Keywords
INTRODUCTION
Idiopathic pulmonary arterial hypertension is an infrequent disease characterized by an increase in pulmonary artery pressure. If left untreated, there is rapid disease progression, which leads to refractory right heart failure and death.1
It has been shown that continuous intravenous infusion of prostacyclin increases long-term survival, and improves quality of life, exercise capacity and hemodynamic parameters.2-4 Treatment with treprostinil and iloprost, stable prostacyclin analogues that are administered subcutaneously or by inhalation, respectively, has resulted in significant improvements in both functional capacity and quality of life.56 Nevertheless, no long-term studies of their effect on survival have been carried out.
Phosphodiesterases (PDEs) form a superfamily of enzymes that inactivate cyclic adenosine monophosphate (cAMP) and guanosine 5'-cyclic monophosphate (cGMP), compounds which are intracellular second messengers for prostacyclin and nitric oxide. Sildenafil is a selective phosphodiesterase type-5 (PDE-5) inhibitor that exerts a vasodilatory effect via the nitric oxide pathway, in a manner dependent on an increase in the intracellular cGMP concentration. High levels of PDE-5 are found in pulmonary muscular arteries and in the corpus cavernosum penis. PDE-5 inhibition results in selective pulmonary artery vasodilatation, which has little impact on systemic vascular resistance. Prostacyclin's vasodilatory effect is mediated by the intracellular second messenger cAMP, which is, in turn, inactivated by PDE-3. It is known that an increase in the intracellular cGMP concentration exerts an inhibitory effect on PDE-3. Sildenafil probably acts in a similar indirect way, thereby functioning synergistically to augment the vasodilatory effect of prostacyclin.7
Experience with the long-term use of sildenafil, whether administered as monotherapy or in association with prostacyclin, for treatment of idiopathic pulmonary arterial hypertension is very limited. There are only few reports on its use in a small number of patients.8-12
The aim of the present study was to investigate the benefits of long-term sildenafil treatment in patients with pulmonary hypertension in whom treatment with prostacyclin, administered as monotherapy through different routes, was insufficient to stabilize patients in New York Heart Association (NYHA) functional class II without signs of right heart failure.
PATIENTS AND METHOD
An observational study was carried out in patients with severe pulmonary hypertension that was either idiopathic or associated with toxic oil syndrome.13 Pulmonary hypertension was diagnosed in all patients before the initiation of prostacyclin treatment using criteria from the United States National Institutes of Health's patient registry for the characterization of pulmonary hypertension.1 All patients had been receiving continuous treatment with prostacyclin or one of its analogues (i.e., intravenous epoprostenol, subcutaneous treprostinil, or iloprost inhalation) for at least 6 months. Long-term oral treatment with sildenafil was added when patients presented at least 2 of the following clinical criteria: a) they were classified as being in NYHA functional class III or IV; b) there were signs of decompensated right heart failure that did not respond to optimized diuretic therapy; c) syncope; and d) a >20% reduction in the distance walked in the 6-min walk test. Decompensated right heart failure was defined as the presence of signs of systemic venous congestion (i.e., hepatomegaly, ascites, or edema) that did not respond to treatment with diuretics. The absence of symptoms and signs of right heart failure was considered as an indication of effective control.
Patients with systemic arterial hypotension (i.e., a systolic arterial pressure <85 mm Hg) or with altered levels of enzymes associated with hepatic cytolysis (i.e., when aspartate aminotransferase and alanine aminotransferase levels were more than three times the normal reference levels) were excluded. The initial sildenafil dose used in all patients was 25 mg per 12 hours. This was increased progressively to a target dosage of 150 mg/day, taken in 3 doses. The prostacyclin dose remained the same during the first 3 months of follow-up; it was later adjusted individually according to the patients' clinical evolution. Patients were informed in advance, both verbally and in writing, of the clinical characteristics of the medicine being administered. Patients gave written agreement (accepting their inclusion in the study and consenting to use of information obtained) and a request was made for compassionate use the medication, which was accepted by the relevant health authorities. In the study, a serious adverse event was defined as any event that was life-threatening, or that resulted in death, permanent incapacity, or the need for hospitalization or prolongation of hospital stay. The medication was regarded as being well tolerated if there were no adverse events and it was possible to increase the dose to the target level.
Between December 2001 and December 2002, 11 out of 45 (24%) patients with idiopathic pulmonary arterial hypertension who had received continuous treatment with prostacyclin for at least 6 months fulfilled criteria for inclusion in the study. These patients underwent clinical follow-up, complete laboratory analysis, evaluation of functional capacity using the standardized 6-min walk test14 (quantified as meters walked), and echocardiography, at baseline and 3 and 12 months after the initiation of sildenafil treatment.
Transthoracic echocardiography was carried out according to an agreed protocol by a single experienced individual using an Acuson Sequoya echocardiographic scanner. All echocardiographic investigations were recorded in both digital and video formats. Quantitative analysis of variables was performed off-line, with values being derived as the mean of 3 measurements. The variables recorded were:
- Geometric parameters that characterize right ventricular function: systolic and diastolic eccentricity indices, which were calculated according to Ryan's method15; fractional area shortening (percentage shortening =100*[end-diastolic areaend-systolic area/end-diastolic area]); diastolic minor diameter, and right atrial area.
- Non-geometric parameters that characterize right ventricular function: myocardial performance index or Tei index.16
- Maximum tricuspid regurgitant jet velocity, which can be used to give an estimate of the pressure gradient between the right ventricle and right atrium by using Bernoulli's equation (p=4v2).17
Statistical Analysis
The SPSS 10.0 statistical program was used. All continuous quantitative variables are expressed as a mean ± standard deviation. The differences between the means of the different quantitative variables measured before and after sildenafil treatment were analyzed using a non-parametric Wilcoxon test. A difference was considered to be statistically significant if the P value was <.05.
RESULTS
Of the 11 patients studied, 7 were men and 4 were women. Their mean age was 42±8 years. Eight patients presented with idiopathic pulmonary arterial hypertension and 3 had pulmonary arterial hypertension associated with toxic oil syndrome.18 Prostacyclin administration was being carried out as follows: 6 patients were receiving treprostinil subcutaneously; 3 were receiving iloprost by inhalation, and 2 were receiving epoprostenol intravenously. The form of prostacyclin administration remained unchanged throughout follow-up. Ten of the 11 patients were followed up for 12 months.
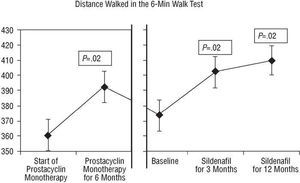
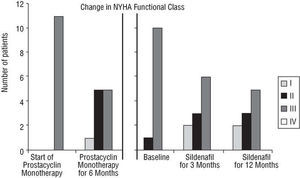
The patients started receiving prostacyclin as monotherapy for a mean of 21 months (range: 634 months) before study entry. Initial responses in the first 6 months were favorable (i.e., there was an increase of 29 m in the distance walked in the 6-min walk test, and NYHA functional class improved in 6 of the 11 patients). Subsequently, the patients' conditions deteriorated markedly and could not be controlled by optimizing their current treatment. For this reason, it was decided to add sildenafil to the existing treatment regimens.
Patients' Clinical Status and Functional Capacity Before Combination Treatment With Sildenafil (Baseline)
All patients were in NYHA functional class III, with the exception of 1 patient who was in NYHA functional class II and who experienced dyspnea and syncope during exertion. Seven of the 11 patients had decompensated right heart failure that did not respond to diuretic treatment. Two patients had syncope, which occurred on minimum exertion in one. The mean distance walked in the 6-min walk test prior to sildenafil administration was 374±63 m. The mean prostacyclin dose before the start of sildenafil therapy was 23±6 ng/kg per min for intravenous epoprostenol, 31±6 ng/kg per min for treprostinil, and 150 µg/day for the 3 patients on iloprost.
Clinical Follow-up After 3 and 12 Months of Combination Treatment With Prostacyclin and Sildenafil
The distance walked in the 6-min walk test increased in all patients, by a mean of 25 m at 3 months and 36 m at 12 months (Figure 1). At 3 month follow-up, 5 patients exhibited an improvement in NYHA functional class (Figure 2). Syncope, which was present in 2 patients, disappeared within the first 3 weeks of treatment. The symptoms and signs of right heart failure, which were observed in 7 patients before initiation of sildenafil treatment, had already disappeared within the first 3 months of combination treatment in 5 patients, and disappeared within the following months in a sixth patient. One patient continued to have decompensated heart failure, though symptoms of congestion were better controlled, and died suddenly in the fourth month of follow-up.
Fig. 1. Change in distance walked in the 6-min walk test (m). P values are for comparisons with baseline parameters. Prostacyclin monotherapy was given for 6 months. The change at 6 months of long-term treatment with prostacyclin monotherapy is shown.
Fig. 2. Change in New York Heart Association (NYHA) functional class.
The mean sildenafil doses achieved at 3 and 12 months were 146±44 mg/day and 152±34 mg/day, respectively. No patient withdrew from treatment because of poor tolerance, hypotension, or altered biochemical liver test results. Two patients experienced headache and 2 had dyspepsia, which meant that the increase in sildenafil dosage in these patients had to be implemented more slowly. Only 1 patient could not be given the target daily sildenafil dosage of 150 mg, because of headache.
Echocardiographic Follow-up of Combination Treatment With Prostacyclin and Sildenafil
Geometric parameters of right ventricular function had improved by the third month of combination treatment and remained unchanged after twelve months. Changes from baseline in the right ventricular minor diastolic diameter and in the diastolic eccentricity index reached statistical significance. There was also an improvement in myocardial performance index, though it did not reach statistical significance. However, the right ventricle-atrium pressure gradient did not change during follow-up (Table).
DISCUSSION
In our study group, which comprised patients with severe pulmonary hypertension in a poor functional state and with a limited therapeutic response margin, long-term treatment with prostacyclin and sildenafil not only stabilized clinical status, but also lead to significant and sustained improvements in exercise capacity (as measured by the 6-min walk test), the level of dyspnea (i.e., in NYHA functional class), and the prevalence of decompensated right heart failure. Similarly, there was also a trend towards beneficial remodeling of the right ventricle, which was demonstrated by improved ventricular function and reduced ventricular dilatation.
After the initiation of prostacyclin monotherapy, our patients followed a favorable clinical course. There was an improvement in NYHA functional class and an increase in the distance walked in the 6-min walk test, as has been described in the medical literature in other patients treated with prostanoids.26,19
However, after 20 months of follow-up and without any concurrent precipitating cause, the patients exhibited a marked functional deterioration, which did not respond to an increase in prostacyclin dose. A particularly important feature was the appearance of right heart failure in more than half the patients. This occurrence was similar to observations reported by Ghofrani et al9 in patients treated with prostacyclin, who responded favorably in the beginning, but who later exhibited a slow and progressive deterioration in hemodynamic parameters and functional capacity after 18 months of treatment.
There are few reports in the literature on combination treatment with prostacyclin and sildenafil. Those that do exist involve, as does this study, only a small number of patients. Our findings are consistent with those reported by Ghofrani et al in a study of 14 patients.10 These investigators observed sustained improvements in NYHA functional class and in exercise capacity during 12 months of follow-up in patients who were receiving long-term treatment with prostacyclin and who had started to show a marked clinical deterioration. However, in a study of 13 patients carried out by Bathia et al,12 the addition of sildenafil to long-term treatment with prostacyclin in clinically stable patients did not produce an effective response. The disparity in results can be explained by the marked differences in the populations studied: in our series and in that of Ghofrani et al, patients had severely limited exercise capacity (i.e., the mean baseline 6-min walking distances were 365±64 m and 305±28 m, respectively) and progressive heart disease, whereas, in Bathia et al's series, patients were clinically stable and had only slightly limited exercise capacity (i.e., a mean baseline 6-min walking distance of 447±111 m). Effective clinical responses are usually more marked in patients whose clinical state is more compromised, as has been observed in recent clinical trials of prostanoids.5,6
Echocardiography enables the function and structure of the right ventricle to be assessed, and has been shown to be a useful tool for investigating idiopathic pulmonary arterial hypertension, in which it not only helps in providing a prognosis for the disease,20 but also in evaluating responses to treatment.21-24
In our patients, we observed a tendency towards beneficial remodeling of the right ventricle, which was characterized by reduced right ventricular dilatation and improved right ventricular function. However, the changes did not reach statistical significance, probably because of the small number of patients studied. Right atrial area, right ventricular myocardial performance index, and systolic and diastolic eccentricity indices, have been proven useful prognostic parameters for evaluating disease progression in patients with pulmonary hypertension.20-24 In our series, favorable changes in these parameters occurred in parallel with the clinical improvements experienced by our patients.
The right ventricle-atrium pressure gradient, from which pulmonary artery systolic pressure can be estimated,17 did not change during follow-up in our patients. In various studies in which echocardiography was used to monitor the therapeutic effects of pharmaceuticals in patients with pulmonary hypertension, it was found that the change in pulmonary artery systolic pressure was small and less important than that in parameters that characterize right ventricular function. Ghofrani et al10 carried out a hemodynamic follow-up in their study. They demonstrated that there was no change in pulmonary artery systolic pressure but confirmed, nevertheless, that there were positive changes in the cardiac index and in the vascular resistance index, both of which are more closely related to right ventricular function.
In our experience, sildenafil was found to be a safe drug. No serious secondary adverse effects, such as systemic hypotension, were observed, probably because the drug's vasodilatory action selectively affects pulmonary vessels.
Patients receiving long-term treatment with prostacyclin who start to exhibit heart failure or functional deterioration in the absence of precipitating factors (e.g., pneumonia or anemia) have a very poor short-term prognosis and need to undergo urgent transplantation.25 In this situation, the favorable responses obtained in our group of patients who were receiving long-term prostacyclin treatment and who exhibited evidence of progressive heart disease are especially relevant.
One death occurred in our series, in a patient who was receiving an epoprostenol infusion. The patient remained in state of severe right heart failure, despite better control of congestive symptoms following the addition of sildenafil, and died suddenly at home during the fourth month of follow-up. It is remarkable that only one death was observed in our patients considering their disease severity and the long duration of the follow-up period.
Although this study was open, uncontrolled and involved only a small number of patients, the low prevalence of the illness and the need to try all of the few therapeutic alternatives available for these patients, whose clinical condition is so dismal, means that these findings are encouraging and of great interest. Moreover, they are in accordance with the results obtained by Ghofrani et al.10
CONCLUSIONS
The administration of sildenafil to patients with severe pulmonary hypertension who exhibit clinical and functional deterioration despite long-term treatment with prostacyclin or one of its analogues resulted in improved NYHA functional class and exercise capacity and reduced signs of decompensated right heart failure. These gains were maintained over time, during a mean follow-up period of 12 months. The combination of treatments that act via different cellular mechanisms could provide a starting point for more effective therapies, which could perhaps be administered at lower doses and which may result in fewer side effects. Moreover, whether sildenafil is used as monotherapy or in combination, its impact on survival is still unknown. Further clinical trials are needed to provide answers to these questions.
Correspondence: Dra. C. Jiménez López-Guarch.
Unidad de Insuficiencia Cardíaca e Hipertensión Pulmonar.
Servicio de Cardiología. Hospital 12 de Octubre.
Ctra. de Andalucía, km 5,400. 28041 Madrid. España.
E-mail: jlguarch@secardiologia.es