To the Editor,
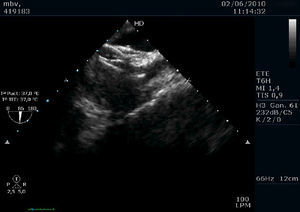
A 58-year-old woman with history of cerebral aneurysm that was embolized 1 year earlier, with no cardiovascular risk factors, was admitted to the hospital with aphasia and hemiparesis due to a cerebral infarction in the left middle cerebral artery. In a transthoracic echocardiography with saline, a moderate tendency of microcavitations in the left atrial was observed, with interatrial septum intact and no structural anomalies. A transesophageal echocardiogram (TEE) demonstrated a hypermobile, >11mm-bulging membrane at the oval fossa that was becoming detached in the anterior segments, and a prominent Eustachian valve directing flow towards it. The patient was referred for percutaneous closure of the patent foramen ovale (PFO) and was treated with 300mg acetylsalicylic acid. Non-fractionated heparin was administered preoperatively at 6000 UI. A 35mm-Amplatzer device was implanted under general anaesthesia using a TEE-guided right femoral approach (before and during the apposition and release of the occluder). No initial complications were produced during this brief procedure. After releasing the device, we observed a hypermobile filiform image in the left atrial face (Figure 1) that would correspond to a thrombus, but which did not cause incorrect disc apposition. We administered an additional 7500 UI non-fractionated heparin and treatment was started with 100mg acetylsalicylic acid, 75mg clopidogrel, and therapeutic doses of enoxaparin. The patient stayed in the hospital for 1 week, with no new neurological symptoms or hemorrhagic events associated with the treatment; TEE imaging showed no thrombi and that the occluder was functioning correctly (Figure 2). Given the patient's history of cerebral aneurysm and the close association between thrombi and this procedure, the patient was discharged with only double anti-aggregation therapy. The clinical follow-up at 4 months was satisfactory.
Figure 1. Filiform image in the atrial face of the left disc that corresponds to a thrombus.
Figure 2. Good apposition of a double disc device, with no images of thrombi.
The prevalence of PFO in patients with a history of stroke ranges between 20% and 40%, and the estimated annual rate of recurrent ictus among PFO patients ranges between 1.5% and 12%, depending on the population studied.1 The optimal treatment for preventing strokes in PFO patients has not been identified. The international clinical practice guidelines recommend antiplatelet aggregation treatment for patients with transient ischemic attack and PFO, although it also could be indicated as an anticoagulant in other situations, such as atrial fibrillation: “[…] insufficient data exists […] regarding the use of percutaneous closing devices for PFO in patients with their first ictus; this strategy could be considered for those patients who have suffered repeated cryptogenic strokes in spite of medical treatment.”2, 3
During the percutaneous closure of a PFO, the total incidence of device thrombosis is small, varies according to the study, and also depends on the type of occluder used. In the Krumsdorf4 series (with 1000 patients [593 PFO and 407 with atrial septal defects] and TEE used during the procedure and at 4-week follow-up), the total rate was 6%. In the TEE study after 4 weeks, no thrombi were found in the 292 cases involving an Amplatzer occluder, 1 (1%) in 161 Helex devices, 3 (7%) in 127 PFO-Star devices, and 7 (7%) in 100 CardioSEALs. Although the incidence was low, the best predictors for the thrombi formation were the presence of persistent atrial fibrillation and ASA. No increased benefit was observed when treating patients with a combination of aspirin and clopidogrel with respect to the group that received only aspirin as a thrombosis prophylaxis treatment. In general, thrombus was resolved through medical treatment in 17 of 20 patients within 4 weeks to 6 months (warfarin and/or heparin); in 3, a surgical extraction of the thrombus was required.
This case illustrates the usefulness of TEE during percutaneous structural procedures, as well as the need for intensive anti-aggregant and anti-coagulant treatment in order to avoid complications in patients with thrombi.
Corresponding author: eduardo.lezcano@gmail.com