The health indicator disability-adjusted life years combines the fatal and nonfatal consequences of a disease in a single measure. The aim of this study was to evaluate the burden of ischemic heart disease in 2008 in Spain by calculating disability-adjusted life years.
MethodsThe years of life lost due to premature death were calculated using the ischemic heart disease deaths by age and sex recorded in the Spanish National Institute of Statistics and the life-table in the 2010 Global Burden of Disease study. The years lived with disability, calculated for acute coronary syndrome, stable angina, and ischemic heart failure, used hospital discharge data and information from population studies. Disability weights were taken from the 2010 Global Burden of Disease study. We calculated crude and age standardized rates (European Standard Population). Univariate sensitivity analyses were performed.
ResultsIn 2008, 539 570 disability-adjusted life years were lost due to ischemic heart disease in Spain (crude rate, 11.8/1000 population; standardized, 8.6/1000). Of the total years lost, 96% were due to premature death and 4% due to disability. Among the years lost due to disability, heart failure accounted for 83%, stable angina 15%, and acute coronary syndrome 2%. In the sensitivity analysis, weighting by age was the factor that changed the results to the greatest degree.
ConclusionsIschemic heart disease continues to have a huge impact on the health of our population, mainly because of premature death. The results of this study provide an overall vision of the epidemiologic situation in Spain and could serve as the basis for evaluating interventions targeting the acute and chronic manifestations of cardiac ischemia.
Keywords
Ischemic heart disease has a major impact on the health of a population, stemming from its acute manifestation, acute coronary syndrome (ACS),1 and chronic manifestations, such as angina and heart failure. These latter forms can develop as sequelae following 1 or various episodes of ACS or be the only clinical expression of the disease.
The disability-adjusted life year (DALY) is a synthetic health indicator used to measure the burden of disease in a population. It provides information on the fatal and nonfatal consequences of diseases and injuries, and their associated risk factors.2 This indicator, which is expressed as the number of years of healthy life lost, has been used to describe the epidemiologic situation in various countries and regions,3 and to estimate the impact of different interventions on the population.4–6
According to data from a previous exploratory study, 4.7 DALYs per 1000 individuals in Spain (6.5 in men and 2.8 in women) were lost in 2008 due to ischemic heart disease. This condition accounts for 4.2% of the total disease burden in our country, and is the third leading specific cause of DALY loss after depression and dementia.7 Calculation of DALY in the exploratory study was performed by an indirect method,2 using mortality data from Spain and morbidity data from the WHO (World Health Organization) for the Euro-A region.8 Euro-A includes countries with widely varying ischemic heart disease-related epidemiology, such as Finland, which has a standardized mortality rate of more than 191 deaths per 100 000 men and 101 per 100 000 women, and France and Spain, with rates of less than 95 and 45 deaths per 100 000 men and women, respectively.9 These differences underscore the importance of using local epidemiologic data to obtain estimations that are more in keeping with the reality of each country. The aim of the present study was to describe the burden of ischemic heart disease in Spain for 2008, through the use of DALY values calculated from national data.
METHODSDisease burden measured in DALYs is the sum of 2 components: the years of life lost (YLLs) due to premature death and the years lived with disability (YLDs). To include the health loss caused by the different manifestations of ischemic heart disease, 3 health states were established, based on the disease model used in the 2010 Global Burden of Disease (GBD) study10: ACS (acute myocardial infarction and unstable angina), stable angina, and heart failure.
Calculation of Years of Life Lost Due to Premature DeathThe overall year of life lost was the sum of the years of life lost per each death due to ischemic heart disease, calculated as the difference between the age of the person at death and the life expectancy at that age taken from the standard life-table reported in the GBD 2010 study.11
Data related to the population and cause-specific mortality were from the Spanish National Institute of Statistics. Deaths with the ICD-10 codes I20 to I25 were selected. Deaths attributed to poorly defined codes were reassigned following the methods used in the original GBD study,2 with the exception of heart failure (code I50). This was retained as a specific cause, and a percentage of the deaths due to heart failure was reassigned to ischemic heart disease based on the epidemiology of Spain. For this purpose, we used data from the GALICAP study, in which 36.8% of heart failure cases in men and 26.6% in women had an ischemic etiology.12
Calculation of Years Lived With DisabilityThe number of YLDs due to ischemic heart disease was estimated by multiplying the number of incident cases of each health state (ACS, stable angina, and ischemic heart failure) by the average duration of the health state, and by an assigned weighting factor that reflected the severity of the disability associated with the health state. To obtain the information required, we preferentially searched population studies carried out in Spain around the year 2008 that provided data by sex and age groups.
Acute Coronary SyndromeVarious publications were identified containing data on the incidence of acute myocardial infarction obtained from population registries.13–24 However, most of these studies focused on specific regions of Spain or covered incident cases from the 1990s, before troponin analysis was routinely used in the diagnosis of acute myocardial infarction. Because of these limitations, we decided to draw on the information in the Spanish Registry of Hospital Discharges (Minimum Basic Data Set),25 which has been used in several studies on acute myocardial infarction.26–29 Episodes were selected in which the main diagnosis was coded as 410, 411.1, 411.81 or 411.89 (ICD-9MC). The duration of the ACS episode was set at 28 days, following the model used in the GBD 2010 study.30
Stable AnginaThe only nationwide prevalence study on stable angina identified31 presented data from 1995 to 1996, which were not considered sufficiently representative of the epidemiologic situation in 2008. Therefore, data from the Minimum Basic Data Set were again used (episodes with the main diagnosis coded as ICD-9MC 413, 414.00, or 414.01). The disease model contemplated 3 levels of angina severity (mild, moderate, and severe), and assigned different disability weights to each. The distribution of prevalent cases among the severity levels was taken from the AVANCE registry.32
Heart FailureThe prevalence data for heart failure were drawn from the PRICE study.33 The YLD calculation only included the percentage of cases attributable to cardiac ischemia, which was taken from the etiologic distribution reported in the GALICAP study (36.8% in men and 26.6% in women).12 The heart failure model contemplated 4 levels of severity, according to the New York Heart Association classification. The distribution of prevalent cases among these levels was taken from the GALICAP study.12
Disability Weights Applied, Social Values and Calculation of RatesThe disability weights applied to each health state were taken from GBD 2010.34 The data used are summarized in Table 1. No discount factors or weighting by age were applied. The crude YLL, YLD, and DALY rates by age groups and sex, and the DALY rates adjusted to the Standard European Population were calculated using the direct method.
Information Sources and Aggregate Data for Each of the Parameters Used to Calculate Disability-adjusted Life Years in Spain in 2008
| Parameter | Information source | Estimation |
|---|---|---|
| Deaths due to ischemic heart disease | INE35 anonymized microdata file | 36 717 + 6241 (from deaths coded with the poorly-defined code I50 – heart failure)a |
| Population | Population estimations published by the INE36 for 2008 | 45 593 385 |
| Annual incidence of ACS episodes | MBDS, 200825 | 52 378 episodes of AMI + 18 361 of unstable angina |
| Duration of ACS episode | GBD study, 201030 | 28 daysb |
| Prevalence of stable angina episodes in 2008 | MBDS, 200825 | 47 232 |
| Distribution of stable angina by severity | AVANCE study32 | 36% mild, 51% moderate, and 14% severe |
| Prevalence of heart failure | PRICE study33 | 1 255 750 persons (391 900 attributed to ischemic HF, according to etiologic distribution observed in the GALICAP12 study) |
| Distribution of HF by etiology | GALICAP study12 | 31.5% ischemic, 35.8% hypertensive, 24.5% valvular, and 8.2% others |
| Distribution of HF by severity | GALICAP study12 | 18.5% asymptomatic, 48% mild, 28.7% moderate, and 4.8% severe |
| Disability weightsc | GBD study, 201034 | ACS first 2 days, 0.422dACS next 26 days, 0.056dMild angina, 0.037Moderate angina, 0.066Severe angina, 0.167Mild HF, 0.037Moderate HF, 0.07Severe HF, 0.186 |
ACS, acute coronary syndrome; AMI, acute myocardial infarction; GBD, global burden of disease; HF, heart failure; INE, Instituto Nacional de Estadística (Spanish National Institute of Statistics); MBDS, Minimum Basic Data Set.
With regard to mortality coding, the code for heart failure (ICD-10 I50) is considered a poorly-defined code. Hence, one should always seek the condition that led to heart failure and establish that condition as the underlying cause of death. Nonetheless, this information is not always available, and a large number of deaths are coded as I50. In 2008 in Spain, there were 20 969 of these cases, of which 6241 were included in the calculation of YLL in the present study. This number corresponds to 36.8% and 26.6% of deaths assigned to code I50 in men and women, respectively, older than 45 years (taken from the percentages of heart failure cases classified as having an ischemic etiology in the GALICAP12 study).
The duration of the acute coronary episode was set at 28 days, in keeping with the value in the GBD 2010 study. Starting with the MONICA study, most epidemiologic population studies, as well as global and regional studies on disease burden, have used the limit of 28 days to establish the lethality of the acute phase of ACS. The disease model assumes that after the first 28 days, disability only occurs when sequelae develop (angina or heart failure), for which the burden of disease was calculated separately.
Range of possible values from 0 to 1, from the least to the most severe disability. The disability weights in the GBD 2010 study were obtained using an international population survey, carried out by personal interviews at the patient's home, telephone contact, or information sent through the web site. The participants had to indicate which of 2 hypothetical patients in different health states they considered had better health. The online survey additionally contained questions asking whether the benefits attained in the population secondary to different health interventions were equivalent. The results of the survey were analyzed by statistical methods to obtain a disability weight for each of the health states considered.
The calculations were performed in 8 scenarios that differed from the base case in 1 or more of the following parameters: life-table,11 discount rate, age weighting, disability weighting,8,34,37 and prevalence of heart failure. The GesMor software package was used for the calculations.
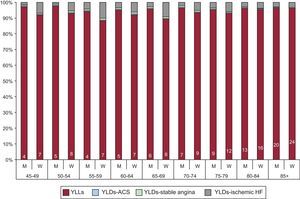
RESULTSIn 2008, 539 570 DALYs were lost in Spain due to ischemic heart disease (358 230 in men and 181 340 in women). The crude DALY rate per 1000 inhabitants was 11.8 (15.9 in men and 7.9 in women) and the adjusted rate was 8.6 (13.4 in men and 4.3 in women). YLLs accounted for 96% of this disease burden (97% in men and 95% in women), with no significant differences between the age groups (Figure 1).
Weight of each of the components of the burden of ischemic heart disease in persons older than 45 years, by age group and sex: Spain 2008. The numbers in the lower part of each bar represent the percentage of years of life lost due to premature death among deaths assigned the code 150 with respect to the total number of years of life lost in each age- and sex-specific group (for further details on how these deaths were incorporated in the calculation of years of life lost due to premature death, see the “Methods” section). ACS, acute coronary syndrome; HF, heart failure; M, men; W, women; YLDs, years lived with disability; YLLs, years of life lost due to premature death.
Inclusion of the percentage of deaths coded as heart failure attributable to an ischemic cause in the YLL calculation implied a 10.7% increase in the number of YLLs due to ischemic heart disease. The percentage of YLLs resulting from inclusion of these deaths was higher in women than in men in all the age groups and increased with age, reaching 20% in men and 24% in women in the group aged 85 years and older (Figure 1).
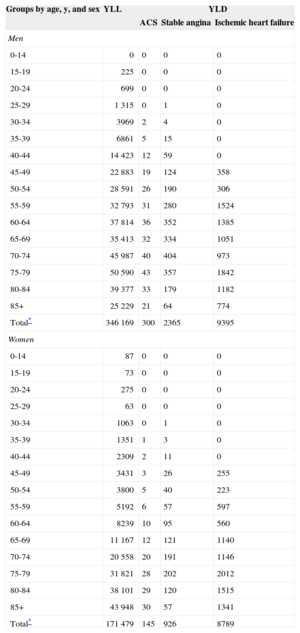
Ischemic heart failure accounted for 83% of the YLDs (18 184 YLDs), stable angina 15% (3291), and ACS 2% (445). The relative disability weight secondary to angina was greater in men than in women in all the age groups, and decreased starting at age 75 to 79 years, at which time the weight assigned to heart failure began to increase. The number of YLLs and YLDs lost to ischemic heart disease are shown in Table 2 by age and sex.
Number of Years of Life Lost due to Premature Death and Years Lived With Disability for Each of the Ischemic Heart Disease Health States, by Age Groups and Sex. Spain, 2008
| Groups by age, y, and sex | YLL | YLD | ||
|---|---|---|---|---|
| ACS | Stable angina | Ischemic heart failure | ||
| Men | ||||
| 0-14 | 0 | 0 | 0 | 0 |
| 15-19 | 225 | 0 | 0 | 0 |
| 20-24 | 699 | 0 | 0 | 0 |
| 25-29 | 1 315 | 0 | 1 | 0 |
| 30-34 | 3969 | 2 | 4 | 0 |
| 35-39 | 6861 | 5 | 15 | 0 |
| 40-44 | 14 423 | 12 | 59 | 0 |
| 45-49 | 22 883 | 19 | 124 | 358 |
| 50-54 | 28 591 | 26 | 190 | 306 |
| 55-59 | 32 793 | 31 | 280 | 1524 |
| 60-64 | 37 814 | 36 | 352 | 1385 |
| 65-69 | 35 413 | 32 | 334 | 1051 |
| 70-74 | 45 987 | 40 | 404 | 973 |
| 75-79 | 50 590 | 43 | 357 | 1842 |
| 80-84 | 39 377 | 33 | 179 | 1182 |
| 85+ | 25 229 | 21 | 64 | 774 |
| Total* | 346 169 | 300 | 2365 | 9395 |
| Women | ||||
| 0-14 | 87 | 0 | 0 | 0 |
| 15-19 | 73 | 0 | 0 | 0 |
| 20-24 | 275 | 0 | 0 | 0 |
| 25-29 | 63 | 0 | 0 | 0 |
| 30-34 | 1063 | 0 | 1 | 0 |
| 35-39 | 1351 | 1 | 3 | 0 |
| 40-44 | 2309 | 2 | 11 | 0 |
| 45-49 | 3431 | 3 | 26 | 255 |
| 50-54 | 3800 | 5 | 40 | 223 |
| 55-59 | 5192 | 6 | 57 | 597 |
| 60-64 | 8239 | 10 | 95 | 560 |
| 65-69 | 11 167 | 12 | 121 | 1140 |
| 70-74 | 20 558 | 20 | 191 | 1146 |
| 75-79 | 31 821 | 28 | 202 | 2012 |
| 80-84 | 38 101 | 29 | 120 | 1515 |
| 85+ | 43 948 | 30 | 57 | 1341 |
| Total* | 171 479 | 145 | 926 | 8789 |
ACS, acute coronary syndrome; YLD, years lived with disability; YLL, years of life lost due to premature death.
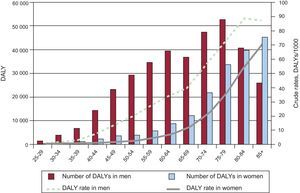
The number of DALYs lost gradually increased with age in both sexes, although the increase was faster from young ages in men. In the group younger than 65 years, 43% of DALYs corresponded to men and 15% to women. A decrease in DALYs was observed after the age of 80 years in men, whereas the progressive increase was maintained in all the age groups in women (Figure 2). Crude DALY rates increased with advancing age in both sexes, except in men aged 85 years and older. The crude DALY rate was higher in men than in women in all the age groups, at a ratio of 2.0. The greatest difference was seen in the 50- to 54-year-old group, with a man:woman ratio of 7.3, and the minimum was in the group 85 years and older, with a ratio of 1.2.
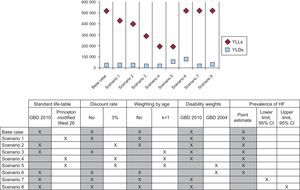
In the sensitivity analysis (Figure 3), the individual parameter with the greatest impact on the overall calculation of DALYs due to ischemic heart disease was weighting by age (scenario 3), with 44% fewer DALYs than in the base case. Scenario 5, in which parameters recommended by the WHO before the GBD 2010 study38 were applied (Princeton modified model life-table West level 26, and age weighting, discount rate, and disability weighting from 2004), yielded 54% fewer DALYs than the base case (63% fewer YLLs and 146% more YLDs). After applying the disability weights from the GDB 2004 study and maintaining the remaining parameters (scenario 6), the number of YLDs increased by more than 250% and the number of DALYs by 11%. The impact of the heart failure prevalence data on the total of DALYs due to ischemic heart disease was found to be 2% above or below that of the base case, depending on whether the upper or lower limit of the confidence interval was used for the prevalence.
DISCUSSIONThe results of this study provide a detailed description of the burden of disease attributable to ischemic heart disease in Spain in terms of mortality and disability, using data from studies and information sources from the same country and taking into account both acute episodes and chronic expressions of the disease. Year of life lost due to premature death accounted for more than 90% of the total DALYs due to ischemic heart disease. In the YLL calculation, inclusion of deaths assigned the code I50, heart failure, which is considered a poorly defined code, increased the YLL value by 11% and the DALY value by 10%. This increase was particularly evident in women (17%) and in the older age groups (29% in patients aged 85 years and older).
The disability component made a substantially smaller contribution than premature death, but in absolute terms, it was also found to have a relevant impact on the health of the population. This was mainly seen for the disability associated with ischemic heart failure: 0.4 YLD/1000 inhabitants and 2.3 YLD/1000 persons older than 75 years).
The distribution of DALYs by age, in which 6% of the total was in persons younger than 45 years and 28% in those aged 45 to 65 years, underscores the importance of primary preventive measures for cardiovascular disease even in the younger population. In parallel, given the sustained increase in the burden of disease with increasing age, these measures, supplemented with secondary and tertiary prevention measures, should be adapted to each population group and maintained up to older ages.
The sensitivity analysis showed that application of the methodology used in the GBD 2010 study yielded a larger number of YLLs and YLDs for ischemic heart disease than if previous proposals from the WHO had been applied. These differences highlight the importance of explicitly describing the parameters and assumptions used in the DALY calculations to enable comparisons of results between studies.
The crude DALY rate of the base case (11.8/1000) used is lower than the value reported for the United Kingdom in 2010 (23.5/1000).39 The results obtained in scenario 5 of the sensitivity analysis enable comparison with studies that applied the previous WHO recommendations: The crude DALY rate for ischemic heart disease was 8.6 cases/10008 in the WHO Euro-A region in 2004 and 20.0 cases/1000 in Serbia in 200040; both of these values are higher than the rate in our study (5.4). The DALY rate adjusted to the European Standard Population was 16.3 cases/1000 in Serbia and 4.2 in our study. These findings are consistent with the lower mortality due to cardiovascular disease observed in Spain relative to that of several other European countries.
Although cardiovascular diseases are among the most widely researched pathologies, the availability and quality of the information required to calculate DALYs are limited. With regard to the mortality data, a considerable percentage of deaths are assigned to poorly defined codes, among them, the code for heart failure.41 In an effort to provide a complete estimation of DALYs due to ischemic heart disease, we identified deaths assigned to code I50 and attributed a percentage of them to ischemic heart disease. The percentage to be applied was estimated from data reported in a clinical study, as we found no mortality studies that provided this information. Thus, the contribution of heart failure may have been overestimated.
Another potential limitation is related to the availability of updated data on the incidence and prevalence of stable angina.42 Use of the Spanish Minimum Basic Data Set as the source for the prevalence of stable angina may have led to underestimation of the related YLDs because cases that were never hospitalized would not have been included. Nonetheless, we believe that the magnitude of this difference would not be very large in terms of YLD, since cases that go undetected would be mild ones, and would be assigned a low disability weight. A relatively simple way to obtain data on the prevalence of stable angina in Spain would be to include the complete Rose questionnaire in the National Health Survey.
As to heart failure, one of the main limitations in the studies identified was the lack of information on etiology and levels of severity broken down by age and sex. In this regard, the actual differences by sex and age might be larger than those reflected in our results, since we applied the same distribution by etiology and severity in all the age groups.
CONCLUSIONSDespite significant advances in ACS treatment and the knowledge acquired on cardiovascular risk factors and their control, ischemic heart disease continues to have a major impact on the health of our population, particularly in terms of mortality. These results signal the need to enhance primary preventive measures, as well as secondary prevention and treatment for ACS and its chronic sequelae, especially heart failure.
This study underscores the need to strengthen and promote epidemiological research in ischemic heart disease. National population studies that take into account factors such as age and sex will provide accurate data on the epidemiology of angina and heart failure, and more detailed and updated data on the epidemiology of ischemic heart disease in its various manifestations.
The findings presented here could be used as the basis to study the cost-effectiveness of preventive or therapeutic interventions, to estimate the burden of disease attributable to cardiovascular risk factors, to analyze changes in the burden of ischemic heart disease over time or compare this burden with that of other diseases, and to help establish priorities in interventions to improve the health of our population.
FUNDINGThis study was funded by the PS09/00086 project, integrated in the Plan Estatal de I+D+I (2008-2011), and co-funded by the Carlos III Institute of Health (ISCIII) Deputy General Directorate for Evaluation and Promotion of Research, and the European Regional Development Fund (ERDF).
CONFLICTS OF INTERESTNone declared.
The authors thank Eva Andres for the data and clarifications provided regarding one of the studies rated as a source of information on the incidence of acute myocardial infarction.