for 3 months. The evidence is weaker for patients with nonischemic HF. Most of these patients do not receive discharges from the device and therefore research into more efficient methods of selecting those patients who could benefit from an implantable cardioverter-defibrillator remains a priority.
The high percentage of deaths from noncardiovascular causes (6.9% in Grigorian-Shamagian et al., 5.4% in MUSIC, and 9.8% in Pons et al.) reflects the high comorbidity of patients with HF who, as previously mentioned, are increasingly older and more fragile. This implies the need for more comprehensive management of individual patients and improved coordination among health care levels to allow early detection of conditions that can arise during the clinical course of patients with HF.
CONCLUSIONSHistorically, in Spain, there has been a lack of reliable nationwide, population-based studies to allow accurate measurement of the impact of HF. While the prevalence of HF in other European countries and the United States is approximately 2%, Spanish studies report figures of 5% or higher. This difference is unlikely to reflect reality and is more likely due to methodological limitations of studies in Spain.
The clinical characteristics of patients with HF form two typical patterns: one with preserved systolic function, more closely associated with women of more advanced age with a history of high blood pressure, who are generally followed up in PC; the other associated with depressed systolic function, more closely associated with ischemic heart disease in middle-aged men, who are more commonly followed-up in cardiology services.
The number of admissions for HF in Spain has increased in the last 20 years, especially in persons older than 65 years. Mortality related to hospitalization for HF is high and its incidence extends over months or years following discharge.
In 2010, HF accounted for 3% of all deaths in men and for 10% of all deaths in women. The mortality rate for HF has gradually fallen in recent years. The increase in admissions and the fall in HF mortality can partially be explained by limitations in diagnostic coding systems. Another factor that could have reduced mortality is adherence to clinical practice guidelines.
Due to the enormous health care and social cost of HF and because prevention of this disease and limiting is repercussions is within our grasp, we propose the creation of an institution or center which, by drawing on the efforts of health care planners, epidemiologists and medical professionals, would enable us to identify the reality of HF (and other cardiovascular diseases) through nationwide studies, and to plan for adequate resources that would reduce its impact in our society.
CONFLICTS OF INTERESTNone declared.