To the Editor:
In the majority of patients with permanent pacemakers with endocavitary stimulation on the right ventricle, a left bundle branch block pattern on the surface electrocardiogram that makes it difficult to identify acute myocardial ischemia. Occasionally, the changes in the repolarisation of these stimulated complexes can reveal myocardial lesions in the context of an acute coronary syndrome, as described in these illustrative cases.
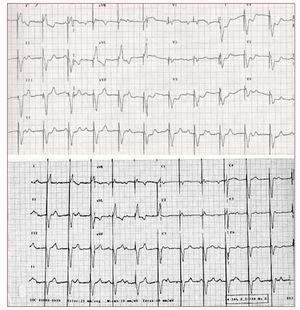
The first case is a 76-year-old woman with a history of hypertension, paroxysmal atrial fibrillation, moderate combined mitral valvulopathy, and endocavitary pacemaker (mode VVI) due to complete atrioventricular block. She was admitted to hospital presenting angina with elevated myocardial lesion markers (troponin I, 11.43 ng/ mL). The ECG demonstrated a paced rhythm with stimulated complexes with left bundle branch block morphology and ST segment depression of 3 mm from V3 to V6 concordant with the QRS complex, with normalized after the angina symptoms creased with medical treatment (Figure 1). Clinical course was favourable with conservative management and there was no evidence of heart failure or arrhythmic episodes. The echocardiography displayed study demonstrated preserved systolic function and localized septal and anterior hypokinesia.
Figure 1.Electrocardiogram during acute ischemia, with ST segment depression of 3 mm from leads V3 to V6 concordant with the QRS complex polarity and the baseline electrocardiogram.
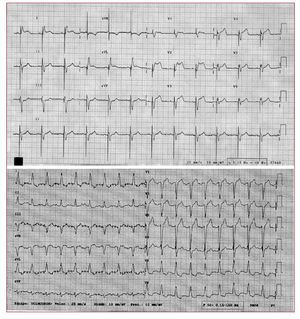
Case 2 is an 81-year-old female, with a history of dyslipidemia, hypertension, and endocavitary pacemaker (mode VDD) due to complete atrioventricular block. She was admitted to the emergency room with angina, nausea and profuse sweating; the surface ECG showed a pacemaker rhythm with atrial tracking and left bundle branch block morphology with ST segment elevation of 5 mm in leads V2, V3 and V4, not concordant with the QRS complex (Figure 2A). Urgent coronary arteriography disclosed atherothrombotic occlusion of the mid-proximal anterior descending artery and percutaneous coronary intervention was performed (angioplasty and bare metal stent deployment). Clinical course was favourable (tropinin I, 32.7 ng/ mL), with normalisation of repolarisation in paced QRS complexes (Figure 2B). Ventriculography displays anterior hypokinesia, with mild systolic dysfunction.
Figure 2.Electrocardiogram displaying ST segment elevation of 5 mm in leads V2, V3 and V4, not concordant with the QRS complex polarity and the baseline electrocardiogram.
In the GUSTO I study, Sgarbossa et al1 described the sensitivity and specificity of various ECG patterns to diagnose an acute coronary syndrome in the presence of right bundle branch block morphology, both native and induced by endocavitary pacing from the right ventricle,2 as well as the increased risk that these represent for those suffering the episode.
In the ECG with right endocavitary pacing, both ST segment depression >1 mm in precordial leads with concordant QRS complex polarity, and ST segment elevation >5 mm with opposite QRS complex polarity presented low sensitivity for diagnosis (25% and 31%, respectively). However, specificity is very high (96% and 92%), so this finding represents a considerably excessive risk (odds ratio [OR] =6 and OR=4.3, respectively; <.05) and, therefore, a valuable diagnostic tool.3 The reduced sensitivity of these criteria increases considerably (67%) when the electrical changes are dynamic in relation to the episodes of pain.4 In the presented cases, the elevation of myocardial necrosis markers and the echocardiographic or angiographic findings confirm the diagnosis of acute coronary syndrome indicated by the surface ECG.